Archive for February, 2022
[ABSTRACT] Brain Stimulation Using Responsive Neurostimulation Improves Verbal Memory: A Crossover Case–Control Study
Posted by Kostas Pantremenos in Epilepsy, TBI on February 28, 2022
Abstract
BACKGROUND:
The effects of brain stimulation on memory formation in humans have shown conflicting results in previous studies. We hypothesized that direct cortical stimulation using an implanted responsive neurostimulation (RNS) system will improve memory.
OBJECTIVE:
To evaluate whether direct cortical stimulation using RNS improves memory as measured with recall scores of a list-learning task.
METHODS:
During outpatient visits, a list-learning task (Hopkins Verbal Learning Test-Revised) was administered to 17 patients with RNS implants. Patients were read a list of 12 semantically related words and asked to recall the list after 3 different learning trials. True or sham stimulations were performed for every third word presented for immediate recall. Most patients had frontotemporal network stimulation—one patient each had insular and parietal stimulations. After a 20-min delay, they were asked to recall the list again, first freely and then through a “yes/no” recognition paradigm. A crossover design was used in which half the patients had true stimulation during the initial visit and half had sham stimulation—followed by crossover to the other group at the next visit.
RESULTS:
The Hopkins Verbal Learning Test–Revised delayed recall raw score was higher for the stimulation condition compared with the nonstimulation condition (paired t-test, P = .04, effect size d = 0.627).
CONCLUSION:
Verbal memory improves by direct cortical stimulation during a list-learning task. The RNS system can be effectively used in memory research using direct cortical stimulation. This study has implications in the development of neurostimulation devices for cognitive enhancement in conditions such as epilepsy, dementia, and traumatic brain injury.
[REVIEW] The emerging role of virtual reality training in rehabilitation
Posted by Kostas Pantremenos in Video Games/Exergames, Virtual reality rehabilitation on February 27, 2022
Abstract
Virtual reality (VR) uses computer-generated simulations to create a virtual environment for users which appears, sounds, and feels like real-life objects and events. The use of VR in rehabilitation is relatively new and has demonstrated to be an effective tool in achieving desired clinical outcomes by active engagement of participants. Over the past few years, the use of VR in rehabilitation has rapidly increased because of its advantages over traditional rehabilitation techniques. These include better patient adherence to the rehabilitation protocols with high levels of engagement and motivation. This review summarises the available evidence on the role of VR in rehabilitation, its effects, and scope across different clinical conditions and outcomes. We also describe the current status of VR utilization in rehabilitation settings across Pakistan and highlight the need for further research.
Introduction
Virtual reality (VR) uses a computer-generated simulated three-dimensional environment to provide a virtual world to the user with seemingly real images and sounds. It provides an interactive environment where participants can visualize, communicate and manipulate with computer-generated illusions, ultimately enhancing their learning for different outcomes.1 In the past two decades, the use of VR in rehabilitation has increased among healthcare professionals to provide maximum support and quality care to the community.
Types of virtual reality
There are three primary types of virtual reality simulation.
1. Immersive virtual reality provides a fully immersive experience of the virtual or non-physical world to the participant involving equipment such as VR glasses, a head-mounted display, headphones, gloves, and possibly a treadmill. This type of VR provides the most realistic simulation environment to the participant who feels a part of the virtual world. This is most commonly used for gaming and entertainment.2
2. Semi-immersive virtual reality is based on interaction with a partial virtual environment using a screen, displaying real images instead of an avatar in the virtual environment. While it immerses the participants into a different reality, it also allows them to stay connected with their actual surroundings outside the virtual world. Compared to immersive VR, it has fewer side effects such as cybersickness (dizziness and vomiting) and therefore, it is the most commonly used type of VR in rehabilitation practice.2
3. Non-immersive virtual reality is based on traditional illustrations with a computer-generated environment with no immersion into the virtual world. Body and gadgets are separate, and the user stays fully connected with their physical environment. Non-immersive VR systems make use of equipment such as digital screens, game consoles, keyboards, mouse and controllers.2
Use of virtual reality in rehabilitation
VR has been widely used in healthcare, including medical training, patient treatment, telemedicine, disease awareness programmes, and medical marketing. The use of VR is now increasingly common among rehabilitation professionals because of its several advantages over traditional rehabilitation techniques. These include but are not limited to assessment in a more naturalistic environment, safe evaluation of potentially dangerous situations, dual-task assessment, consistency in assessments, better outcome measurements and training protocols, high patient motivation, engagement, and participation.3 VR also helps overcome the challenges associated with physical, supervised, and person-specific training, which can be expensive, physically exhausting for professionals, time-consuming, and does not meet certain repetition (therapy dose) requirements such as in neurological deficits for neuro-plasticity. In contrast, VR provides easy access to home-based activities, promotes independent and active participation of patients, thereby increasing the repetitions and adherence to the rehabilitation programmes.3
Howard (2017) reported that VR rehabilitation programmes are more effective than conventional rehabilitation programmes for the improvement in physical outcomes.4 They proposed three mechanisms for these better outcomes; increased excitement, increased physical fidelity, and cognitive fidelity. Physical fidelity refers to the degree to which a virtual environment appears and sounds real, while cognitive fidelity refers to how a simulator involves the user in cognitive activities used in the real world.4
VR is widely used in various fields of rehabilitation and has shown promising effects in health outcomes.
Neurological rehabilitation
VR has been successfully used in different neurological conditions like brain and spinal cord injury, cerebral palsy, Parkinson’s disease, attention deficit hyperactivity disorder, dyslexia, multiple sclerosis, and focal epilepsy. VR programmes mainly target motor control, posture, balance, movement disorders, strength and endurance in these conditions and it has shown more potential for improvement than the traditional rehabilitation interventions.5
Musculoskeletal rehabilitation
VR has also been used in various musculoskeletal conditions such as osteoarthritis, rheumatoid arthritis, post total knee arthroplasty, chronic low back pain, cervical pain, adhesive capsulitis, and fibromyalgia. The primary outcomes in these conditions are endurance, strength, and functional impairments. A systematic review reported significant positive effects of VR in chronic neck pain, shoulder impingement syndrome, rheumatoid arthritis, knee osteoarthritis, ankle sprains, and cruciate ligament reconstruction; however, the evidence on effects of VR in fibromyalgia, back pain, and knee arthroplasty was inconclusive.6
Cardiopulmonary rehabilitation
VR has shown significant improvements in cardiovascular conditions such as coronary artery disease, stable heart failure, coronary artery revascularization, valve replacement surgeries, angioplasty, cardiomyopathy, prehypertension and other cardiac pathologies and pulmonary conditions like chronic obstructive pulmonary disease. The use of VR improved endurance, functional performance, pain and ability to walk, energy expenditure, high-density lipoprotein cholesterol, body composition, and quality of life in patients with cardiopulmonary diseases.7
Sports rehabilitation
VR has been used as a training tool for athletes and other sports professionals. A VR-based training in sports has several benefits such as supporting athletes to train (cycling, walking, weightlifting, rowing, and running) irrespective of weather situations, geographical variation to compete with other athletes and allowing accurate and replicable control over features of the virtual environment.8
Psychosocial rehabilitation
VR based interventions have been successfully utilized for the management of anxiety disorders, depression, psychosis, bipolar disorder, substance disorders, eating disorders, phobias, stress, post-traumatic stress disorder and schizophrenia.9
Specific clinical outcomes addressed by virtual reality
The clinical outcomes that the rehabilitation professionals can potentially target through VR in different conditions include but are not limited to motor control, balance, gait, strength, pain control, improved physical endurance, mental well-being, reduced fatigue, and better cognition.
1. Motor control: VR provides a specific enriched environment to re-learn motor skills and tasks through repetitive training, task specificity, problem-solving, and experience stimulating neural plasticity in neurological deficits like stroke, brain injury and multiple sclerosis.10
2. Balance: VR provides multi-sensory feedback through virtual environments and offers audio-visual cues, generating synaptic activities and improving collateral networks within the brain to enhance the patient’s balance abilities.11 VR has demonstrated beneficial effects in improving balance in stroke, Parkinson’s disease, multiple sclerosis, cerebral palsy, and traumatic brain injury.12
3. Gait and walking abilities: VR provides a dynamic set of tasks where weight shift, body movements, small steps, reactive balance, and objective progression during the VR experience improve locomotor abilities. VR significantly improved the walking speed, distance covered and the number of steps per day.12
4. Strength: The exact mechanism of how VR improves muscular strength is unclear. However, VR has a diverse set of applications and can change a simple task to a complex activity based on the user’s ability and provides a natural environment for intense activities, ultimately improving strength. In a 2015 study patients with Parkinson’s received task-oriented resistance training incorporated in a virtual environment such as heel raise, squats, and stepping resulting in significant improvement in muscle strength and walking ability.13
5. Pain: The current evidence supports use of VR as a valuable pain distraction intervention with minimal side effects. A systematic review showed that VR experience was an effective non-pharmacological intervention for individuals experiencing pain from burn injuries or acute or chronic medical procedures.14
6. Fatigue: Fatigue is a debilitating problem for individuals suffering from conditions like stroke, multiple sclerosis, cancer, kidney failure, pulmonary diseases, and autoimmune disorders. A recent systematic review suggested an inverse relationship of VR training with fatigue levels. However, there was limited evidence available, and further studies are needed to make strong inferences.14
7. Cognition: There is evidence to support VR use for cognitive training in individuals suffering from cognitive impairments. Cognitive training aims to maintain or improve higher mental functions like attention, concentration, memory, and problem-solving skills. Zhao et al. (2020) in a systematic review reported that exergaming is beneficial in improving cognitive function in people with dementia or mild cognitive impairments. The proposed underlying mechanism could the rich environment provided by VR games which stimulates brain functioning.15
The use of Virtual reality rehabilitation in Pakistan
Although VR rehabilitation is being used in the USA and Europe for more than 2 decades, it is relatively a newer rehabilitation tool in Pakistan. Only few centers have the VR rehabilitation set-up, and all are in the major cities of Pakistan. However, the research on the use of VR in rehabilitation has increased in the last few years. A literature search in August 2021, revealed 14 published research studies on the use of VR in rehabilitation in Pakistan. The most common VR device used was X-box Kinect 360. Most studies suggested that VR is an effective tool compared to the traditional exercise programmes in terms of goal attainment, motivation, and engagement. All studies demonstrated beneficial effects of VR; however, most studies were either limited to the elderly population or neurological conditions only targeting balance, mobility, and function. In addition, many studies lacked statistical power and used a weak experimental research design. Future studies with larger sample sizes targeting other conditions and outcomes with stronger research designs are needed to make better conclusions about the scope of VR rehabilitation in Pakistan
Conclusion:
The current literature supports the use of VR as an innovative, engaging, and cost-effective tool for rehabilitation professionals. It has been successfully used in many neurological, cardiopulmonary, and musculoskeletal disorders with good outcomes. It has certain advantages over the traditional rehabilitation interventions which should be considered while making a rehabilitation plan. The research and use of VR rehabilitation is increasing in Pakistan and there is a need to improve the quality of research in order to generate high quality evidence.
References
1. Cameirão MS, Badia SB, Oller ED, Verschure PF. Neurorehabilitation using the virtual reality based Rehabilitation Gaming System: methodology, design, psychometrics, usability and validation. J Neuroeng Rehabil. 2010;7:48. doi: 10.1186/1743-0003-7-48.
2. Nadeem A. Virtual Reality Educational Transforms and Prospect for Pakistan. Muslim Perspectives 2019;4:79-101. Retrieved August 8, 2021. Available from https://www.muslim-perspectives.com/ Publication-Detail?publication=92/Virtual-Reality-Educational-Transforms-and-Prospect-for-Pakistan
3. Burke T, Rooney B. Multi-Modal Dual-Task Measurement: A New Virtual Reality for Assessment. Front Psychol. 2021;11:635413. doi: 10.3389/fpsyg.2020.635413.
4. Howard MC. A meta-analysis and systematic literature review of virtual reality rehabilitation programs. Comput Hum Behav 2017;70:317-27. https://doi.org/https://doi.org/10.1016/j.chb.2017. 01.013
5. Kachmar O, Kushnir A, Fedchyshyn B, Cristiano J, O’Flaherty J, Helland K, Johnson G, Puig D. Personalized balance games for children with cerebral palsy: A pilot study. J Pediatr Rehabil Med. 2021;14: 237-245. doi: 10.3233/PRM-190666.
6. Gumaa M, Rehan Youssef A. Is Virtual Reality Effective in Orthopedic Rehabilitation? A Systematic Review and Meta-Analysis. Phys Ther. 2019; 99: 1304-1325. doi: 10.1093/ptj/pzz093.
7. García-Bravo S, Cuesta-Gómez A, Campuzano-Ruiz R, López-Navas MJ, Domínguez-Paniagua J, Araújo-Narváez A et al. Virtual reality and video games in cardiac rehabilitation programs. A systematic review. Disabil Rehabil. 2021 ;43(4):448-457. doi: 10.1080/09638288.2019. 1631892.
8. Neumann DL, Moffitt RL, Thomas PR, Loveday K, Watling DP, Lombard CL, Antonova S, Tremeer MA. A systematic review of the application of interactive virtual reality to sport. Virtual Reality. 2018;22:183-98.
9. Siani A, Marley SA. Impact of the recreational use of virtual reality on physical and mental wellbeing during the Covid-19 lockdown. Health Technol (Berl). 2021 14:1-11. doi: 10.1007/s12553-021-00528-8.
10. Levin MF, Weiss PL, Keshner EA. Emergence of virtual reality as a tool for upper limb rehabilitation: incorporation of motor control and motor learning principles. Phys Ther. 2015;95:415-25. doi: 10.2522/ptj.20130579.
11. Syed UE, Kamal A. Video game-based and conventional therapies in patients of neurological deficits: an experimental study. Disabil Rehabil Assist Technol. 2021 ;16:332-339. doi: 10.1080/17483107. 2019.1679266..
12. Cano Porras D, Siemonsma P, Inzelberg R, Zeilig G, Plotnik M. Advantages of virtual reality in the rehabilitation of balance and gait: Systematic review. Neurology. 2018 ;90:1017-1025. doi: 10.1212/WNL.0000000000005603.
13. Liao YY, Yang YR, Wu YR, Wang RY. Virtual reality-based Wii fit training in improving muscle strength, sensory integration ability, and walking abilities in patients with Parkinson’s disease: a randomized control trial. Int J Gerontol. 2015 1;9:190-5.
14. Ioannou A, Papastavrou E, Avraamides MN, Charalambous A. Virtual Reality and Symptoms Management of Anxiety, Depression, Fatigue, and Pain: A Systematic Review. SAGE Open Nurs. 2020;6:2377960820936163. doi: 10.1177/2377960820936163.
15. Zhao Y, Feng H, Wu X, Du Y, Yang X, Hu M, Ning H, Liao L, Chen H, Zhao Y. Effectiveness of Exergaming in Improving Cognitive and Physical Function in People With Mild Cognitive Impairment or Dementia: Systematic Review. JMIR Serious Games. 2020;8:e16841. doi: 10.2196/16841.
[ARTICLE] Rhythm and Music-Based Interventions in Motor Rehabilitation: Current Evidence and Future Perspectives – Full Text
Posted by Kostas Pantremenos in Music/Music therapy on February 27, 2022
Abstract
Research in basic and clinical neuroscience of music conducted over the past decades has begun to uncover music’s high potential as a tool for rehabilitation. Advances in our understanding of how music engages parallel brain networks underpinning sensory and motor processes, arousal, reward, and affective regulation, have laid a sound neuroscientific foundation for the development of theory-driven music interventions that have been systematically tested in clinical settings. Of particular significance in the context of motor rehabilitation is the notion that musical rhythms can entrain movement patterns in patients with movement-related disorders, serving as a continuous time reference that can help regulate movement timing and pace. To date, a significant number of clinical and experimental studies have tested the application of rhythm- and music-based interventions to improve motor functions following central nervous injury and/or degeneration. The goal of this review is to appraise the current state of knowledge on the effectiveness of music and rhythm to modulate movement spatiotemporal patterns and restore motor function. By organizing and providing a critical appraisal of a large body of research, we hope to provide a revised framework for future research on the effectiveness of rhythm- and music-based interventions to restore and (re)train motor function.
Introduction
Brain and clinical research conducted over the past 25 years have provided a new understanding of the capabilities of music to engage and shape non-musical perceptual, cognitive, language, and motor functions to effectively support brain recovery processes (Thaut, 2010; Koshimori and Thaut, 2018, 2019; Altenmüller and James, 2020; Thaut and Koshimori, 2020; Chatterjee et al., 2021). In the context of motor rehabilitation, the finding that musical rhythm entrains movement in patients with neurological disorders opened new frontiers for the use of rhythm and music as a continuous time reference to prime the motor system and re-program the execution of movement patterns (Thaut et al., 1996, 2015).
Music is a potent driving force for movement. Synchronization of body movements to external rhythmic auditory stimuli, such as music or a metronome, is possible because the regular and predictable rhythmic structure of the music is readily and precisely detected by the auditory system, inducing entrainment of neuronal activity in auditory and motor regions of the brain involved in rhythm perception and movement production (Thaut et al., 2015; Damm et al., 2020). Growing experimental evidence of the effect of rhythmic entrainment on movement spatiotemporal patterns and the current advances of the neural underpinnings of auditory-motor coupling have informed the development of theory-driven interventions that have been tested in a large number of studies.
In this paper, we review recent studies focusing on four evidence-based interventions using rhythm and active music playing to improve motor functions following central nervous injury and/or degeneration: respectively, Rhythmic Auditory Stimulation, and Music-supported Therapy, Therapeutic Instrumental Music Performance, and Patterned Sensory Enhancement (Table 1). This paper aims to provide a critical narrative review of the current literature on the effects of rhythm- and music-based interventions for motor rehabilitation in a wide range of clinical populations (e.g., Parkinson’s Disease, stroke, cerebral palsy, traumatic brain injury, and multiple sclerosis) as well as aging. Additionally, considering that evidenced-based practices are built on ongoing fundamental brain research and theories, we briefly overview recent neurophysiological and neuroimaging evidence of the potential mechanisms underlying the effectiveness of rhythm and music in shaping movement timing and control. To finalize, we highlight research questions and methodological concerns that should be on the agenda for future research. By organizing and providing a critical appraisal of a large body of research, we hope to provide a revised framework for future research on the effectiveness of rhythm- and music-based interventions to restore and (re)train motor function.[…]
[Abstract] Effects of proprioceptive training for people with stroke: A meta-analysis of randomized controlled trials
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop on February 27, 2022
Abstract
Objective
To evaluate the effectiveness of proprioceptive training on balance performance, trunk control, and gait speed in people with stroke.
Methods
We searched PubMed, Science Direct, Cochrane, Embase, and Medline for randomized controlled trials that evaluated the effects of proprioceptive training for patients with stroke from the date of each database’s inception to July 26, 2021. Two reviewers independently screened the titles and abstracts of potentially eligible articles that were identified on the basis of the search criteria. Methodological quality was determined using version 2 of the Cochrane risk of bias tool for randomized trials. Data were analyzed using Comprehensive Meta-Analysis software. The treatment effect was estimated by calculating Hedges’ g and 95% confidence intervals (CIs) using a random-effects model. Statistical heterogeneity was assessed according to the I2 value. The primary outcome was balance performance and secondary outcomes were trunk control, gait speed, and basic functional mobility.
Results
In total, 17 trials involving 447 people with stroke were included. Proprioceptive training had a significant effect on balance performance (Hedges’ g = 0.69, 95% CI = 0.36–1.01), gait speed (Hedges’ g = 0.57, 95% CI = 0.19–0.94), trunk control (Hedges’ g = 0.75, 95% CI = 0.33–1.17), and basic functional mobility (Hedges’ g = 0.63, 95% CI = 0.31–0.94) among people with stroke.
Conclusion
Proprioceptive training may be effective in improving balance performance, gait speed, trunk control, and basic functional mobility among people with stroke.
[Infographic] Mental Illness: What People See Versus What is Actually Happening
Posted by Kostas Pantremenos in Cognitive Rehabilitation on February 27, 2022

[REVIEW[ Neurological Immune‐Related Adverse Events After COVID‐19 Vaccination: A Systematic Review – Full Text
Posted by Kostas Pantremenos in COVID-19 on February 27, 2022
Abstract
The coronavirus disease 2019 (COVID-19) pandemic has affected millions of individuals worldwide. The global scientific effort to design an effective vaccine against this virus has led to the development of several vaccine candidates. The expedited rollout of these vaccines has created some public distrust regarding the safety of these new vaccines. This review compiles clinical data from reports of diagnosed immune-related neurological events that have occurred after COVID-19 vaccine administration with the exception of those secondary to hematological abnormalities. A systematic literature search was performed, using several databases, to identify reports of postvaccination adverse neurological events. The search resulted in 18 studies that met our criteria. These studies included 61 patients who had received COVID-19 vaccines and experienced at least 1 neurological adverse effect. The most common neurological event was facial nerve palsy (50% of all events). Other less frequently reported events included the reactivation of herpes zoster, Guillain-Barre syndrome, other demyelinating diseases, and neuropathy. The underlying mechanism was hypothesized to be related to vaccine-induced type 1 interferon production leading to decreased tolerance of the myelin sheath antigens. Other hypotheses include vaccine-induced transient lymphopenia and immune dysregulation. Most of the reported events were time limited and resolved spontaneously. Given the rarity of reported neurological events compared to the total number of vaccines administered, and the similarity in the incidence of events between COVID-19 vaccines and other more common vaccines, there is little evidence to support a causal relationship between COVID-19 vaccines and adverse neurological events.
The novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) became a cause of global alarm in 2019. The severe respiratory disease first seen in the Wuhan district of China spread across the world at an extraordinary rate leading to the declaration of coronavirus disease 2019 (COVID-19) as a pandemic. As of November 26, 2021, there have been 259 million reported COVID-19 cases with >5 million deaths reported worldwide according to the World Health Organization (WHO).1 The impact of the pandemic on the worldwide economy, morbidity, and mortality has led to unprecedented collaboration in scientific research across the global scientific community to establish diagnostic and therapeutic modalities to help curb the pandemic. Perhaps the most remarkable development is the creation of efficacious vaccines against the virus in record time. This haste in scientific research, vaccine production, and rollout has led to a widespread discussion on whether the progression in research has come at the cost of compromising safety standards.
Several hundred vaccines have been under development since the start of the pandemic, with over 60 having reached the stage of clinical trials.2 Late 2020 witnessed the rapid approval and rollout of several vaccines such as the Pfizer-BioNTech, Moderna, and Oxford-AstraZeneca, with >3.4 billion vaccine doses administered since then.1
Pfizer-BioNTech Vaccine
The Pfizer-BioNTech or BNT162b2 COVID-19 vaccine is a lipid nanoparticle–formulated mRNA vaccine that was the first vaccine to be authorized and rolled out in the Western Hemisphere. It consists of the raw material encoding the SARS-CoV-2 spike glycoprotein.3 The Food and Drug Administration (FDA) authorized the vaccine for emergency use on December 11, 2020.4 The vaccine consists of 2 doses of intramuscular injections that are administered 3 weeks apart.4 More than 114 countries have approved the use of the BNT162b2 vaccine, with the rollout of the vaccine first beginning in early December in the United Kingdom.5 More than 700 million doses of the BNT162b2 vaccine had been administered as of May 2021.6
Moderna Vaccine
The Moderna or mRNA-1273 COVID-19 vaccine is a mRNA vaccine that codes for the prefusion spike protein.7 It was authorized for emergency use by the FDA on December 18, 2020.8 Several countries including the United States, Singapore, and the European Union have authorized the use of the vaccine.8 It consists of 2 doses of intramuscular injections that are administered (100 μg, 0.5 mL each) 4 weeks apart.4 In January 2021, Moderna announced starting a phase 1 clinical trial for a newer vaccine (mRNA-1273.351) against the beta variant known as B.1.351 first identified in South Africa.9
Oxford-AstraZeneca COVID-19 Vaccine
The Oxford-AstraZeneca or AZD1222 COVID-19 vaccine consists of the spike protein genetic sequence carried by an adenovirus vaccine vector. The same vaccine is also manufactured by the Serum Institute of India under the name of “Covishield.”10 The vaccine is shown to be effective against the alpha (lineage B.1.1.7) and the delta (lineage B.1.617.2) variants.11, 12 It was first authorized in the United Kingdom on December 30, 2020, and has been approved in more than 170 countries.13 The vaccine consists of 2 intramuscular doses of 0.5 mL each (2.2 × 1010 viral particles per dose) administered 8 to 12 weeks apart,14 with rollout beginning on January 4, 2021.15 Reports of a rare blood clot disorder associated with the vaccine resulted in the temporary halting of its use in many countries. Since then, the vaccine has been recontinued in most countries, as the side effects were found to be very rare in relation to its general efficacy.16
Sinopharm
The Sinopharm/BIBP COVID-19 vaccine consists of inactivated SARS-CoV-2 virus.17 It was first authorized for use on December 31, 2020, by the China National Medical Products Administration, with its rollout starting immediately.18 On May 7, 2021, months after the vaccine had been in use in several countries across the world, the vaccine was approved for emergency use by the WHO.18 It is an intramuscular vaccine with 2 doses administered 3 to 4 weeks apart.18 It has been in use in over 40 countries with almost 65 million doses administered globally up to June 2021.18
Sputnik V
The Sputnik V/Gam-COVID-Vac COVID-19 vaccine was developed by Gamaleya Research Institute of Epidemiology and Microbiology in Russia. It was the world’s first vaccine developed against COVID-19 and was registered by the Russian Ministry of Health on August 11, 2020.19 It consists of 2 doses, each with a different adenovirus-based viral vector (serotypes 26 and 5), that code for the SARS-CoV-2 spike protein to generate immunity against the virus. Each dose contains (1.0 ± 0.5) × 1011 gene particles administered 21 days apart.20 On July 9, 2021, the Russian Direct Investment Fund said that the vaccine remains effective even if the gap between the doses is extended to 180 days.21 It has been approved in 67 countries, including Brazil, Hungary, India, and the Philippines.22 It is yet to be approved by the European Medicines Agency or WHO however, as there are concerns with the lack of transparent safety and efficacy surveillance data.
Johnson & Johnson
The Janssen COVID-19 vaccine or the Johnson & Johnson COVID-19 vaccine was developed by Janssen Vaccines, Netherlands.23 It consists of a recombinant adenovirus type 26 vector expressing the SARS-CoV-2 spike protein.24 It consists of a single dose of 0.5 mL, which is administered intramuscularly.25 The FDA approved its use on February 28, 2021, with rollout in the United States beginning 2 days later.26 The WHO approved its emergency use on March 12, 2021, with approved use in several countries across Europe, Asia, and the Americas. As of May 2021, >8 million doses of the Janssen COVID-19 vaccine had been administered in the United States alone.25
Several studies were conducted to assess the efficacy/effectiveness and safety of the COVID-19 vaccines. The BNT162b2 vaccine was found to be 95% efficacious, while the mRNA-1273 vaccine trials showed an efficacy of 94.1%. The AZD1222 vaccine has been shown to have 70.4% efficacy following 2 doses.27 With the emergence of new variants, the long-term efficacy of the vaccines has been brought into question. A recent study found that BNT162b2-induced protection against SARS-CoV-2 infection waned rapidly following its peak after the second dose.28 In response, many countries are starting to administer booster doses 6 months after receiving the primary vaccination series.29
There is a consensus in the scientific community of the success of these vaccines in combating COVID-19; however, the reporting of side effects associated with their use has led to vaccine hesitancy in the general population. The US FDA Center for Biologics Evaluation and Research published a protocol on the background rates of Adverse Events of Special Interest for COVID-19 vaccine safety monitoring. Many side effects were listed as an outcome of COVID-19 vaccination, including acute myocardial infarction, anaphylaxis, appendicitis, Bell’s palsy, deep vein thrombosis, disseminated intravascular coagulation, encephalomyelitis, Guillain-Barre syndrome (GBS), hemorrhagic and nonhemorrhagic stroke, immune thrombocytopenia, myocarditis/pericarditis, narcolepsy, pulmonary embolism, and transverse myelitis.30
This review compiles data about the diagnosed adverse immune-related neurological events reported after COVID-19 vaccination, with the exception of those secondary to hematological abnormalities like thrombosis or hemorrhage. The possible mechanisms for the vaccines to induce these events are discussed. This may help increase awareness about the possible incidence of such rare events and their outcome.[…]

[WEB] EXCLUSIVE: Three assistive technology modifications in electric vehicles to help drivers with disabilities
Posted by Kostas Pantremenos in Assistive Technology on February 27, 2022
by Sarah Sarsby

In this article, Jessica Pierce, Content Producer and Researcher from The Sixth Degree, explores three assistive technology modifications in electric vehicles to help drivers with disabilities.
Driving can be a key component of remaining independent for many people, especially those with disabilities. A car can allow you to go out and get your own food, meet friends, and visit new places, which can be especially crucial for those who live in more rural areas. Even for those that live in cities, public transportation is not always the most convenient or accessible.
However, driving a standard car can be difficult for someone with a disability, as they require moving multiple components, often quickly and smoothly. Although automatic cars are somewhat easier than manual vehicles, they can still be challenging. Luckily, modern technology has led to the invention of some amazing modifications that give those with limited mobility the chance to stay on the road.
Remember that in the UK, you are legally required to report any disabilities or health conditions that affect your driving to the DVLA. They will then assess if you can continue to drive, and if they recommend an adapted vehicle, you’ll need to complete a driving assessment. They can then discuss which adaptations might suit you best.
Here, we look at three of the most common adjustments that you might hear about.
Hand controls
One of the key parts of being able to retain your driving licence is being able to brake and accelerate safely and consistently. If a driver struggles to keep control of their lower body mobility, or has lost this mobility, the car can be driven using hand controls to brake and accelerate.
There are several options for this. The most common one is a push and pull lever, where the driver pushes the lever away to brake and pulls it towards them to accelerate. Doing this manually operates the pedals in the footwell of the car. They can either be fitted to the floor with a longer stick or a short stick which is attached to the steering column, and they work best with an automatic car.
Electronic accelerators
Of course, a hand control lever also requires strength and coordination to control. But lacking the strength to pull a lever doesn’t mean that you can’t drive. There are plenty of acceleration options for those who would benefit from an electronic tool, which are then paired with a braking tool (these do tend to be mechanical, but there are electronic options available).
Plenty of these tools are also very discreet, so there are no chunky additions to your sleek vehicle. Ring accelerators can either be placed in front of or behind the steering wheel, so that you push or pull the ring in order to go faster. You can also get a ghost ring accelerator, which sits behind the steering wheel and the driver controls the speed by moving the ring side-to-side.
Steering aids
Steering wheels can be heavy and awkward to turn for those with disabilities. Steering aids are aimed at making turning the wheel easier for the driver, allowing them to rotate the wheel with only one arm. The most common types are standard fixed and standard quick release. They are both ‘ball and mushroom’ style additions to the wheel allowing the driver to control the vehicle with just one hand rather than two.
The quick-release option allows you to remove this easily from the steering wheel, which can be really helpful for disabled drivers who share a car with a non-disabled driver.
[Abstract] The use of rhythmic auditory stimulation for functional gait disorder: A case report
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, Music/Music therapy on February 26, 2022
Abstract
Background: Functional gait disorders (FGD) are a common and disabling condition. Consensus-based rehabilitation techniques for treating FGD and other functional neurological disorder presentations at large utilize a variety of therapeutic strategies, including distraction, novel approaches to movement, entrainment, stress/hypervigilance modulation, and psychotherapy.
Case report: Here we present a case of a 24-year-old woman with a complex history of anxiety, depression, left frontal astrocytoma, postural orthostatic tachycardia syndrome (POTS) and FGD. During a multidisciplinary inpatient rehabilitation stay for FGD, the patient underwent rhythmic auditory stimulation (RAS) delivered by a neurologic music therapist in conjunction with physical therapy, occupational therapy, and psychotherapy.
Results: The RAS intervention appeared to play a significant role in symptom resolution for this patient. Improvement in the patient’s truncal displacement, foot dragging, and well as overall gait speed occurred following serial RAS trials performed over a single treatment session. Benefits persisted immediately following the intervention and upon subsequent reassessment. Although at four-year follow-up the patient’s FGD symptoms remained resolved, fatigue continued to limit her ambulatory capacity and overall endurance.
Conclusion: RAS represents a unique therapeutic approach for treating FGD, complementary to existing consensus-based rehabilitation recommendations, and may warrant further consideration by the field.
[WEB] Treatment with new innovative Technology – Swiss Medica
Posted by Kostas Pantremenos in REHABILITATION on February 25, 2022
New innovative treatment at Swiss Medica clinic
Discover treatments that have been helping patients facing conditions such as arthritis, diabetes, multiple sclerosis, autism, Parkinson’s and many more hard to treat diseases.
Swiss Medica clinic has been helping patients reclaim their quality of life for 8 years. Headquartered in Switzerland with clinics in Austria, Serbia, Slovenia, and Russia.
What results can you expect from New Innovative treatment?
Find out if this therapy is beneficial for a certain disease, how and why it works, and what the treatment involves.
What diseases can we treat?
The therapy help to eliminate the cause of disorders leading to a reduction in symptoms or a full recovery, depending on the initial condition, for (mostly) autoimmune disorders and/or diseases associated with tissue damage.
There is a large percentage of cases with a variety of diseases that have experienced health improvements. We’ve seen various levels of recovery after treating the following diseases (not a full list):
Neurological disorders
- Multiple Sclerosis
- Parkinson’s disease
- Dementia
- Alzheimer’s disease
- Post-stroke condition
- Injuries of CNS
- Lyme diseas
Endocrine diseases
- Diabetes type 2
- Diabetic foot
- Erectile dysfunction
- Obesit
Musculoskeletal disorders
- Arthritis
- Osteoarthritis
- Sports-related injuries complications
- Athletic performance improvemen
Digestive System Diseases
- Crohn’s disease
- Cirrhosis of the liver
- Peptic ulcer disease
- Chronic pancreatitis
Respiratory diseases
- COPD
- Asthma
- Allergic rhinitis
- Sarcoidosis
Rheumatic diseases
- Systemic scleroderma
- Dermatomyositis
- Rheumatoid arthritis
- Lupus
- Vasculitides
It is important to understand that the treatment is not a guaranteed cure for every disease.The patient may be denied for various reasons. The effectiveness of the therapy for a particular disease depends on multiple factors: duration of the illness, age of the patient, the existence of chronic conditions, hereditary predisposition, lifestyle, etc.
[…]
[ARTICLE] Making Best Use of Home-Based Rehabilitation Robots – Full Text
Posted by Kostas Pantremenos in Rehabilitation robotics, Tele/Home Rehabilitation on February 25, 2022
Abstract
Large-scale clinical trials have shown that rehabilitation robots are as affective as conventional therapy, but the cost-effectiveness is preventing their uptake. This study investigated whether a low-cost rehabilitation robot could be deployed in a home setting for rehabilitation of people recovering from stroke (n = 16) and whether clinical outcome measures correlated well with kinematic measures gathered by the robot. The results support the feasibility of patients independently using the robot with improvement in both clinical measures and kinematic data. We recommend using kinematic data early in an intervention to detect improvement while using a robotic device. The kinematic measures in the assessment task (hits/minute and normalised jerk) adequately pick up changes within a four-week period, thus allowing the rehabilitation regime to be adapted to suit the user’s needs. Estimating the long-term clinical benefit must be explored in future research.
1. Introduction
Complications from neurological disorders may leave patients with physical and/or mental impairments which affect their function in daily activities and quality of life. A consequence of these neurological disorders is often physical weakness, both in the upper and lower limbs. Physiotherapy in the acute stage can be less focused on upper-limb rehabilitation [1] as the use of the lower limbs for mobility is considered of greater importance. Conventional therapy services are resource limited and can be a source of disappointment to participants [2,3]. This is a problem for the patients who are discharged from hospital wards and need to continue to undertake rehabilitation.
Since the early 1990s the use of rehabilitation robotics to aid and administer therapy to participants has been developed [4,5]. Robots can help a patient to complete a task and have been seen to motivate patients using computerised interfaces. Studies have shown that after robot training participants can improve arm function and ability in Activities of Daily Living (ADL) [6,7].
There is a wide range of neurological conditions, but the research described in this paper will focus on adults with stroke. In adulthood, stroke is one of the major causes of disability [8,9]. In the UK alone more than 100,000 people have a stroke each year (currently 1.3 million survivors in the UK) [10] at an estimated cost that exceeds £26 billion per year [11]. The success of rehabilitation can vary on the type of stroke. After hemispheric infraction (obstruction of blood to the brain) about 75% of survivors report weakness in their affected hand making it difficult to perform ADL [12]. Rehabilitation plays a large part in the recovery of stroke participants. However, the type of rehabilitation and choice of intervention play an important role in terms of impact on participant outcomes. Conventional therapy generally involves one-on-one interaction between patient and therapist. The therapist assists and encourages the patient through a number of repetitive movements. The therapy aims at reduction of impairment and improvement of functions for ADL [13].
Novel technologies which assist a person to undertake arm exercise can provide a means of supplementing physical treatments provided through conventional therapy. Increasing the intensity of practice is an important component of recovery, particularly for functionally useful movements [13,14]. There are several devices currently being developed with varying degrees of complexity. Many of these require the system to be used and supervised in a clinical or hospital setting. These devices are intended to be used for patients with moderate to severe arm weakness. However, patients with some good residual function could benefit from using devices which are less complex and allow independent use.
There have been a number of rehabilitation robots that have been developed over the last 30 years, and studies have shown that they have their place [15]. But the devices found in research studies are not suitable for home-based rehabilitation [16], and there are few commercial offerings available.
With the COVID-19 pandemic, the impact on the NHS and patients was devastating. Across Europe, over 50% of patients in the later stages of recovery were refused in-house therapy [17]. Although rehabilitation from stroke is focused on many areas [18], rehabilitation robotics could have played an important factor in home-based rehabilitation. However, the cost–benefit ratio is yet to be explored for robotic therapy en masse. Since 2019, the rehabilitation landscape has changed [19], and this is an opportunity for robots to make a difference—if the price is right [20].
In a recent large-scale study with 770 participants called RATLUS [21], the key findings were that robot therapy is just as useful as conventional therapy but using expensive rehabilitation robotic devices is not a cost-effective solution. The current rehabilitation devices on the market require a therapist to be present, usually in a hospital setting, which reduces the cost-effectiveness of the technology [22].
There are currently no low-cost commercial devices on the market that allow independent robotic rehabilitation in the home. This paper focuses on the potential for robotic rehabilitation in a home setting, and the potential practices for implementation. There have been a number of recent research studies within the home, particularly inspired by the COVID-19 pandemic, that show there is a place for home-based robotics [23,24], and the use of tele-rehabilitation, although it is in its early stages of research [25,26,27].
It has been shown that clinical-based measurements are not accurate enough to pick up small changes but can be combined with kinematic measures for better measurement outcomes [28,29,30]. This paper discusses a number of kinematic measurements that were taken alongside robotic therapy and compared to clinical scales.
Our intervention lasts eight weeks but it has been shown that improvement through rehabilitation can happen over as little as a couple weeks [31]. The paper will discuss what would happen if we halved the time of the intervention, and if the rehabilitation benefit can be maintained.
2. Materials and Methods
This study was a single centre prospective design involving 16 people recovering from stroke. Participants were recruited from the local stroke services who were over 18 years old, had a diagnosis of ischaemic, or hemorrhagic, stroke at least one month prior, had residual strength of the upper limb, and had enough voluntary movement to initiate movement of the joystick. However, participants were not taken on to the study if they had pain in the arm affecting use of the system, had cognitive impairments affecting understanding and capacity to consent, or were medically unstable (e.g., uncontrolled epilepsy).
The clinical exploratory study evaluates the system in people’s homes across an eight-week period with functional clinical assessments at the start, the end, and after a four-week washout period from the end. The washout period allows assessment of any improvement after the robotic study has finished. Clinical assessment measures include the Fugl Meyer (FM) measure, which evaluates recovery after stoke and is a commonly used measure, the Action Research Arm Test (ARAT) which assesses upper limb function using observational methods, the Chedoke Arm and Hand Activity Inventory (CAHAI) which uses a number of functional tasks to assess recovery, the ABILHAND which is another measure of manual ability for upper limb impairment based on interview questions, and the Motor Assessment Scale (MAS) which is an activity observation scale and the Medical Research Council (MRC) scale for muscle strength. The clinical results for this study are fully presented by Sivan et al. [32]. Robotic measures were calculated between start and end of the eight weeks, as the device was used by each participant.
MyPAM (University of Leeds, Leeds, UK) is a bespoke rehabilitation device consisting of a 2D planar robot powered by two DC motors, controlled by National Instruments CompactRIO (National Instruments, Austin, TX, USA) linked to a PC which displays menus and games to the participant. Figure 1 shows the original MyPAM device in a home setting. MyPAM was built using principles of user centred design and design philosophies such as Ulrich and Eppinger’s six-phase product-development process [33] where usability, safety, and functionality are essential.
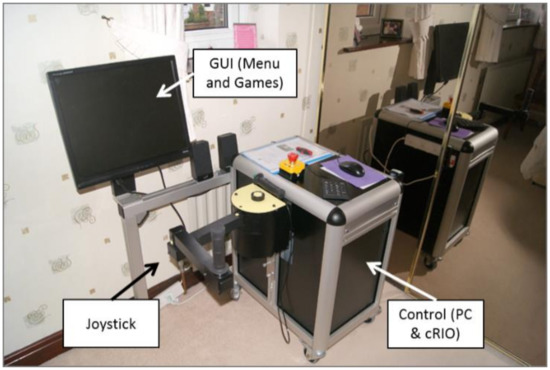
Figure 1. The MyPAM (v1) device in a home setting.
[…]
