Archive for September, 2022
[WEB] What is the Role of Non-invasive Imaging in Diagnostics? – Video
Posted by Kostas Pantremenos in Educational, Radiology/Imaging technology, Video on September 30, 2022
By Dr. Liji Thomas, MD, Reviewed by Aimee Molineux
Introduction
Structural and functional medical imaging
Radiation exposure
Individual techniques
References
Further reading
The use of diagnostic imaging in medicine dates back over a century. However, tremendous advances have been made over the last 50 years, in which multiple imaging modalities have offered a previously unimaginable wealth of data on the structure and function of the inward organs of the human body.

Structural and functional medical imaging
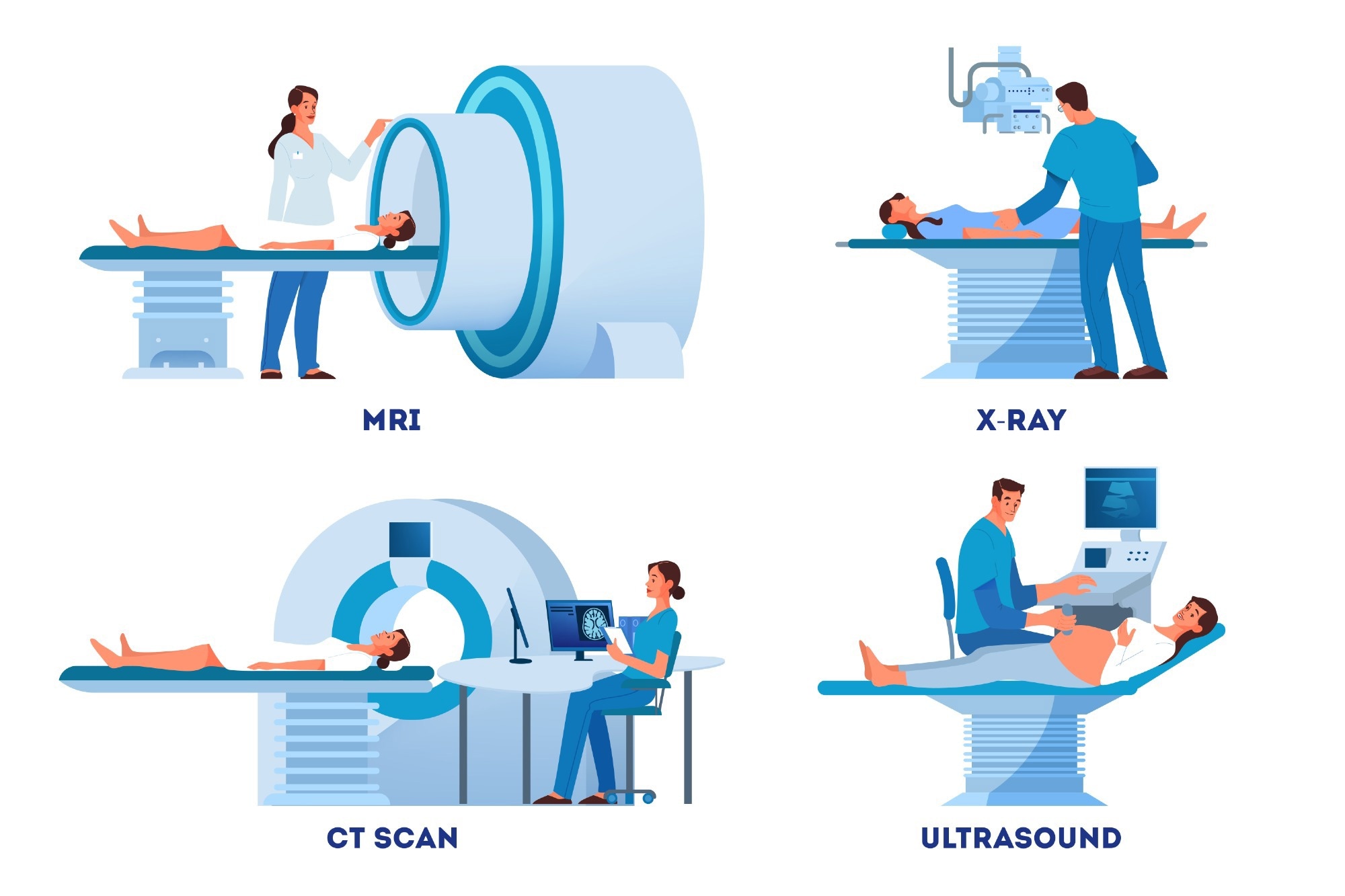
Imaging technologies are directed mainly at elucidating the structure or function of tissues and organs. Structural imaging includes producing images of the anatomy and morphology of the body part generated using computed tomography (CT), magnetic resonance imaging (MRI), and ultrasound (US) scans.
Conversely, the working of a tissue or organ in health and disease is equally vital data for diagnosis and treatment and is called functional imaging. This includes multiple quantitative imaging techniques that look into physiology at the molecular level, using metabolites and other molecules involved in cellular pathways.
Techniques like CT, MRI, and US scanning also allow for functional imaging. However, these are complemented by others, such as positron emission tomography (PET), single-photon emission computed tomography (SPECT), and optical imaging. Whereas the former is better at providing structural and anatomical images, all help to arrive at a good idea of organ function.
However, the spatial resolution of each modality varies, with MRI and US imaging providing a resolution of 50-500 μm and 200 μm, respectively. CT, PET, SPECT, and optical imaging have a resolution of 0.5-1 mm, 1-4 mm, 0.3-3 mm, and 0.1-10 mm, respectively.
The development of contrast agents has helped to provide greater resolution and specificity to the final images, reducing the proportion of noise to signal and allowing both purposes to be fulfilled with the same imaging technique.
Radiation exposure
CT, SPECT, and PET imaging modalities all expose the patient to ionizing radiation, a disadvantage not shared by MRI, US, or optical imaging. On the other hand, MRI is a relatively expensive modality, while the latter two techniques have relatively poor tissue penetration, offering low-quality images beyond the surface.
Together, these are often used to provide more information with lower radiation exposure than one set alone. This is also called multimodal imaging and takes advantage of the complementary aspects of each technique individually. For instance, hybrid PET-MRI scanners are being tested preclinically for their ability to provide dynamic imaging without exposure to ionizing radiation.
The outcome is a more precisely defined knowledge of where a disease process is located, how it affects the organ or tissue, and the patient’s health overall. It also helps to decide how best to treat the patient and monitor their health during and after treatment.
Individual techniques
Computerized tomography (CT)
CT scanning uses an X-ray beam passed through the body that is partly absorbed or scattered within the imaged organ. The residual X-rays follow multiple linear paths to fall onto a rotating detector, forming a cross-sectional image of the body. While the CT scan uses more radiation than an ordinary X-ray, the volume of the body to be scanned, the number of sequences, and the quality/resolution of the images desired all affect the radiation dose.
Sometimes contrast CT scans are used, with heavy molecules used as dyes to help the soft tissues stand out at more excellent resolution. Iodine-based compounds are used as water-soluble dyes and also to measure renal function. These do not confer color on the organs but change how the imaging beam interacts with them.
Ionic and non-ionic iodine-based dyes are used, with high and low osmolarity. Second-generation compounds based on barium or gadolinium, with lower osmolarity and toxicity than ionic compounds. Unfortunately, these may sometimes trigger allergic reactions in up to 3% with non-ionic dyes but up to 12% with ionic contrast.
CT scanning has come into its own in angiography and other cardiovascular applications. CT angiography (CTA) can show arteries and veins within an organ in a 3D view from any desired angle. Another application is the artery calcium score, which uses CT scans to visualize calcium deposits within the coronary arteries, indicating a higher risk of cardiovascular disease.
Magnetic resonance imaging (MRI)
MRI is a technique that uses magnetic fields to align the protons within hydrogen atoms found in water which makes up most of the human body. The MRI scanner emits short radio wave pulses, exciting the protons and breaking up their alignment in the scanned part of the body. As the protons realign, they emit radio waves that are detected to produce high-resolution images of organs and internal structures.
The MRI signal is thus based on the water content and magnetic properties of the body part imaged because the speed of realignment varies from tissue to tissue, producing different signals in each. The millions of radio wave emissions are integrated by a computer to provide a detailed picture of the inside of the organ or the body.
Gadolinium-based non-ionic contrast agents can also be used. Interestingly, the discovery that deoxyhemoglobin is a strongly paramagnetic molecule is used to understand changes in the structure and activity of the brain. The resulting local magnetic field disturbances around and within blood vessels alters the MRI appearances near them.
This has led to the use of functional MRI to detect how tumors, cerebrovascular accidents, brain trauma, and neurodegenerative disorders affect the brain and produce a map of the brain’s structure. This is called BOLD (Blood Oxygen Level Dependent) contrast.
MRI does not employ ionizing radiation and is considered among the safest imaging platforms. Researchers have not found harm from using a brief strong magnetic field. However, metal implants, including pacemakers and metal implants, may heat up or fail if exposed to this technique. Pregnancy is a contraindication as well.
Positron emission tomography (PET) and single-photon emission computed tomography (SPECT)
SPECT and PET are both highly sensitive nuclear imaging techniques, where small amounts of radioactive tracers are used to produce images of the body part where they are concentrated. External detectors are responsible for capturing the radiation. These are fed to a computer that generates the image.
The main limitation of these techniques is the poor spatial resolution, as well as, with SPECT, the lack of attenuation that is required to build the image accurately, and the few radiopharmaceuticals available currently. The radiotracers are excreted within 72 hours.
Related Stories
- Pioneering new medical imaging solutions
- See it to Believe it: How Medical Imaging Technologies Could Help Reduce Health Risks and Inspire Behavior Change
- Sectra signs digital pathology contract with Erasmus MC
PET is useful in studying metabolically active tissue, its structure, function, and biochemical characteristics. It uses positron emitters, while SPECT uses γ photon emitters, which have slightly longer half-lives. The positrons come from the breakdown of the radionuclide, like fluorodeoxyglucose (FDG), created by attaching a glucose atom to a radioactive label.
The positrons collide with nearby electrons to create gamma rays or annihilation protons. These are detected by the gamma-ray scanners, and the signals are passed to the computer to create an image map displaying the tissue structure and how metabolically active it is.
PET uses a larger range of compounds, expanding its ability to visualize cellular metabolic and functional pathways. The final image is also more accurate with PET because of the corrections applied to the image during reconstruction.
However, all PET tracer molecules have the same decay energy, preventing the distinguishing of different tracers simultaneously. In addition, increased availability of radionuclides and the introduction of gamma camera systems have extended the reach of PET.
Proton magnetic resonance spectroscopy (1H-MRS) is another technique based on the relationship between proton resonance frequency and the chemical environment, lipids, water, amino acids, and the like. This allows evaluation of the brain and metabolic processes during health and disease.
Ultrasound (US)
US imaging uses sound waves of 1-12 MHz frequency to reflect off internal body structures, thus producing accurate images of such body parts. The underlying principle is the principle of reflection depending on the distance of the reflective surface from the origin of the sound wave. Echocardiography is invaluable in assessing heart size and function, as well as the function of the heart valves.
In contrast, the US has been developed, where gas-filled microbubbles are used intravascularly. They have been proven safe while increasing spatial resolution at a relatively low cost. Doppler US scanning has also proven useful in measuring blood flow through blood vessels.
Optical imaging
Optical imaging uses digital cameras to detect molecular emissions from electromagnetic waves. Without ionizing radiation, it is suitable for repeated examinations, while the addition of contrast can help distinguish between soft tissues. Multiple techniques have been introduced, including diffuse optical tomography (DOT), optical coherence tomography (OCT), and hyper-spectral imaging.
DOT uses low-frequency red and infrared light to detect changes in the concentrations of certain molecules and thus identify changes in cellular function. OCT uses backscattered light detected on the principle of interference and is helpful in examining deeper images. Imaging spectroscopy, meanwhile, combines conventional digital imaging and spectroscopy.
A fascinating advance in this area is molecular imaging, where specific biomolecules that are operative in certain cellular processes underlying one or more disease states are targeted selectively by the imaging modality. Labeled molecules are required, as well as a detector and a ligand to bind to the molecular target, whether this is an antibody, peptide, or small molecule.
Molecular imaging agents are still few, however, and their development is slow. Moreover, the personalized nature of this technique makes its commercialization a less attractive possibility. Nevertheless, the continuing trend towards increased effectiveness and fewer adverse effects in the development of medical diagnostics will probably make multimodal imaging a commonplace entity in various medical conditions.
References:
- Barsanti, C. et al. (2015). Diagnostic and prognostic utility of non-invasive imaging in diabetes management. World Journal of Diabetes. https://doi.org/10.4239%2Fwjd.v6.i6.792. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4478576/. Accessed on June 23, 2022.
- Hanson, G. (2017). 7 Types of Diagnostic Imaging Tests You May Assist with as a Radiologic Technologist. https://www.rasmussen.edu/degrees/health-sciences/blog/types-of-diagnostic-imaging/. Accessed on June 23, 2022.
- Umar, A. A. et al. (2019). A review of Imaging Techniques in Scientific Research/Clinical Diagnosis. MOJ Anatomy & Physiology. https://doi.org/10.15406/mojap.2019.06.00269. https://medcraveonline.com/MOJAP/a-review-of-imaging-techniques-in-scientific-researchclinical-diagnosis.html. Accessed on June 23, 2022.
- Gilson, W. D. et al. (2022). Noninvasive Cardiovascular Imaging Techniques for Basic Science Research: Application to Cellular Therapeutics. Revista Espanola de Cardiologia. DOI: 10.1016/S1885-5857(09)72656-8. https://www.revespcardiol.org/en-noninvasive-cardiovascular-imaging-techniques-for-articulo-13140623. Accessed on June 23, 2022.
- Baerlocher, M. O. et al. (2010). The Use of Contrast Media. CMAJ. https://doi.org/10.1503%2Fcmaj.090118. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2855918/. Accessed on June 28, 2022.
- Overview – MRI Scan. https://www.nhs.uk/conditions/mri-scan. Accessed on June 28, 2022.
- BOLD Contrast Mechanism (2021). https://mriquestions.com/bold-contrast.html. Accessed on June 28, 2022.
- Single Photon Emission Computed Tomography (SPECT) (2021). https://www.heart.org/en/health-topics/heart-attack/diagnosing-a-heart-attack/single-photon-emission-computed-tomography-spect. Accessed on June 28, 2022.
- Positron Emission Tomography (PET) (2022). https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/positron-emission-tomography-pet. Accessed on June 28, 2022.
Further Reading
Last Updated: Sep 29, 2022
Currently rated 5.0 by 2 people

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
[Abstract + References] Self-Rehabilitation – Book Chapter
Posted by Kostas Pantremenos in Books, REHABILITATION on September 29, 2022
Abstract
Self-rehabilitation has an increasingly important role in rehabilitation. However, there are very few data regarding the methodology for creating a self-rehabilitation program available in the literature.
References
- WHO. World Health Organization International classification of functioning, disability and health. Geneva, Switzerland: World Health Organization; 2001.Google Scholar
- Feleus A, van Dalen T, Bierma-Zeinstra SM, et al. Kinesiophobia in patients with non-traumatic arm, neck, and shoulder complaints: a prospective cohort study in general practice. BMC Musculoskelet Disord. 2007;8:117.CrossRef Google Scholar
- Ryall C, Coggon D, Peveler R, Poole J, Palmer KT. A prospective cohort study of arm pain in primary care and physiotherapy – prognostic determinants. Rheumatology (Oxford). 2007;46:508–15.CAS CrossRef Google Scholar
- American Physical Therapy Association. American Physical Therapy Association Interactive guide to physic. Alexandria, VA: American Physical Therapy Association; 2003.Google Scholar
- Williams AC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev. 2012;11:CD007407.PubMed Google Scholar
- Brody LT. Effective therapeutic exercise prescription: the right exercise at the right dose. J Hand Ther. 2012;25(2):220–32.CrossRef Google Scholar
- McDonough CM, Jette AM. The contribution of osteoarthritis to functional limitations and disability. Clin Geriatr Med. 2010;26:387–99.CrossRef Google Scholar
- Kegerreis S. The construction and implementation of functional progressions as a component of athletic rehabilitation. J Orthop Sports Phys Ther. 1983;5:14–9.CAS CrossRef Google Scholar
- Mueller M, Maluf K. Tissue adaptation to physical stress: a proposed “physical stress theory” to guide physical therapy practice, education, and research. Phys Ther. 2001;82:383–403.CrossRef Google Scholar
- Hakkinen K, Kallinen M, Linnamo V, Pastinen UM, Newton RU, Kraemer WJ. Neuromuscular adaptations during bilateral versus unilateral strength training in middle-aged and elderly men and women. Acta Physiol Scand. 1996;158(1):77–88.CAS CrossRef Google Scholar
- Kubo K, Ohgo K, Takeishi R, et al. Effects of isometric training at different knee angles on the muscle tendon complex in vivo. Scand J Med Sci Sports. 2006;16:159–67.CAS CrossRef Google Scholar
- Paddon-Jones D, Leveritt M, Lonergan A, Abernethy P. Adaptation to chronic eccentric exercise in humans: the influence of contraction velocity. Eur J Appl Physiol. 2001;85(5):466–71.CAS CrossRef Google Scholar
- Seger JY, Arvidsson B, Thorstensson A. Specific effects of eccentric and concentric training on muscle strength and morphology in humans. Eur J Appl Physiol Occup Physiol. 1998;79(1):49–57.CAS CrossRef Google Scholar
- Wernbom M, Augustsson J, Thomee R. The influence of frequency, intensity, volume and mode of strength training on whole muscle cross-sectional area in humans. Sports Med. 2007;37(3):225–64.CrossRef Google Scholar
- American College of Sports Medicine. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2009;41:687–708.CrossRef Google Scholar
- Valdes K, Boyd JD, Povlak SB, Szelwach MA. Efficacy of orthotic devices for increased active proximal interphalangeal extension joint range of motion: a systematic review. J Hand Ther. 2019;32(2):184–93.CrossRef Google Scholar
- Metsios GS, Moe RH, Kitas GD. Exercise and inflammation. Best Pract Res Clin Rheumatol. 2020;34:101504.CrossRef Google Scholar
- Reinold MM, Escamilla RF, Wilk KE. Current concepts in the scientific and clinical rationale behind exercises for glenohumeral and scapulothoracic musculature. J Orthop Sports Phys Ther. 2009;39(2):105–17.CrossRef Google Scholar
- Frank C, Woo SL, Amiel D, Harwood F, Gomez M, Akeson W. Medial collateral ligament healing. A multidisciplinary assessment in rabbits. Am J Sports Med. 1983;11(6):379–89.CAS CrossRef Google Scholar
- Woo SL, Takakura Y, Liang R, Jia F, Moon DK. Treatment with bioscaffold enhances the fibril morphology and the collagen composition of healing medial collateral ligament in rabbits. Tissue Eng. 2006;12(1):159–66.CAS CrossRef Google Scholar
- Niyibizi C, Kavalkovich K, Yamaji T, Woo SL. Type V collagen is increased during rabbit medial collateral ligament healing. Knee Surg Sports Traumatol Arthrosc. 2000;8(5):281–5.CAS CrossRef Google Scholar
- Nguyen TD, Liang R, Woo SL, Burton SD, Wu C, Almarza A, Sacks MS, Abramowitch S. Effects of cell seeding and cyclic stretch on the fiber remodeling in an extracellular matrix-derived bioscaffold. Tissue Eng Part A. 2009;15(4):957–63.CAS CrossRef Google Scholar
- Uhl TL, Muir TA, Lawson L. Electromyographical assessment of passive, active assistive, and active shoulder rehabilitation exercises. PM R. 2010;2:132–41.CrossRef Google Scholar
- Zelenski NA, Shin AY. Management of nondissociative instability of the wrist. J Hand Surg Am. 2020;45(2):131–9.CrossRef Google Scholar
- Mesplié G, Grelet V, Léger O, Lemoine S, Ricarrère D, Geoffroy C. Rehabilitation of distal radioulnar joint instability. Hand Surg Rehabil. 2017;36(5):314–21.CrossRef Google Scholar
- Hall C. Patient management. In: Brody L, Hall C, editors. Therapeutic exercise: moving toward function, vol. 3. Philadelphia, PA: Wolters Kluwer/Lippincott Williams & Wilkins; 2011. p. 91–4.Google Scholar
- Kanehisa H, Nagareda H, Kawakami Y, et al. Effects of equivolume isometric training programs comprising medium or high resistance on muscle size and strength. Eur J Appl Physiol. 2002;87(2):112–9.CAS CrossRef Google Scholar
- Prithishkumar IJ, Michael SA. Understanding your student: using the VARK model. J Postgrad Med. 2014;60(2):183–6.CAS CrossRef Google Scholar
- Aydın L, Ilhan AŞ, Kızıltan E, Yazıhan N, Yazıcı AC, Gundogan NU. The influence of six-year medical education on learning styles in medical students at Baskent University. Open Access Libr J. 2015;02(04):1–8.Google Scholar
- Valdes K, Gendernalik E, Hauser J, Tipton M. Use of mobile applications in hand therapy. J Hand Ther. 2020;33(2):229–34.CrossRef Google Scholar
[WEB] New Data on Stroke Recovery Patterns May Guide Rehabilitation
Posted by Kostas Pantremenos in Recovery Plateau, REHABILITATION on September 29, 2022
Long-term recovery patterns after a stroke differ in different functional domains and vary by patient age, stroke severity, and stroke type, a new study shows.
The results also suggest that improvements occur in many functional domains over a longer timescale than previously thought, with consequent implications for rehabilitative care.
“Understanding the diversity of long-term functional recovery patterns and factors associated with these outcomes in survivors of stroke may help clinicians develop strategies for effective stroke care and rehabilitation,” the Korean authors conclude.
The study was published online September 23 in JAMA Network Open.
The researchers, led by Seyoung Shin, MD, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea, explain that a thorough understanding of long-term functional outcomes after stroke is important for setting suitable management plans and correctly informing patients and their families about prognoses.
They note that while disability and mortality are the most important outcomes, stroke is associated with diverse functional impairments that vary by lesion location or size, and long-term outcomes in different functional domains need to be understood separately to establish adequate stroke management strategies in accordance with individual patient needs. Moreover, it would be worthwhile to examine whether functional recovery patterns differ by clinical characteristics already known to be associated with stroke prognosis, such as age, stroke type, or stroke severity, they write.
For the current study, the researchers examined long-term recovery patterns in diverse functional domains and factors associated with outcomes among patients with first-time stroke.
They analyzed data from a cohort of 4443 patients (3508 with ischemic and 935 patients with hemorrhagic stroke) who underwent repeated functional assessments for 60 months after their stroke.
Recovery Continued Up to 18 Months
Overall, functional scores showed significant improvement in most domains until 12 or 18 months after stroke onset and then plateaued and declined after 30 months.
However, recovery patterns differed significantly by age, initial stroke severity, and stroke type.
Some reports have suggested that activities of daily living (ADL) and motor functions plateau after 6 months, they write, “however, our results demonstrated that recovery continued for more than 1 year in all functional domains and until 18 months in motor, ambulatory, and ADL functions.”
These suggest that these outcomes may be associated with improvements in structural stroke care and comprehensive rehabilitation services in recent years.
Functional recovery occurred “rapidly in acute and subacute phases of stroke, especially in younger patients, those with moderate or severe stroke severity,” and patients with hemorrhagic stroke, they add. “Those phases are a time when patients should receive as much restorative therapy as needed to obtain maximal recovery,” the researchers state.
In the chronic stage of stroke, on the other hand, functional decline occurred beginning 30 months after onset, which suggests that maintenance care strategies are of utmost importance at that time, they add.
Noting that a previous study has found that late recovery was associated with reduced mortality and healthcare cost in patients with stroke, they say that stroke care should be extended to provide rehabilitation services needed by individual patients even in the chronic phase.
The study also showed that age is an important factor associated with functional outcomes after stroke, with older patients (65 years plus) having lower scores than younger patients in all functional domains at every time point. While older patients with stroke had noticeable functional recovery during the subacute phase, most functions declined from 18 to 60 months after stroke.
“These findings emphasize that older patients with stroke should be monitored closely for possible functional deterioration in the chronic stage,” the researchers say.
Functional recovery patterns also differed by stroke severity and type, with moderate and severe groups showing rapid recovery during the first 6 to 12 months after stroke, and patients with hemorrhagic stroke, who had higher severity at onset, experiencing more rapid restoration of function in the first 12 months after stroke than patients with ischemic stroke.
The study also found that functional status at 7 days after stroke was associated with outcomes of other functional domains after 60 months. For example, higher scores at day 7 on the Korean Mini-Mental State Examination (K-MMSE) scale were associated with good functional outcomes in all six functional domains, including motor, ambulatory, swallowing, language, and ADL performance.
Implications for Post-Stroke Rehabilitation
Commenting on the study for theheart.org | Medscape Cardiology, Wendy Ziai, MD, professor of neurology, neurosurgery, anesthesiology & critical care medicine at Johns Hopkins University School of Medicine, Baltimore, Maryland, said: “This study is important because it highlights, as with other types of acute brain injury, that full recovery takes a very long time. Also noteworthy is that most measures of disability, especially motor and cognitive function, recover concomitantly and may be interdependent.”
She added: “This has implications for post-stroke rehabilitation and the duration over which such interventions may continue to optimize functional recovery. It also implies limits on ultimate recovery, especially at higher age, although it is not known whether efforts to maintain functional plateaus may be effective.”
Ziai noted that the data support the use and potential benefit of longer-term follow-up for stroke clinical trials.
She also pointed out that the current study used standardized tests of motor, ambulatory, cognitive, language, swallowing, and ADL functions, and future research is required to translate these outcomes into those that are important to stroke survivors including return to work, driving, and participation in other meaningful social activities.
This study was supported by grants from the Korea Disease Control and Prevention Agency and the National Research Foundation of Korea. The researchers have reported no relevant financial relationships.
JAMA Netw Open 2022. Published online September 23, 2022. Full text
[WEB] Mental Health During the COVID-19 Pandemic
Posted by Kostas Pantremenos in COVID-19 on September 29, 2022
An Urgent Issue
Both SARS-CoV-2 and the COVID-19 pandemic have significantly affected the mental health of adults and children. In a 2021 study, nearly half of Americans surveyed reported recent symptoms of an anxiety or depressive disorder, and 10% of respondents felt their mental health needs were not being met. Rates of anxiety, depression, and substance use disorder have increased since the beginning of the pandemic. And people who have mental illnesses or disorders and then get COVID-19 are more likely to die than those who don’t have mental illnesses or disorders.
Mental health is a focus of NIH research during the COVID-19 pandemic. Researchers at NIH and supported by NIH are creating and studying tools and strategies to understand, diagnose, and prevent mental illnesses or disorders and improve mental health care for those in need.
How COVID-19 Can Impact Mental Health
If you get COVID-19, you may experience a number of symptoms related to brain and mental health, including:
- Cognitive and attention deficits (brain fog)
- Anxiety and depression
- Psychosis
- Seizures
- Suicidal behavior
Data suggest that people are more likely to develop mental illnesses or disorders in the months following infection, including symptoms of post-traumatic stress disorder (PTSD). People with long COVID may experience many symptoms related to brain function and mental health.
How the Pandemic Affects Developing Brains
The impact of the COVID-19 pandemic on the mental health of children is not yet fully understood. NIH-supported research is investigating factors that may influence the cognitive, social, and emotional development of children during the pandemic, including:
- Changes to routine
- Virtual schooling
- Mask wearing
- Caregiver absence or loss
- Financial instability
Not Everyone Is Affected Equally
While the COVID-19 pandemic can affect the mental health of anyone, some people are more likely to be affected than others. People who are more likely to experience symptoms of mental illnesses or disorders during the COVID-19 pandemic include:
- People from racial and ethnic minority groups
- Mothers and pregnant people
- People with financial or housing insecurity
- Children
- People with disabilities
- People with preexisting mental illnesses or substance use problems
- Health care workers
People who belong to more than one of these groups may be at an even greater risk for mental illness.
Telehealth’s Potential to Help
The pandemic has prevented many people from visiting health care professionals in person, and as a result, telehealth has been more widely adopted during this time. Telehealth visits for mental health and substance use disorders increased significantly from 2020 to 2021 and now make up nearly half of all total visits for behavioral health.
Widespread adoption of telehealth services may help people who otherwise would not be able to access mental health support, such as people in rural areas or places with few providers.

Frequently Asked Questions
I have a preexisting mental illness. Is COVID-19 more dangerous to me?
COVID-19 can be worse for people with mental illnesses. Data suggest that people who reported symptoms of anxiety or depression had a greater chance of being hospitalized after a COVID-19 diagnosis than people without those symptoms.
The Centers for Disease Control and Prevention (CDC) reports that having mood disorders and schizophrenia spectrum disorders can increase a person’s chances of having severe COVID-19. People with mental illnesses who belong to minority groups are also more likely to get COVID-19. And people with schizophrenia are significantly more likely to get COVID-19 and more likely to die from it.
Despite these risks, effective treatments are available. If you have a preexisting mental illness and get COVID-19, talk to your health care professional to determine the treatment plan that’s appropriate for you.
I’m experiencing symptoms of a mental illness or disorder. What should I do?
If you are experiencing symptoms of anxiety, depression, or any other mental illness or disorder, there are ways you can get help. For immediate help:
- Call 911
- Call or text the 988 Suicide & Crisis Lifeline at 988 (para ayuda en español, llame al 988)
- Call or text the Disaster Distress Helpline, 1-800-985-5990 (press 2 for Spanish)
- The Substance Abuse and Mental Health Services Administration can help you find mental health or substance use specialists.
- Talk to your health care professional or mental health care professional. Together, you can work on a plan to manage or reduce your symptoms.
What research is NIH doing on the mental health impacts of COVID-19?
The National Institute of Mental Health (NIMH) and other NIH Institutes have created research initiatives to address mental health for people in general and for the most vulnerable people specifically. Examples of this research include:
- NIMH launched a five-year research study called RECOUP-NY to promote the mental health of New Yorkers from communities hard-hit by COVID-19. The study will test the use of a new care model called Problem Management Plus (PM+) that can be used by non-specialists.
- A study funded by NIMH is examining the use of mobile apps to address mental health disparities.
- The Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) is funding research to understand the effects of mask usage for children, including any impacts on their emotional and brain development.
- NIMH is funding research on the impacts of the pandemic on underserved and vulnerable populations and on the cognitive, social, and emotional development of children.
- The National Institute on Alcohol Abuse and Alcoholism (NIAAA) is funding research on how COVID-19 and SARS-CoV-2 affect the causes and consequences of alcohol misuse.
- A collaborative study supported by NIMH and the National Center for Complementary and Integrative Health (NCCIH) enrolled more than 3,600 people from all 50 U.S. states to understand the stressors affecting people during the pandemic.
[ARTICLE] Bilateral Lower Limb Training for Post-stroke Survivors: A Bibliometric Analysis – Full Text
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop on September 28, 2022
Abstract
Stroke is one of the most disabling conditions affecting the middle-aged population all around the world. This study aims to explore the rehabilitation of stroke patients using bibliometric analysis, which includes statistical analysis of recent articles, books, and other kinds of publications, to assess scientific output and determine the significance of scientific investigations in terms of both quality and quantity. In this study, an analysis of global trends in research in bilateral lower limb training for training balance and walking for patients in the subacute stage post-stroke between 1988 and 2021 was done. All the articles were obtained from PubMed databases. CiteSpace software was used to analyze the relationship between publications and country, journals, institutions, authors, references, and the keywords used. A total of 160 publications were included in the analysis. There was a tremendous increase in the research of physiotherapy intervention in patients who had residual disability post-stroke with a publication rate of 7.1 articles per year of publications. The use of the sophisticated PubMed database to extract articles allowed for a thorough and powerful bibliometric analysis of stroke rehabilitation research published between 1988 and 2020. In general, the number of studies on bilateral training has increased in recent decades. This historical overview of rehabilitation for post-stroke survivors will serve as a valuable starting point for future study into possible collaborators, focus issues, and trends. This bibliometric analysis highlights the potential value of exercise therapy for stroke survivors in creating more effective hemiplegia rehabilitation programs. This research may encourage the use of strengthening in the therapeutic therapy of hemiplegia balance. The groundwork will be laid for future research on strengthening stroke to be organized and given top priority.
Introduction & Background
Stroke as defined by the World Health Organization is “Fast-developing clinical evidence of localized (or general) brain dysfunction, with symptoms lasting 24 hours or more or leading to death, with no obvious etiology other than vascular origin” [1,2]. Its prevalence is increasing day by day and has reached to a point that 0.84 individuals out of 1,000 have a high risk of getting a stroke, leading to hemiplegia and hemiparesis [3-7]. Post-stroke the weakness leads to difficulty in performing daily activities and deteriorating the life of the individual. Early rehabilitation not only provides quality of life but also increases longevity [8,9].
As there is affection on the opposite side of the lesion, the unaffected side is supposed to be having no change in its performance [8,10,11]. But, in reality, it is not so, it is also affected, but less than the opposite one [12]. There is bilateral paralysis due to the uncrossed fibers affecting the overall individual’s life. Training the individual in a task-oriented pattern along with strengthening not only helps in improving balance but also makes the person ambulate independently [13-15].
For the hemi patients, while planning any protocol, we focus on the affected side, thus the other side goes into further deterioration [16-19]. Training both sides equally, although focusing on the affected side helps to improve the overall well-being of the individual [20]. There are many studies done for the upper limb for the same objective, but there is ample gap for the lower limb. Thus, this research will milestone in its own way. […]
[ARTICLE] Stroke survivors’ experiences with home-based telerehabilitation using an assistive device to improve upper limb function: a qualitative study – Full Text
Posted by Kostas Pantremenos in Paretic Hand, REHABILITATION, Tele/Home Rehabilitation on September 28, 2022
Abstract
Purpose
Patients in the chronic phase after stroke often lack the possibility to intensively train their upper limb function. Assistive devices can be a solution to training intensively at home. This qualitative study investigated stroke survivors’ experiences regarding training using the hoMEcare aRm rehabiLItatioN (MERLIN) system, an assistive device and telecare platform. We investigated patients’ perspectives regarding the home-based training with the MERLIN system, on the International Classification of Functioning, Disability and Health (ICF) domains and the facilitators and barriers of the MERLIN system.
Methods
Eleven patients in the chronic phase of stroke who completed the MERLIN trial took part in semi-structured interviews. Interviews were analysed using the framework method.
Results
Participants were in general positive about the device and the training. Several experienced positive effects on ICF body functions, such as joint range of motion and self-confidence. Some experienced improvements in activities, but not on participation level. Home training had advantages: flexibility in training time and duration and no need to travel. The major barriers were technical hard- and software issues and ergonomic complaints. A list of recommendations regarding assistive devices and home-based rehabilitation was created.
Conclusions
Homebased training using an assistive device was well received by stroke patients to train their upper limb function. Future device developers should take patients’ feedback into account to overcome the barriers related to the introduction of new assistive devices at home. Our recommendations may be the first step to implementing patients’ perspectives during the early stages of device development.
- Implications for rehabilitation
- Training at home was a well-received and convenient solution to improve the upper limb function
- Barriers regarding hard- and software and device ergonomics need to be addressed in future assistive devices
- Recommendations are provided for more successful implementation of assistive devices and home-based telerehabilitation programs
Introduction
Stroke can have a major impact on someone’s life. Multiple cognitive and physical problems are commonly seen in stroke patients, such as problems with concentrating, walking or using the upper limb. In rehabilitation centres most time is spent on improving walking, the upper limb is often undertreated [1]. According to a qualitative study among stroke survivors, arm function seems to be neglected during the critical time window during rehabilitation [1]. This imbalance may result in many patients having remaining problems using the arm or hand in daily life. After the first six months post-stroke, there are often minimal opportunities for further training [2]. Other factors such as travel time, travel costs or lack of transportation towards the facility may also be a burden to continue training.
To pursue training on an intensive level, home programs can be a solution. By means of home training, patients can increase the amount of training time. Assistive devices are often used to provide training programs at home, such as electro-stimulation in combination with exercises, orthoses, joysticks or spring systems [3–8]. These devices have the advantage of guiding and monitoring the patient’s movements. The use of assistive devices makes it possible to train for more hours in comparison to supervised training [9]. Another great advantage of assistive devices is enhanced engagement due to fun and challenging exercises. Home training can especially be useful during the chronic phase of stroke since patients are only reimbursed for a limited number of training sessions per year due to limited resources of the current healthcare system, as is e.g. the case in the Netherlands. It is generally known that much repetition is necessary to achieve functional recovery [10]. Repeatedly performing the same movement can be demotivating and may lead to boredom. Stroke survivors emphasise that it is difficult to adhere to performing exercises daily if the training is not interesting [1]. Gaming for rehabilitation purposes is therefore a useful addition to assistive devices in the patients’ homes.
The International Classification of Functioning, Disability and Health (ICF) is often used to investigate the effect of training on function, activity and participation levels [11]. While qualitative studies often focus on the improvement of body functions [12], less information is available on whether the training also has an impact on the patient’s activity or participation level. A qualitative approach can reveal the experiences and perspectives of the patients regarding changes in ICF levels, as also their opinions on the rehabilitation program and the feasibility of device usage at home. External and personal factors are often not taken into consideration and they are especially important when training at home.
This study investigates stroke survivors’ experiences with training their upper limb function at home with hoMEcare aRm rehabiLItatioN (MERLIN), an assistive device combined with a telecare platform and serious gaming [13]. The aims of this study were to 1) investigate the experiences and perspectives of chronic stroke survivors on ICF levels (body functions, activities and participation) and ICF factors (external and personal) after using MERLIN to train the upper limb function at home; 2) describe the facilitators and barriers regarding upper limb training at home using MERLIN.[…]
[WEB] About brain injury
Posted by Kostas Pantremenos in TBI on September 26, 2022
An acquired brain injury (ABI) is an injury caused to the brain since birth. There are many possible causes, including a fall, a road accident, tumour and stroke.
This section gives an overview of the brain, brain injury and the practical issues that can arise.
It is divided into sections for individuals who are affected by brain injury, professionals who work in the field of brain injury, and further information about brain injury.
Because of your cookies settings you are unable to see this video. If you’d like to view it, please visit our cookies page, scroll down and click the ‘Cookies Settings’ button. Enabling cookies will allow you to view all of the content on our website. After enabling cookies (above link) please click to refresh the page to show the video.
Information for individuals
Find out about how acquired brain injury affects survivors, family members, carers and the people around them. We provide information to help at the different stages of brain injury, from hospital to home.
Types of brain injury
Acquired brain injury can have a number of different causes. Some of the most common types of brain injury include:
- Traumatic brain injury (for instance road traffic collisions, falls or assaults)
- Minor head injury and concussion (loss of consciousness of less than 15 minutes)
- Aneurysm (also known as a cerebral aneurysm)
- Brain haemorrhage (also known as a haemorrhagic stroke)
- Brain tumour
- Carbon monoxide poisoning
- Encephalitis
- Hypoxic/anoxic brain injury (caused a reduction or loss of oxygen to the brain)
- Meningitis
- Stroke
Effects of brain injury
A brain injury can lead to a wide range of effects. While many people recover quickly after a minor head injury (often known as concussion), this is not always the case and people may experience longer-term effects.
The more severe the brain injury, the longer-term and more pronounced the effects are likely to be. Some people may spend time in a coma, or experience a more prolonged reduced awareness state. During the early stages of recovery, brain injury survivors often go through a stage called Post-traumatic amnesia, where they have no continuous memory of day-to-day events and their behaviour may be very uncharacteristic and confused.
A brain injury can cause behavioural and emotional changes, hormonal imbalances, difficulties with cognition and memory, a range of communication problems, physical effects and, very commonly, fatigue.
Hospital treatment and early recovery after brain injury
The time immediately after the injury is bound to be full of worry and uncertainty for everyone concerned.
We provide information on the different stages of recovery, from the time in the hospital and early rehabilitation through to discharge. Families may be able to access a grant to help with the unexpected costs of brain injury by applying to our Emergency Fund.
You can also set up a page on our I’m calling about Chris website to post updates on your loved one’s situation and allow family and friends to keep up-to-date. They can also access our information that explains how to support a family that is dealing with brain injury.
Rehabilitation and continuing care after brain injury
Rehabilitation aims to help the brain learn alternative ways of working in order to minimise the long-term impact of the brain injury. Rehabilitation also helps the survivor and the family to cope successfully with any remaining disabilities.
In this section you can find out more about what brain injury rehabilitation involves, and get information on the rehabilitation team that you will be working with.
After the initial phase of rehabilitation is complete, you may require continuing care, and want to find out about ways you can self-direct your support.
Practical issues after brain injury
A brain injury can lead to a wide range of difficulties in day-to-day life. For many people, a priority may be to seek financial support. This could involve getting legal advice to pursue compensation, applying for welfare benefits or applying for a grant from the Headway Emergency Fund.
In the longer-term, many brain injury survivors may want to return to driving, or get back to work or education.
They may also qualify for a Brain injury identity card, which is designed to provide brain injury survivors with added confidence in everyday social scenarios, and ensure they get the right support if they come into contact with the police.
Relationships after brain injury
For some people, the emotional, behavioural, physical and cognitive changes of brain injury can have an impact on existing and future relationships.
We explain how a brain injury effects relationships, with further information for partners and friends. We also provide in-depth information on an often overlooked issue – the affect of brain injury on sex and sexuality.
There is also useful information to help people with brain injury to cope with parenting and supporting children.
Information library
You can browse our full range of free booklets and factsheets in the information library.
Brain injury and me
Brain injury and me is an innovative and exciting website that raises awareness of brain injury through personal stories.
The Living with brain injury section contains a wide range of practical advice, incorporating the experiences and views of survivors and carers.
You can find the information you need using the menu or the quick links below. If you can’t find what you are looking for or have any more questions, please contact our helpline.
[BLOG POST] 30+ Years of research prove the validity of Virtual Reality
Posted by Kostas Pantremenos in Virtual reality rehabilitation on September 26, 2022

Click the “+” in front of the desired research category below.
+ VR IN NEURO REHAB
+ VR IN COGNITIVE TRAINING
+ VR FOR UE FUNCTION
+ VR FOR PAIN MANAGEMENT
+ VR FOR ANXIETY
+ VR FOR DEPRESSION
+ VR FOR GAIT & BALANCE
[BLOG POST] XR THERAPY SYSTEM CASE STUDIES
Posted by Kostas Pantremenos in Virtual reality rehabilitation on September 26, 2022





