Posts Tagged foot drop
[BLOG POST] Can an AFO actually be FUN?
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop on January 21, 2023
If you currently use a foot drop brace, you know how uncomfortable and “clunky” it can be.
And because of that, maybe you avoid some of your favorite activities because your mobility feels limited or awkward.
After a stroke, many things change, and your ability to comfortably navigate around your environment shouldn’t be one of them!
That’s why we recently launched Flex AFO. It’s a comfortable, low-profile foot drop brace that’s designed to be sturdy yet flexible.

Here’s what Patricia recently said about Flex AFO:
Return to natural walking freedom
“After my stroke 2 years ago I began recovery progressing through 4 rigid braces. At first they provided the needed support to walk but each was restricting me from a natural feeling walk. I saw an ad for Flint’s AFO ankle brace and asked my OT would she recommend it’s use for me. After reviewing it she said Go For It! Now after using the AFO which gives my foot it’s needed toe lift I’m enjoying the freedom of the other braces restrictions. My walking has become more naturally flowing. I never intend to choose to go back to the prior prescription braces.”
Patricia is not only having tons of fun with her new Flex AFO, but she describes the experience as “natural walking freedom.” We love that!
Now Patricia is getting back to the activities that she loves, like corn hole:

If you’re ready for a foot drop brace that helps you find fun and freedom — while providing flexible, sturdy support — then Flex AFO is perfect for you.
Here’s the link to learn more: https://www.flintrehab.com/product/afo/
[WEB] Serial Casting for Spasticity
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, Spasticity on January 9, 2023

When brain injuries cause spasticity in lower limbs and restrict joint mobility, casting can allow a patient to participate in rehabilitation.
by Naama Kenig, PT, DPT, and Shannon Motisi, PT, DPT
According to the Centers for Disease Control and Prevention, about 2% of the population are living with a disability due to brain injury.1 After an acquired brain injury, which may range from mild to severe, patients may benefit from time in an acute rehabilitation setting. One of the complications frequently seen after brain injury is the onset of spasticity.
Spasticity is defined as hyper-excitability of reflexes and over-activity of muscle groups. This occurs due to disruptions in pathways of the upper motor neurons and dysfunction of central nerve processes.2 Spasticity after brain injury can interfere with movement and therefore can impact mobility, self-care, positioning, and transfers. Also, spasticity and restrictions in joint mobility can lead to significant pain, which can impact a person’s ability to participate in rehabilitation.
Spasticity can be managed through pharmacological means or non-pharmacological means. The physiatrist determines the plan for pharmacological management, which may include the administration of oral medications such as baclofen, or with injections such as Botox or phenol. Physical therapists often utilize non-pharmacological interventions such as stretching, weight-bearing, serial casting, splinting, and electrical stimulation to manage spasticity.3 In acute rehabilitation, the treatment team works together to provide both pharmacological and non-pharmacological interventions, in conjunction with one another, to provide optimal management of spasticity.
Choosing Serial Casting
Serial casting is often utilized as a therapy tool in the inpatient rehabilitation setting for patients with severe brain injury.4,5 It is defined as the application of successive casts to a joint, set at submaximal range, for a prolonged stretch to the joint. Serial casting can be used to reduce spasticity, increase range of motion, prevent contractures, improve positioning, and improve mobility.6
In the lower extremities, serial casting may be applied at the ankle or the knee joint.7 At the ankle, an equino-varus deformity is the most common deformity that occurs due to spasticity. The plantarflexion and varus are due to overactivity of the related musculature, combined with the resting position of the foot when supine or in a non-weight-bearing position. At the knee, there may be a loss in range of motion due to either excessive flexion tone or excessive extension tone. Serial casting can be used to provide a stretch into either flexion or extension, to address the aforementioned limitations.

Prepping for Casting
When determining the need for serial casting, several aspects must be considered, including medical history, tolerance, ability to communicate, level of agitation, and skin integrity. Precautions to cast application include: current fractures, wounds, impaired circulation, and deep vein thrombosis.
Prior to cast application, therapists should take goniometric measurements of the joint’s range of motion. It is important to assess the range in a resting position, as well as the passive range of motion and active range of motion. Spasticity is measured using the Modified Ashworth Scale as well as the Modified Tardieu Scale, which has a higher test-retest and inter-rater reliability in adults with brain injury.8 The clonus score should be assessed as well. A thorough skin inspection must be performed prior to cast application to assess for any areas of skin breakdown or erythema. This information must be carefully documented in order to detect any possible changes post cast removal.
Casting Process
The patient is typically positioned on a treatment mat for lower extremity cast application. When applying a cast, the patient may be positioned in a prone or supine position, based on the patient’s tolerance. If supine, bolsters or wedges may be utilized in order to support the limb in the optimal position. Casting includes a partnership between two therapists: a “caster” and a “holder.” The “holder” provides the necessary sustained stretch, while the “caster” applies the cast. It is important to work in a quick and efficient manner so that the holder is able to sustain a sufficient stretch, in optimal alignment, and not fatigue.
A terry cloth stockinette is donned over the limb, encapsulating the joint. The fabric has some elasticity and provides padding. It is available in different measurements to accommodate differently sized limbs. Care must be taken to ensure it is not restrictive and will not compromise blood flow. Following the stockinette layer, layers of cotton cast padding are applied. Several layers are applied in order to provide proper padding, and extra layers are added at areas of bony prominences to reduce the risk of pressure points within the cast.
Finally, the casting tape is applied. The casting tape may be in the form of a plaster or fiberglass. While a plaster cast may be easier to mold, and is the cheaper option, fiberglass casts are lighter, stronger, and more durable. Plaster casts also take significantly longer to dry and set, and there is a risk of the plaster breaking or cracking while hardening.

Assessing After Application
After the cast is applied, capillary refill at the toes is assessed to ensure adequate blood supply to the extremity. Other evaluations performed after cast application include assessing coloration and temperature of the foot and noting any swelling of the limb. A finger must be able to be inserted into the cast around the circumference of both proximal and distal aspects of the cast, to ensure the cast does not become too restrictive.
These assessments are completed every two hours while the cast is donned. Nursing staff, as well as family and caregivers, are trained in performing these assessments as well.
As some level of edema is likely to occur while the cast is donned, it is recommended to avoid prolonged periods with the limb placed in a dependent position. Intermittent elevation of the lower extremity may help reduce the amount of swelling that will occur.
Cast Removal and Reapplication
When the cast is removed, a thorough skin inspection is completed to take note of any areas of skin breakdown. Goniometric measurements as well as spasticity measurements are reassessed. If positive change is noted and no skin breakdown has occurred, the next serial cast may be applied.
In our inpatient setting, we aim to ideally have the casts applied for five consecutive days. We typically remove the casts prior to the weekend, to reduce the chances of any concerns or issues arising over the weekend. When removed, a maintenance plan is determined in order to sustain any gains achieved with casting. This short-term plan typically consists of utilizing multi-podus boots, with continued skin checks every two hours.
If there are no skin issues over the weekend, and casting is still indicated, another round of casting will be completed at the start of the next week. This cycle of casting will continue as long as objective gains are made and there are no negative side effects, such as skin issues, excessive autonomic storming, or behavioral issues.
Maintaining Range
When the casting process is completed, it is important to maintain the new range that was achieved.9 There are several bracing options that are utilized. The serial cast may be bi-valved and then reapplied as a resting splint. A multi-podus boot can also help maintain range achieved. However, its use is somewhat limited if the patient continues to have significant range limitations. As a multi-podus boot does not allow for custom fitting, there may be areas of excessive pressure which can increase the risk of skin breakdown. Another option is dynamic splinting. Dynamic splints provide low-load prolonged duration stretch at end ranges of motion. The goal of dynamic splinting is to not only maintain rage, but to continue to improve it.10
The decision to cast a patient while they are in inpatient rehabilitation can be a challenging one. The casts may limit functional mobility in some capacity, and may make interventions such as gait training more challenging. They may also create more challenges for the caregiver during transfers, positioning, and ADLs. The treating team must weigh the pros and cons of casting, and consider the length of stay and goals in acute rehabilitation when making the determination to cast. Therefore, the time frame and number of serial casts applied in an inpatient setting may look differently than when done in an outpatient setting.
Naama Kenig, PT, DPT, graduated with her doctorate in Physical Therapy from SUNY Downstate Medical Center in 2013. She currently is a clinical therapy manager of the brain injury unit in Kessler Institute for Rehabilitation in West Orange, NJ. She is a board-certified clinical specialist in neurologic physical therapy.
Shannon Motisi, PT, DPT, graduated with her doctorate in Physical Therapy from Quinnipiac University in 2010. She currently is a clinical specialist in the brain injury unit in Kessler Institute for Rehabilitation in West Orange, NJ. She is a board-certified clinical specialist in neurologic physical therapy. For more information, contact RehabEditor@medqor.com.
References
1. Centers for Disease Control and Prevention.CDC: TBI Data and Statistics. Centers for Disease Control and Prevention.Published April 10, 2019. http://www.cdc.gov/traumaticbraininjury/data/
2. Enslin JMN, Rohlwink UK, Figaji A. Management of Spasticity After Traumatic Brain Injury in Children. Front Neurol. 2020 Feb 21;11:126. doi: 10.3389/fneur.2020.00126. PMID: 32153498; PMCID: PMC7047214.
3. Lee SJ, Sung IY, Jang DH, Yi JH, Lee JH, Ryu JS. The effect and complication of botulinum toxin type a injection with serial casting for the treatment of spastic equinus foot. Ann Rehabil Med. 2011;35(3):344-353. doi:10.5535/arm.2011.35.3.344
4. Singer BJ, Singer KP, Allison GT. Evaluation of extensibility, passive torque and stretch reflex responses in triceps surae muscles following serial casting to correct spastic equinovarus deformity. Brain Inj. 2003;17(4):309-324. doi:10.1080/0269905021000013237
5. Mortenson PA, Eng JJ. The use of casts in the management of joint mobility and hypertonia following brain injury in adults: a systematic review. Phys Ther. 2003;83(7):648-658.
6. Singer BJ, Singer KP, Allison GT. Evaluation of extensibility, passive torque and stretch reflex responses in triceps surae muscles following serial casting to correct spastic equinovarus deformity. Brain Inj. 2003;17(4):309-324. doi:10.1080/0269905021000013237
7. Leung J, Harvey LA, Moseley AM. An intensive programme of passive stretch and motor training to manage severe knee contractures after traumatic brain injury: a case report. Physiother Can. 2013;65(3):223-228. doi:10.3138/ptc.2012-29
8. Platz T, Eickhof C, Nuyens G, Vuadens P. Clinical scales for the assessment of spasticity, associated phenomena, and function: a systematic review of the literature. Disabil Rehabil. 2005;27(1-2):7-18. doi:10.1080/09638280400014634
9. Leung J, Stroud K. Long-Term Resolution of Severe Ankle Contractures Using Botulinum Toxin, Serial Casting, Splinting, and Motor Retraining. Physiother Can. 2018;70(2):152-159. doi:10.3138/ptc.2016-76
10. Curran S, Willis FB. Chronic Ankle Contracture Reduced: A Case Series. The Foot and Ankle Online Journal. Published online July 1, 2011. Doi:10.3827/faoj.2011.0407.0002
[Abstract + References] Feasibility of a rehabilitation robot using functional electrical stimulation technology in the treatment of hemiplegic gait foot droop after stroke – Conference Proceedings
Posted by Kostas Pantremenos in Functional Electrical Stimulation (FES), Gait Rehabilitation - Foot Drop, Rehabilitation robotics on December 22, 2022
ABSTRACT
Stroke is a very common disease. Hemiplegia is its sequela, but also a high disability rate of the disease. There have been some targeted rehabilitation training and rehabilitation treatment in medicine, but the effect is not obvious or has some limitations. This paper introduces a new kind of rehabilitation robot for this disease, and uses the functional electrical stimulation technology in rehabilitation to realize the treatment and training of this kind of patients. Through the analysis and discussion of the technology and the application of the rehabilitation robot, the feasibility and effectiveness of this kind of robot are verified. Strive to provide new ideas for the rehabilitation of such diseases.
REFERENCES
- 1.Mayo E., Wood-Dauphinee S., Sar, et al. Disablement following stroke[J]. Disability & Rehabilitation, 1999, 21(5-6):258–268. https://doi.org/10.1080/096382899297684, Google ScholarCrossref
- 2.Moseley A., Wales A., Herbert R., et al. Observation and analysis of hemiplegic gait: stance phase[J]. Australian journal of physiotherapy, 1993, 39(4): 259–267. https://doi.org/10.1016/S0004-9514(14)60486-4, Google ScholarCrossref
- 3.Moore S., Schurr K., Wales A., et al. Observation and analysis of hemiplegic gait: swing phase[J]. Australian journal of physiotherapy, 1993, 39(4): 271–278. https://doi.org/10.1016/S0004-9514(14)60487-6, Google ScholarCrossref
- 4.Wall J. C., Turnbull G I. Gait asymmetries in residual hemiplegia[J]. Archives of physical medicine and rehabilitation, 1986, 67(8): 550–553. Google Scholar
- 5.Lynch C. L., Popovic M R. Functional electrical stimulation: closed-loop control of induced muscle contractions. [C]// Agu Fall Meeting. AGU Fall Meeting Abstracts, 2012. Google Scholar
- 6.Sharif F., Ghulam S., Malik A. N., et al. Effectiveness of functional electrical stimulation (FES) versus conventional electrical stimulation in gait rehabilitation of patients with stroke[J]. J Coll Physicians Surg Pak, 2017, 27(11): 703–706. Google Scholar
- 7.Weber D. J., Stein R. B., Chan K. M., et al. Functional electrical stimulation using microstimulators to correct foot drop: a case study[J]. Canadian journal of physiology and pharmacology, 2004, 82(8-9): 784–792. https://doi.org/10.1139/y04-078, Google ScholarCrossref
- 8.Horprasert T., Haritaoglu I., Wren C., et al. Real-time 3d motion capture[C]//Second workshop on perceptual interfaces. 1998, 2. Google Scholar
- 9.Pfister A., West A. M., Bronner S., et al. Comparative abilities of Microsoft Kinect and Vicon 3D motion capture for gait analysis[J]. Journal of medical engineering & technology, 2014, 38(5): 274–280. https://doi.org/10.3109/03091902.2014.909540, Google ScholarCrossref
- 10.Langhorne P., Bernhardt J., Kwakkel G. Stroke rehabilitation[J]. The Lancet, 2011, 377(9778): 1693–1702. https://doi.org/10.1016/S0140-6736(11)60325-5, Google ScholarCrossref
[WEB] HARNESSING THE POWER OF HIGH-INTENSITY GAIT TRAINING
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop on October 19, 2022

BY MARY VAN DER MEER, PT, DPT, AND LAUREN WRIGHT, PT, DPT
THE RISE OF HIGH-INTENSITY GAIT TRAINING
Research has shown that high-intensity gait training—walking practice at intensities of 75% to 85% maximum heart rate—is the best way to promote neuroplasticity and optimize walking recovery after a neurological injury. High-intensity gait training has been shown to improve gait speed, walking distance, and balance. In acute inpatient rehabilitation, a patient walks, on average, fewer than 300 steps a day.1 After implementing a high-intensity gait training program, daily stepping increased to approximately 1,500 steps a day, which was also positively correlated to improved 6-minute walk test scores, improved Berg Balance Scores, improved gait speed, and decreased levels of assistance required at discharge.1 As more research is published, it is clear: we need to really push our patients for the best recovery after a neurological injury.
PHYSICAL DEMANDS OF A PHYSICAL THERAPIST
We also know that our job as physical therapists is very physically demanding. In a survey completed on physical therapists and physical therapist assistants, 32% experienced a work-related injury within the past year.2 Of the work-related injuries, 50% involved the low back, 21% involved the wrist, 14% involved the shoulder, and 15% involved the head/neck.2 The most common causes of work-related injuries are not surprising: 53% of injuries were from transfers/lifting, 9% from functional activities, 7% from patient falls, and 7% from manual therapy.3 Manual facilitation and hands-on assistance throughout a day of work can result in long periods of awkward postures, heavy lifting, and repetitive forceful tasks. Work-related injuries are also very expensive. On average, a worker’s compensation claim related to patient handling costs $15,600,4 and this number does not account for employee turnover and training, productivity impacts, and effects on morale.
As our practice shifts to include high-intensity gait training, and as our acute care hospital lengths of stays continue to decrease, physical therapists are expected to push more-involved patients harder than ever before. At the same time, physical therapists are already at higher risk for work-related injuries due to the very physically demanding nature of the job. How can physical therapists stay safe, yet be able to effectively do their jobs of pushing high-intensity gait training on more involved and complex patients?
PRODUCT RESOURCES
The following companies provide technologies that can be useful in the treatment of stroke and neurological conditions:
Allard USA Inc
www.allardusa.com
Biodex
www.biodex.com
DIH Technology
www.dih.com
CIR Systems Inc/GAITRite
www.gaitrite.com
Mobility Research Inc
www.litegait.com
ProtoKinetics
www.protokinetics.com
Vista Medical
www.boditrak.com
DIFFERENT GAIT TRAINING DEVICES
Overhead harness systems inherently increase patient and provider safety, as the patient’s body weight is supported by the machine, allowing the patient increased freedom of movement while minimizing the risk of injury to patient and therapist. This allows the therapist to provide hands-on assistance and facilitation as needed to support limb advancement, stance stability, and lateral weight shifting. In addition, the patient is not reliant on the therapist’s ability to support their body weight, allowing for increased opportunities to practice stepping at the recommended intensity. A variety of overhead harness systems are available for clinic use and vary in design, cost, size, height-weight capacities, degrees of vertical displacement, and environmental requirements.
For example, the LiteGait from Mobility Research Inc, Tempe, Ariz, and Biodex NxStep Unweighting System from Shirley, NY-based Biodex are freestanding harness systems with four wheels that offer bilateral upper extremity support if needed that can be pushed or pulled by the patient or therapist overground. The ZeroG Gait and Balance System from Aretech, Ashburn, Va, is a single-point harness that uses a ceiling track, which makes it a more versatile harness system, as it can be used over virtually any surface. The Andago from Minneapolis-based DIH Technology is a robotic harness system that is used only overground where the speed and direction can be controlled with a remote by the therapist or the patient through detection of their movement. As compared to other systems, the Andago and the ZeroG have an increased vertical displacement range, allowing the patient to be more dynamic in a safe environment.

Overhead harness systems, including the single-point-harness Biodex NxStep, can be used for gait training as well as obstacle negotiation and pre-stair training.
ENVIRONMENTAL CONSIDERATIONS
An important factor in device selection includes the gym set-up and design, as some overhead systems utilize a ceiling track, whereas others are freestanding. The height of the gym ceilings and doorways are important to assess, as some of the devices are able to accommodate changes in ceiling height, whereas others are at a fixed height.
The Litegait, Biodex NxStep, and the ZeroG can be utilized overground and over a treadmill, whereas the Andago is utilized only overground due to the robotic technology that allows the therapist to control the speed and direction of the device with a remote. All of the devices mentioned can be used for gait training, obstacle negotiation, and pre-stair training. The number of clinicians and support staff required for the treatment session will vary for each device depending upon the level of assistance the patient requires, which is an additional consideration when selecting a device.
SINGLE-POINT VS 4-POINT
When evaluating which device to utilize, it is important to consider how much support the patient will need from the harness system, as the harness design and how the body weight is supported will influence the amount of available trunk support and available degrees of freedom. A single-point harness system, such as the Biodex NxStep Unweighting System or the ZeroG, allows for increased degrees of freedom, as the patient can turn 360 degrees in the harness, allowing for dynamic turns and multi-directional stepping.
A four-point harness, such as the LiteGait or the Andago, allows for increased stability and asymmetrical unweighting. Asymmetrical unweighting is useful for treating patients who present with decreased weight-bearing through a lower extremity due to pain or weakness, impaired lateral weight-shifting abilities, impaired midline, or contraversive pushing behaviors.
CONSIDERATIONS
It is important to note that although overhead bodyweight support harness systems are beneficial for most patients, not all patients are appropriate for harness use. Some contraindications include pregnancy, rib fractures, graft sites, and wounds that would be directly impacted by harness placement.5 Precautions should be taken for PEG tubes, baclofen pumps, catheters, colostomy bags, and uncontrolled orthostatic hypotension.5
Therapists can use towels or foam padding to off-load any area of potential concern. However, it is important to reference each device manual for specific contraindications and precautions prior to initial use. When new to an overhead harness system, it may take increased time or additional assistance for set-up, but with time and experience, set-up time will become more efficient.
CONCLUSION
These overhead systems are expensive, but in our opinion a worthy investment when factoring in patient and therapist safety, as the patient’s ability to participate in high-intensity gait training is not solely dependent on the therapist for physical support. Additionally, these devices can increase patient confidence and their willingness to try challenging activities that otherwise might induce fear due to risk of falling. These devices help to prevent injury to patients and therapists. They also allow for the patient to participate in upright activities for longer periods of time and relearn how to regain their mobility as they progress and achieve their goals. PTP
Mary van der Meer, PT, DPT, and Lauren Wright, PT, DPT, are both Board-Certified Clinical Specialists in Neurologic Physical Therapy at the Kessler Institute for Rehabilitation, Saddle Brook Campus. For more information, contact PTPeditor@medqor.com.
REFERENCES
- Hornby TG, Holleran CL, Leddy AL, et al. Feasibility of Focused Stepping Practice During Inpatient Rehabilitation Poststroke and Potential Contributions to Mobility Outcomes. Neurorehabil Neural Repair. 2015;29(10):923-932. doi:10.1177/1545968315572390
- McCrory, B, Burnfield, J Darragh, A, et al. (2014). Work Injuries Among Therapists In Physical Rehabilitation. Proceedings of the Human Factors and Ergonomics Society Annual Meeting. 58. 1072-1076. 10.1177/1541931214581224.
- Darragh AR, Campo M, King P. Work-related activities associated with injury in occupational and physical therapists. Work. 2012;42(3):373-384. doi:10.3233/WOR-2012-1430
- https://www.osha.gov/sites/default/files/publications/OSHA3279.pdf
- https://www.litegait.com/page/contraindications
FEATURED IMAGE CAPTION: A four-point harness, such as the Andago from DIH Technology, allows for increased stability and asymmetrical unweighting. Asymmetrical unweighting is useful for treating patients who present with decreased weight-bearing through a lower extremity This system is made to be used overground.
Related Content:
Gait Training to Music Offers Practice a Clinical and Competitive Advantage
[BLOG POST] 10 Foot Drop Exercises to Get Back on Your Feet with Confidence
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop on October 14, 2022
Medically reviewed by Andrew Tran PT, DPT, NCS, CSCS — written by Flint Rehab.

Foot drop is a general term for a condition resulting in difficulty lifting the front part of the foot and toes. It often results in difficulty walking, as the individual is at higher risk of falls if the foot drags or the toes get caught on the ground. Fortunately, there are ways to regain strength and mobility in the foot — and one of the best methods includes foot drop exercises.
Exercises for foot drop are designed to help strengthen the lower limb muscles to improve the ability to lift the foot up again. Exercise also helps stimulate and rewire the brain, which makes it an effective way to overcome foot drop after a stroke or brain injury.
Through this article, you’ll learn exercises that you can safely start doing at home. At the end, you’ll also discover other treatments for foot drop that can help boost your results even more.
Table of contents
- How physical therapy helps foot drop
- Foot drop exercises
- Exercise video for foot drop
- Additional rehabilitation methods for foot drop
How Does Physical Therapy Help Foot Drop?
Foot drop (also called drop foot) is a condition that impairs your ability to lift the top part of your foot (and our toe area) up toward your shin. This movement is known as dorsiflexion, and it’s important for walking properly and maintaining balance.
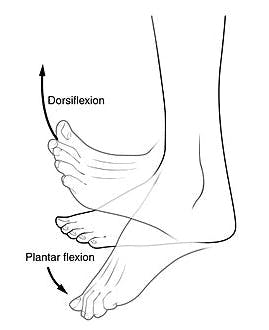
Image credit: Wikipedia
To move your muscles, the brain must send signals that tell your muscles when to contract and relax. When a brain injury or stroke affects the areas of the brain that sends these signals, it can lead to foot drop. However, foot drop can also occur due to damage to the muscles or nerves in the lower leg that directly perform dorsiflexion, or the nerve roots originating from the lumbar spine (specifically L4 and L5).
Foot drop exercises help strengthen the muscles in the area and rewire the brain to improve your brain’s ability to send the correct signals to move your foot. This rewiring process is known as neuroplasticity, and it’s key to foot drop recovery.
Consistent practice of therapeutic exercises and movement retraining provides the brain with the stimulation it needs to relearn the skill of dorsiflexion. Most physical therapists send patients home with a sheet of exercises to practice on their own at home to provide the brain with the repetition it needs to recover.
Now that you know why exercises for foot drop are important, let’s start exercising.
Foot Drop Exercises for At-Home Physical Therapy
The following foot drop exercises feature physical therapist Liliana, DPT. She’s the same therapist that guides our leg exercises on YouTube.
Liliana has experience helping patients with foot drop regain mobility using these exact exercises. Here are some of her best physical therapy exercises for foot drop, organized from easiest to hardest:
1. Ankle Dorsiflexion


Start this passive foot drop exercise with your affected leg still crossed over your other leg. Then, use your non-affected arm to move your foot into dorsiflexion. This is the exact movement that people with foot drop struggle with, so this exercise is a perfect starting point. If you struggle with getting into this position, or have difficulty reaching your hand to your foot, you can also wrap a towel or belt around your foot to perform the movement.
This is a passive movement, which is a great starting point for anyone struggling with extremely limited mobility. It will also help reduce the chances of your foot and ankle muscles becoming stiff from lack of movement.
2. Ankle Adduction/Abduction


For another great passive foot drop exercise, cross your affected leg over your other leg. Then, use your non-affected hand to move the front part of your foot side to side. Focus on initiating all the movement from your ankle.
Passive exercises are great for patients with severely limited mobility. If you already have some movement, then add some challenge by doing the exercise without assistance from your hand (i.e. “active exercise”).
3. Assisted Toe Raises


Toe raises are the most difficult movement to perform with foot drop. If you have difficulty with this movement — that’s okay! Fortunately, this is another passive exercise that you can use to help spark neuroplasticity and rewire the brain.
Start by placing your affected foot on top of your non-affected foot. Then, use your non-affected foot to lift your foot up. Use slow, intentional movements to help stimulate the brain. This can be done passively with your foot completely relaxed, or active-assisted as you consciously attempt to dorsiflex with the help of your other foot.
Lift your foot up and down during this exercise a total of 10 times or more.
4. Toe Raise “Negatives”
A “negative” exercise involves emphasizing the eccentric part of a movement. With the previous Toe Raise exercise, the eccentric part of the movement is lowering your foot back down.
During this exercise, we will emphasize only the eccentric part of the movement.
Start by lifting your affected foot up into a flexed position (toes towards your shin), just like in the Toe Raise exercise. But this time, instead of dropping your foot back down quickly, try to lower your foot as slowly as you can.
This move is more advanced, because it does require some control of your foot. Try doing this a total of 10 times before moving onto the next foot drop exercise.
Want 13 pages of foot drop exercises in a beautiful PDF? Click here to download our free Stroke Rehab Exercise ebook now (link opens a pop up for uninterrupted reading)
5. Heel Raises


This active foot drop exercise is the opposite of toe raises. Although this may not feel like it’s helping with foot drop, it will help train the surrounding muscles.
To perform heel raises, start with your feet flat on the ground. Then, point your toes and lift your heels off the ground. Try to keep proper neutral foot alignment by pressing actively through your 1st and 2nd toes, making sure not to let your ankles turn outwards during the heel raises. You should feel the muscles in the calf and lower back of the leg working. Repeat 10 times.
6. Ankle Eversion


For this active foot drop exercise, place your affected foot flat on the ground. Then, lift the outside edge of your foot and toes up, then relax back down.
Focus on isolating the movement from your foot and ankle and try to avoid compensating with your leg. Repeat 10 times.
7. Ankle Inversion
For ankle inversion, start in the same position but move the inside edge of your foot and toes up towards the midline of your body, then relax back down. Repeat 10 times.
8. Single Leg Stance
Standing on one foot is another great way to exercise ankle eversion and challenge your ankle stability in general.
Patients with foot drop who have enough strength and balance can try to stand on their affected leg for 15 seconds at a time. Be sure to hold onto the back of a chair for stability so that you don’t fall. Balance only improves when stability is challenged, so only use as much hand support as needed for safety.
9. Hip External and Internal Rotation


Although this exercise targets the upper leg and hip, it’s also helpful for foot drop because increased tone (stiffness) in the leg can also affect the foot.
Start this lower limb exercise in a seated position. Then, kick your affected leg inward toward your midline (hip external rotation). Then, kick your affected leg outward (hip internal rotation), like you’re kicking a ball to the side. Repeat back and forth.
This exercise helps with foot drop because improving mobility in the leg has a trickle-down effect into the feet.
10. Hip Rotation Slides


To finish up these foot drop exercises, try this gross motor exercise for the lower limbs.
In a seated position, start with a towel underneath your affected foot. Then, use your arm to assist your affected leg and slide your leg and toes towards your midline (internal rotation). Then, push your leg and slide your leg and toes outwards (external rotation).
You can also perform this exercise by sliding the whole affected leg inward (adduction) to bring the legs closer together, and outward (abduction) to separate the legs.
These last two foot drop exercises target the legs, which can be helpful for patients with severe foot drop when it’s coupled with other lower limb impairments.
Watch More: Foot Drop Exercise Video
If you want more visual guidance, here’s a great YouTube video with foot drop exercises from well-known physical therapists.

Bob & Brad are popular physical therapists on YouTube. While they don’t specialize in stroke rehab like Liliana, their video contains similar exercises, like eccentric movements and hip adduction.
Pick and choose the exercises that are most comfortable for you to start with, and work your way up from there. Ideally, it’s best to work with your own therapist to address concerns with foot drop, and continue exercising at home between therapy sessions.
If your insurance covers outpatient therapy, it may be worth it to schedule an appointment with a physical therapist. PT’s understand the complexities of the human body and can provide additional exercises, balance and gait training not covered in this article.
How to Supplement Your Foot Drop Exercises
Foot drop exercises aren’t the only way to recover from foot drop. In fact, recovery often occurs faster when multiple rehabilitation treatments are pursued.
Below, you’ll find the most popular treatments listed from least invasive to most invasive. Talk to your therapist to see which recommendations are suitable for you.
Passive Exercise
Passive exercise is a great foot drop treatment for anyone that has zero mobility in their foot. As seen in the first exercise above, exercising passively involves assisting your foot through the movement. This helps reduce the risk of getting a joint contracture or worsening stiffness, and can improve blood flow and activate neuroplasticity to help recover from foot drop after a neurological injury like stroke.
Want 13 pages of foot drop exercises in a beautiful PDF? Click here to download our free Stroke Rehab Exercise ebook now (link opens a pop up for uninterrupted reading)
At-Home Rehab Exercise Equipment
Many patients struggle with practicing foot drop exercises at home. Not because they don’t know what to do (after all, there are a dozen ideas in this article alone), but because they don’t have the motivation or accountability.
This issue is solved with high-tech rehab exercise equipment like Flint Rehab’s FitMi home therapy. The device turns that written sheet of exercises into an interactive experience that helps motivate you to exercise. See how a stroke patient named Ron regained foot mobility with FitMi:

“With the FitMi, I have immediate feedback and also weekly feedback on how well I am doing. I am having great fun with this product. I have noticed real-world results as well. I drive one-footed now rather than two-footed because I can target the gas pedal and the brake with my right foot. I can target the cruise control set button with my right hand. These accomplishments are due to the exercises and feedback of the FitMi.”
-Ronald
Electrical Stimulation
Aside from foot drop exercises, electrical stimulation is one of the best complimentary treatments for mobility issues after stroke. Electrical stimulation involves applying electrical currents through the skin to the nerves and muscles. It has been shown to help improve foot drop and gait in stroke patients.
Many studies show that combining electrical stimulation with rehab exercise leads to even better results. It is important to recognize that the research is specifically looking at the effects of neuromuscular electrical stimulation (NMES) or functional electrical stimulation (FES) using specific parameters to help facilitate motor recovery. This differs greatly from transcutaneous electrical nerve stimulation (TENS) which is primarily for pain control.
Work with a physical therapist to learn what electrical stimulation device is most appropriate, how to adjust the settings, and where to place the electrodes. Depending on which muscles or nerves are affected in the foot and leg, they will adjust accordingly.
Ankle Foot Orthotics

Ankle foot orthotics offer support to the foot so that it doesn’t drag on the floor, which helps reduce the risk of tripping and falling. Foot drop braces are notorious for having low compliance rates, though, because they can be uncomfortable. But if your therapist suggests wearing an AFO, you need to wear one to prevent the risk of falling and fracturing a hip, or worse.
Also, be aware that when the foot and lower leg muscles are neglected, you run the risk of worsening the weakness and foot drop condition (“use it or lose it”). To prevent foot drop from worsening, the use of an AFO should always be accompanied with gait training and consistent foot drop exercises to encourage recovery and keep the brain stimulated.
Surgery
If foot drop has not improved after consistent, long-term rehabilitation, nerve transfers can be considered. This surgery works by taking donor “redundant nerves” from other parts of the body and transferring them to the affected area.
Surgery is an invasive treatment that should be a last resort. Usually, doctors recommend surgery if foot drop has not improved after 6-12 months of consistent rehabilitation. Following nerve transfers, it can take anywhere from a few months to years of additional rehabilitation to retrain the motor function, but results have been promising in this relatively novel intervention.
Stimulate the Brain with Foot Drop Exercises
The first line of defense against foot drop is rehab exercise. Regular, consistent practice helps rewire the brain and improve mobility in the foot and lower extremities.
By combining rehab exercise with other techniques, like electrical stimulation, gait and balance retraining, patients can boost recovery further. When foot drop is severe, patients can start with passive exercise and work their way up from there and may consider an AFO or even surgery if the condition is not improving.
We hope this guide has helped you understand your options for overcoming foot drop.
You’re on a Roll: Get Free Foot Drop Exercises in a Beautiful PDF!
Get our free ebook filled with 14 pages of foot drop exercises featuring photos of licensed therapists. Sign up below to get your copy! We never sell your email address, and we never spam. That we promise.
Exercises to Try at Home Click here to get instant access.
[WEB] “Breakthrough” wearable bionic leg improves mobility outcomes in trials
Posted by Kostas Pantremenos in Artificial intelligence, Gait Rehabilitation - Foot Drop on July 21, 2022

Marrying together inclusive design with pioneering mobility technology, a new wearable bionic leg is looking to make waves in the assistive technology space.
Cionic Neural Sleeve uses artificial intelligence (AI) to understand and influence human mobility in real-time, enabling greater access and independence for those with reduced mobility, such as individuals with multiple sclerosis, stroke, and cerebral palsy.
Cionic, which creates bionic clothing that can analyse and augment human movement, partnered with an acclaimed designer, Yves Behar, and his design firm, fuseproject, to launch the wearable bionic leg.
The sleeve is designed for everyday wear. Importantly, it is easy to put on and take off, which is imperative for individuals with restricted mobility.
The lightweight, breathable fabric has a similar feel to sports leggings, according to Cionic, and is available in multiple colours and sizes. Paired with the intuitive Cionic app, the sleeve enables the user to be in control of their own mobility journey.
Cionic Neural Sleeve has demonstrated an improvement in mobility outcomes during user trials.
Cionic trial participants across multiple locations demonstrated strong improvement on the two key measures associated with foot drop: dorsiflexion at heel strike (94 percent of users), and ankle inversion during swing (88 percent of users). Notably, when combining the two measures, there was an average improvement of 9° for participants, the firm underlines.
Cionic Founder and CEO Jeremiah Robison, said: “Building bionic clothing that can augment human movement takes a thoughtful and holistic approach. It starts with advanced technology capable of adapting to each user’s mobility needs to deliver meaningful outcomes.
“Then we designed it to be comfortable to wear and effortless to use. From software to soft goods, our team of experts have pushed the boundaries of human-machine interface to deliver the future of assistive technology.
“Ultimately we are creating not just a single solution, but a platform for bionic clothing that can analyse, predict, and augment human movement for all.”
The wearable leg prioritises user experience. Alongside improving mobility and independence, the design strives to help wearers overcome some of the emotional upset that can come with having reduced mobility.
To achieve this, Cionic and fuseproject worked with potential users to understand their needs and create “the best possible solution”.
Dr. Jacqueline Nicholas, System Chief Neuroimmunology and Multiple Sclerosis at the OhioHealth MS Center, has been an advocate for the Cionic Neural Sleeve, seeing two of her multiple sclerosis patients walk better than they had in ten years after programming the device to their needs.
“This is the first comprehensive system that addresses key muscle groups of the leg, which means it has the potential to improve mobility and function with continued use,” she enthused. “It’s unlike anything I’ve ever seen.”
Home usability trials were also conducted to understand the impact of the bionic leg on mobility over time. Not only has reported mobility improved for many of these users, Cionic notes, but the number of users experiencing moderate-to-severe pain was reduced by 60 percent, and the number of users experiencing moderate to severe anxiety or depression was reduced by 75 percent.
Beverly Chaidez, who has multiple sclerosis and participated in the home usability trials, described her experience with the Neural Sleeve: “When I started the home usability trial I was only able to walk for about five to 10 minutes at a time, and I used a wheelchair for mobility outside of the home.
“Today, I can walk for 40 to 50 minutes at a time and I haven’t used my wheelchair in over a month. I feel hopeful and optimistic that I can regain a lot of things that I lost.”
Cionic is now accepting pre-orders on its website for early 2023 delivery in the USA. The firm told AT Today that after it has launched in the USA, it will explore launching the sleeve internationally.
[ARTICLE] Spatiotemporal, kinematic and kinetic assessment of the effects of a foot drop stimulator for home-based rehabilitation of patients with chronic stroke: a randomized clinical trial – Full Text
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, Tele/Home Rehabilitation on June 15, 2022
Abstract
Background
Gait disability affects the daily lives of patients with stroke in both home and community settings. An abnormal foot–ankle position can cause instability on the supporting surface and negatively affect gait. Our research team explored the ability of a portable peroneal nerve-targeting electrical stimulator to improve gait ability by adjusting the foot–ankle position during walking in patients with chronic stroke undergoing home-based rehabilitation.
Methods
This was a double-blinded, parallel-group randomized controlled trial. Thirty-one patients with chronic stroke and ankle–foot motor impairment were randomized to receive 3 weeks of gait training, which involved using the transcutaneous peroneal nerve stimulator while walking (tPNS group; n = 16, mean age: 52.25 years), or conventional home and/or community gait training therapy (CT group; n = 15, mean age: 54.8 years). Functional assessments were performed before and after the 3-week intervention. The outcome measures included spatiotemporal gait parameters, three-dimensional kinematic and kinetic data on the ankle–foot joint, and a clinical motor and balance function assessment based on the Fugl–Meyer Assessment of Lower Extremity (FMA-LE) and Berg Balance scales (BBS). Additionally, 16 age-matched healthy adults served as a baseline control of three-dimensional gait data for both trial groups.
Results
The FMA-LE and BBS scores improved in both the tPNS groups (p = 0.004 and 0.001, respectively) and CT groups (p = 0.034 and 0.028, respectively) from before to after training. Participants in the tPNS group exhibited significant differences in spatiotemporal gait parameters, including double feet support, stride length, and walking speed of affected side, and the unaffected foot off within a gait cycle after training (p = 0.043, 0.017, 0.001 and 0.010, respectively). Additionally, the tPNS group exhibited significant differences in kinematic parameters, such as the ankle angle at the transverse plane (p = 0.021) and foot progression angle at the frontal plane (p = 0.009) upon initial contact, and the peak ankle joint angle at the transverse plane (p = 0.023) and foot progression angle (FPA) at the frontal and transverse planes (p = 0.032 and 0.046, respectively) during gait cycles after 3 weeks of training.
Conclusions
Use of a portable tPNS device during walking tasks appeared to improve spatiotemporal gait parameters and ankle and foot angles more effectively than conventional home rehabilitation in patients with chronic stroke. Although guidelines for home-based rehabilitation training services and an increasing variety of market devices are available, no evidence for improvement of motor function and balance was superior to conventional rehabilitation.
Background
Stroke is one of the five leading causes of disability-adjusted life-years worldwide [1]. In China, the increasing incidence of stroke and decrease in related mortality have led to a rapid increase in the burden of society [2]. Gait dysfunction is common among stroke survivors and represents a major burden, while the community commonly might provide no more than 1-year’s rehabilitation service due to lack of therapists [3, 4]. After stroke, most patients experience abnormal lower extremity movement and a plantarflexion or inversion pattern of hemiplegia in the ankle and foot during the swing phase of gait [5]. Estimates suggest that 20–30% of stroke survivors experience ankle and foot drop and/or inversion, which causes abnormal gait [4]. Ankle–foot drop and inversion are caused by abnormal activation of the musculature in the distal lower limb and result in inefficient foot clearance and foot tremor during the swing phase of gait and a less stable stance. Consequently, stroke patients tend to exhibit a compensatory gait pattern involving the affected side, such as steppage gait, hip hiking, toe walking, and forefoot walking. These pathological deviations reduce the walking speed and increase the risk of fall, thus impeding an individual’s ability to walk efficiently both indoors and outdoors and restricting their participation in many activities of daily life and the community. Therefore, studies on stroke motor recovery have frequently identified inadequate ankle–foot control and stability during walking as a key factor to address when attempting to improve gait dysfunction [6,7,8,9].
Approaches such as ankle–foot orthosis (AFO), electrical stimulation (ES), and neuroprosthetic implants are used to treat drop foot in stroke survivors [10,11,12], and a meta-analysis revealed that these approaches yielded similar results [12]. AFO is a traditional treatment for ankle joint immobilization in the neutral position and can be used to support ankle dorsiflexion during the swing phase to improve gait stability. However, as a mechanical device, an static AFO only restricts ankle movement when it is worn, leading to no improvement of muscle activety,, reduced muscle activity and a restricted ankle range-of-motion higher possibility of falling over the long term [13, 14]. ES, an alternative approach, is widely used to achieve more physiological positioning of the ankle and foot and to improve ankle–foot function, for example neuromuscular electrical stimulation (NMES), functional electrical stimulation (FES) multichannel and neuroprosthetic implants with the development of electronic engineering technology [8, 15,16,17], but multichannel and implanted devices are not used widely in the clinical settings, which limits their translational use in community and home settings.
Studies conducted in the last 10 years have focused on volitional muscle activation combined with lower motor neuron stimulation, which contributes to several possible mechanisms of neuromuscular plasticity, including repeated muscle contractions leading to increased oxidative capacity; increased numbers of microcapillaries and changes in fiber type at the muscular level; and the convergence of orthodromic or antidromic impulses at the anterior horn, leading to the strengthening of synapses at the spinal level and changes in the cortex [17,18,19]. These effects of therapy culminate in increased volitional muscle activity in the weak dorsiflexors and evertors of the ankle. Such changes are thought to positively influence other biomechanical features and help restore the associated functions. Several studies have observed sustained improvements in volitional muscles after removal of therapeutic devices, particularly in terms of improved gait capacity during the chronic post-stroke stage [19,20,21]. One type of FES treatment, the transcutaneous peroneal nerve stimulator (tPNS), involves the placement of electrodes on the skin surface above the peroneal nerve, and based on the mechanisms of effects on volitional muscle activity combined with lower motor neurone stimulation during walking to acquire a more physiological positioning of ankle and foot. This clinically accepted rehabilitation intervention has been demonstrated to be more efficient than AFO, especially in terms of improving walking speed [22, 23]. However, a multicenter prospective randomized study found that the use of peroneal nerve FES was equivalent to device-free gait training in terms of the clinical outcomes of improvements in walking speed, the Fugl–Meyer Assessment of Lower Extremity (FMA-LE) score, ankle muscle strength and dorsiflexion performance [24].
Above studies in different views of the tPNS suggest that this therapeutic device is an appropriate alternative therapeutic device using at chronic stroke survivors for gait training. Other studies have focused on the physiological and biomechanical effects of tPNS on the kinematics and kinetics of the hip, knee, and ankle joints [16, 22, 25]. However, excessive pronation and supination of the foot and hyper-planta/dorsiflexion of the ankle joint directly result in an abnormal and unstable stance and toe clearance during walking, leading to a tilted posture and increasing the fall risk. The evidence so far for improvement of foot activity is still limited, especially its biomechanical analysis. This study focused on quantitative analysis of both kinematics and kinetics of the ankle joint and foot progression angles (FPA) and spatiotemporal gait and clinical assessment parameters. We aimed to determine the efficacy of tPNS among chronic stroke population and its feasibility for use as a rehabilitation training tool in home and community settings. This is important because most discharged stroke patients in China receive inadequate rehabilitation training at home due to a shortage of rehabilitation therapists.
Therefore, in our study, some chronic stroke patients discharged were recruited to randomized into two groups, including the home-based or community-based gait training was arranged via tPNS or self-training without tPNS with therapist’s guidance lasted for 2 h each day during 3 weeks. The results of gait parameters and clinical assessment outcomes were compared between groups before and after interventions.[…]

[WEB] Gait MyoElectric Stimulator: New from Innovation Lab
Posted by Kostas Pantremenos in Functional Electrical Stimulation (FES), Gait Rehabilitation - Foot Drop on April 13, 2022
Posted by Deborah Overman

Innovation Lab, Innovation Institute’s national health care incubator, and MultiCare Health System, a Washington state not-for-profit health care organization, announce the development of the Gait MyoElectric Stimulator (GMES), a unique functional electrical stimulation device that uses dual stimulator technology to help improve walking ability in patients with neuromuscular conditions such as stroke, cerebral palsy and multiple sclerosis.
The first-generation device was developed and tested in the clinic by David Embrey, PT, PhD, a physical therapist and founder of MultiCare’s Good Samaritan Children’s Therapy Unit’s Movement Laboratory; Gad Alon, PT, PhD, associate professor emeritus of physical therapy and rehabilitation science at the University of Maryland School of Medicine; and Jeffrey Stonestreet, retired senior electrical design engineer for the Boeing Company.
Next steps for Innovation Lab and MultiCare are to secure an industry partner to add GMES to their product portfolio and bring this solution to market to help the millions of stroke survivors and people living with neuromuscular conditions.
“There are 4 million Americans each year who have a stroke,” Dr. Embrey says. “When we think of something coming from this little community hospital that impact hundreds of thousands of individuals in the country, and perhaps around the world, that’s very exciting.”
“The Innovation Lab is thrilled to work with member organization MultiCare on the development of GMES, which will improve quality of life for patients with neuromuscular conditions,” Innovation Lab General Manager Ryan Kelly says. “The GMES team’s work is a shining example of how the Lab taps into the innovative potential of healthcare employees, turning doers into dreamers.”

GAIT MYOELECTRIC STIMULATOR: A WEARABLE DEVICE FOR HEMIPLEGIA OR HEMIPARESIS
Applied to the lower leg of patients with these conditions, GMES is an intuitive, wearable device for patients with hemiplegia or hemiparesis (paralysis or weakness on one side of the body), the most common physical consequence of stroke. GMES provides stimulation from multiple channels to opposing muscles, with that dual stimulation designed to improve post-stroke gait.
Current functional electric stimulation (FES) devices seek to treat only one symptom of hemiplegia: foot drop (an inability to raise the front of the foot). Simply lifting the foot does not smooth a patient’s halted gait, so a significant limp persists.
GMES is different: It mimics normal walking function with dual stimulation — dorsiflexion and plantar flexion — plus motion sensors designed for gait and stability improvement. GMES shows potential to help patients relearn how to walk independently, without long-term dependence on the device. (Clinical data from two published studies is on file.)
Innovation Lab partnered with MultiCare in 2021 to complete development and commercialize the GMES device, leveraging the Lab’s team of experts in medical device product development and commercialization. Innovation Lab is currently working with Dr. Embrey and colleagues to build upon the first-generation device to improve the ease of use and comfort of the device, with the aim of partnering with an industry partner that can scale manufacturing, sales, and distribution of GMES to make it widely available to patients in need.
[WEB] Cionic Neural Sleeve Receives FDA Clearance
Posted by Kostas Pantremenos in Functional Electrical Stimulation (FES), Gait Rehabilitation - Foot Drop on March 14, 2022

Cionic’s first product offering, the lightweight leg-worn Cionic Neural Sleeve, has been granted FDA clearance for “functional electrical stimulation to assist in gait for people with foot drop and leg muscle weakness,” the company announces.
This FDA clearance allows Cionic to take its Neural Sleeve to market and begin actively helping people with mobility issues due to multiple sclerosis (MS), stroke, cerebral palsy (CP), and other neurological conditions. The Cionic Neural Sleeve combines movement analysis and augmentation into a wearable garment.

“We are incredibly excited for the Cionic Neural Sleeve to be an FDA cleared Class II medical device and are ready to start impacting the lives of individuals with movement challenges in meaningful ways,” says Jeremiah Robison, Founder and CEO of Cionic. “Our mission is to become the new standard of care by addressing the underlying brain body connections, enabling confident movement, and greater engagement in the community.”
The lightweight and durable Neural Sleeve is designed to help people walk, a fundamental activity key to independent living. However, Cionic has built its platform from the ground up to enable solutions across the mobility spectrum. Cionic completed human factors and efficacy testing and submitted the Neural Sleeve for FDA clearance in November 2021.
“This would not have been possible without the more than 70 individuals across multiple sclerosis, stroke, cerebral palsy, and spinal cord injury who participated in our trials. Together with our research partners at Cleveland State University we were able to demonstrate statistically significant improvement to foot clearance, leading to more stable and confident walking,” Robison continues.

Jim Vecchi, who has been participating in Cionic’s MS trials, describes his experience with the Neural Sleeve.
“Wearing the Neural Sleeve, I move in a way that is more flowing and natural. I am walking more quickly and smoothly, while using less energy in doing so. Already I feel that I am getting stronger and more endurant,” he says. “I should also mention that the Neural Sleeve is surprisingly comfortable and my body has become accustomed to wearing it surprisingly quickly. I do not have the words to properly explain the positive effects on my confidence and outlook. I very much look forward to seeing what progress I can make with the help of the Neural Sleeve.”
To pre-order the Neural Sleeve for delivery later this year visit Cionic to join the Founder’s Program.
[Source: Cionic]
[VIDEO] Foot Drop Solutions – YouTube
Posted by Kostas Pantremenos in Functional Electrical Stimulation (FES), Gait Rehabilitation - Foot Drop, Video on December 4, 2021
PhysioFunction team discuss the benefits of Foot Drop Solutions at their clinic in Northampton
