Archive for June, 2021
[Book Chapter] Rehabilitation Progress of Arm VR Game Based on Hand Trajectory – Abstract/References
Posted by Kostas Pantremenos in Books, Paretic Hand, REHABILITATION, Video Games/Exergames, Virtual reality rehabilitation on June 30, 2021
Abstract
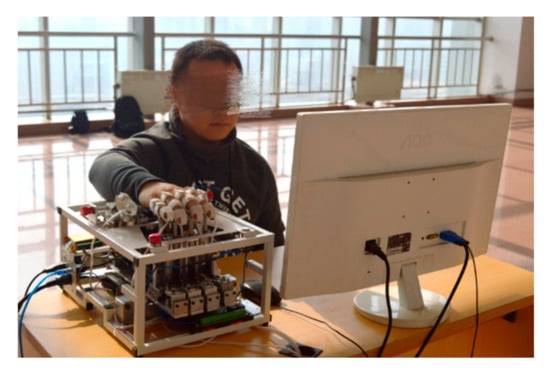
Long-term disability can reduce someone’s performance in activities or jobs. Although stroke is not the leading cause of disability, 75% of stroke survivors have decreased activity caused by disability. Serious long-term disability can be treated by using active movements, repetitive tasks, and task-oriented or movement sequences. Evaluation and monitoring the rehabilitation after stroke is the most crucial element to prevent the injury and determine the next step rehabilitation. This study will discuss monitoring arm movement for virtual reality (VR) game rehabilitation based on the trajectory movements. Five participants have contributed to data collection during three sessions and five repetition. Their movement recorded by using Kinect Xbox One sensor with data sampling 10 Hz. The mean absolute trajectory error (ATE) and hand speed movement methods are used to analyze the arm movement during the VR game. Although this study uses healthy subjects, 80% of them have an improvement in the movements, and this condition is proven by the reduced ATE value in each session. Trajectory data provides useful information about arm movements during the rehabilitation of VR games, including movement errors, hand position errors and hand speed to reach targets. Moreover, the mean ATE and hand speed movement able to provide clear information about the development of hand movements in completing the game.
References
- 1.Johnson W, Onuma O, Owolabi M, Sachdev S (2016) Stroke: a global response is needed. Bull World Health Organ 94(9):633–708CrossRefGoogle Scholar
- 2.Clinic M (2017) Stroke rehabilitation: What to expect as you recover. https://www.mayoclinic.org/stroke-rehabilitation/art-20045172
- 3.Vicky G, Charles RL, Garland SJ (2012) Factors that influence muscle weakness following stroke and their clinical implications: a critical review. Physiother Can 64(4):415–426CrossRefGoogle Scholar
- 4.Trombetta M, Henrique PPB, Brum MR, Colussi EL, Marchi ACBD, Rieder R (2017) Motion Rehab AVE 3D: A VR-based exergame for post-stroke rehabilitation. Computer Methods and Programs in Biomedicine, pp. 15–20Google Scholar
- 5.Kultu M, Freeman CT, Hallewell E, Hughes A-M, Laila DS (2016) Upper-limb stroke rehabilitation using electrode-array based functional electrical stimulation with sensing and control innovationsGoogle Scholar
- 6.Krabben T, Molier BI, Houwink A, Rietman JS, Buurke JH, Prange GB (2011) Circle drawing as evaluative movement task in stroke rehabilitation: an explorative study. Neuroeng Rehabil 8(15):1–11Google Scholar
- 7.Caby B, Stamatakis J, Laloux P, Macq B, Vandermeeren Y (2011) Multi modal movement reconstruction for stroke rehabilitation and performance assessment. Multimod User Interface 4(3):119–127CrossRefGoogle Scholar
- 8.Zhang Z, Fang Q, Gu X (2015) Objective assessment of upper limb mobility for post-stroke rehabilitation. IEEE Trans Biomed Eng 63(4):859–868Google Scholar
- 9.Yeh SC, Lee SH, Wang JC, Chen S, Chen YT, Yang YY, Chen HR, Hung YP (2012) Virtual reality for post-stroke shoulder-arm motor rehabilitation: training system & assessment method. In: 14th International Conference on e-Health Networking, Applications and Services (Healthcom), pp 190–195 (2012)Google Scholar
- 10.Cahyadi BN, Khairunizam W, Ibrahim Z, Razlan ZM, Bakar SA, Mustafa WA, Majid SH (2018) Analysis of EMG based arm movement sequence using mean and median frequency. In: International Conference in Electronics, Electrical, Computer, Science and Informatics, Malang – IndonesiaGoogle Scholar
- 11.Cahyadi BN, Khairunizam W, Majid SH, Ibrahim Z, Bakar SA, Razlan ZM (2018) Investigation of Upper Limb Movement for VR based Post Stroke Rehabilitation Device. International Colloquium on Signal Processing & its Applications, Penang – MalaysiaGoogle Scholar
- 12.B. N. Cahyadi, W. Khairunizam, D. S. Sanny, Z. Ibrahim, L. H. Ling, S. A. Bakar, Z. M. Razlan and W. A. Mustafa: Arm Games for Virtual Reality Based Post-stroke Rehabilitation. Lecture Note in Mechanical Engineering, pp. 91–101 (2020).Google Scholar
- 13.Rasidah SN (2017) Design of Arm Movement Sequence for Virtual Reality-Based Upper Limb Management After-Stroke. University Malaysia Perlis, PerlisGoogle Scholar
- 14.Pedraza-Hueso M, Martín-Calzón S, Díaz-Pernas FJ, Martínez-Zarzuela M (2015) Rehabilitation using kinect-based game and virtual reality. Procedia Comput Sci 75:161–168CrossRefGoogle Scholar
- 15.Shahrbanian S, Ma X, Aghaei N, Korner-Bitensky N, Moshiri K, Simmonds MJ (2012) Use of virtual reality ( immersive vs non-immersive) for pain management in children and adults: a systematic review of evidence from randomized controlled trial. Exp Biol 2(5):408–1422Google Scholar
- 16.Sturm J, Engelhard N, Endres F, Burgard W, Cremers D (2012) A benchmark for the evaluation of RGB-D SLAM system. In: Intelligent Robots and Systems, VilamouraGoogle Scholar
- 17.Zhang C, Liu Y, Wang F, Xia Y, Zhang W (2018) VINS-MKF: a tightly-coupled multi-keyframe visual-inertial odometry for accurate and robust state estimation. Sensors 18(11):1–29CrossRefGoogle Scholar
- 18.Jhon, D (2011) Introduction to Coordinate Geometry. https://www.mathopenref.com/coorddist.html. Accessed 26 June 2019
[ARTICLE] Mechanical Design and Analysis of the End-Effector Finger Rehabilitation Robot (EFRR) for Stroke Patients – Full Text
Posted by Kostas Pantremenos in Paretic Hand, REHABILITATION, Rehabilitation robotics on June 30, 2021
Abstract
Most existing finger rehabilitation robots are structurally complex and cannot be adapted to multiple work conditions, such as clinical and home. In addition, there is a lack of attention to active adduction/abduction (A/A) movement, which prevents stroke patients from opening the joint in time and affects the rehabilitation process. In this paper, an end-effector finger rehabilitation robot (EFRR) with active A/A motion that can be applied to a variety of applications is proposed. First, the natural movement curve of the finger is analyzed, which is the basis of the mechanism design. Based on the working principle of the cam mechanism, the flexion/extension (F/E) movement module is designed and the details used to ensure the safety and reliability of the device are introduced. Then, a novel A/A movement module is proposed, using the components that can easily individualized design to achieve active A/A motion only by one single motor, which makes up for the shortcomings of the existing devices. As for the control system, a fuzzy proportional-derivative (PD) adaptive impedance control strategy based on the position information is proposed, which can make the device more compliant, avoid secondary injuries caused by excessive muscle tension, and protect the fingers effectively. Finally, some preliminary experiments of the prototype are reported, and the results shows that the EFRR has good performance, which lays the foundation for future work.
1. Introduction
According to the World Health Organization (WHO), there are more than 15 million people around the world suffer strokes every year, and about 5 million of them are permanently disabled. Moreover, the global lifetime risk of stroke from the age of 25 years onward has increased from 22.8% in 1990 to 24.9% in 2016. Stroke is still the main cause of death worldwide [1,2,3]. Stroke causes damage to the nervous system, and can cause patients to lose part or all of their ability for activities of daily living (ADL), which brings a heavy burden to the family and society. Currently, the functional impairment of the fingers poststroke is rarely considered life-threatening. Together with the limited resources (time, cost, number of the caregivers and equipment etc.), it rates low on the priority of rehabilitation tasks [4,5,6]. In some ways, this increases the number of people with finger injury sequelae. Therefore, research on finger rehabilitation after stroke should be given more attention.Rehabilitation robots can assist poststroke patients with continuous, repetitive training with a standardized process, reducing the workload of therapists and providing more clinical options for patients. Hand rehabilitation robots can be divided into end-effector devices, exoskeletons and glove type in terms of wearing form [7]. Among all the end-effector devices, Amadeo [8,9] is the most commercially successful hand rehabilitation robot available. HandCARE [10] adopts ropes to fix fingers, and a clutch system is designed to allow all the fingers to be driven by only one motor. Rutgers Master II [11] is a four-degree-of-freedom pneumatically driven finger rehabilitation device which has been clinically tested. It achieves active flexion/extension (F/E) motion for four fingers, and the maximum output force can reach 16.4 N. Reha-Digit [12] is a passive rehabilitation device: patients need to put the fingers into four plastic roller sets during the training process. SAFE [13] drives the patient’s fingertips to do rehabilitation exercises by using rigid connecting rod structures. In addition, some universities have conducted researches on end-effector finger rehabilitation devices [14,15]. As for the exoskeletons, the robot developed by Gifu University [16] controls all of the fingers independently by arranging side-by-side dual motors on the back of the hand. The researchers at the University of Texas at Austin [17,18] applied the series elastic actuator (SEA) to finger rehabilitation. Their device uses Bowden cables to transmit power and obtains joint information through angle sensors, and it is lightweight and easy-to-wear by moving the motors outside of the back of the hand. The rehabilitation robotic exoskeleton hand [19] realizes finger F/E training through two worm gears, and passive pins are set to achieve adduction/abduction(A/A) motion simultaneously and a virtual reality system has been developed for rehabilitation scenarios. The Powered Finger–Thumb Wearable Hand Exoskeleton [20] adopts an under-driven cord control form and designed a self-alignment mechanism that prevents misalignment for the joints between the human and machine, besides, parallel mechanism has been attempt to applied on the hand rehabilitation [21]. The glove-type devices have developed significantly in recent years due to their good adaptability. Their driving form includes pneumatic [22,23], cord drive [24], layered reed drive [25,26,27] and so on.Force-based control is one of the control strategies for finger rehabilitation robots [28]. Cheng et al. [29] proposed a controller combing the iterative learning control (ILC) and the active disturbance rejection control (ADRC) to adapt the repeating training manner and overcome the external interference in a wearable hand rehabilitation robot. Park et al. [30] used proportional-integral-derivative (PID) control to design a control strategy capable of automatically switching between position and force control. Chiri et al. [31] utilized the PID control strategy to compensate for the external forces exerted by the patient on the robot. Huang et al. [32] proposed a variable integral PID (VIPID) controller to track the patients’ finger trajectory which has better performance than the conventional ones. Jones et al. [33] used a PI controller to compensate the auxiliary torque for fingers, and the control of either position or torque can be implemented in this device. Polygerinos et al. [34] presented a sliding-mode controller (SMC) for their finger rehabilitation robot with the obvious advantage of not requiring an explicit model of the system for the synthesis of the controller.The large number of degrees of freedom (DoF) and strong interjoint coupling in human fingers make the development of finger rehabilitation robots difficult, leading to the complex structure and difficulty in wearing most of the existing devices. The inability of the fingers to perform A/A motion is one of the signs of nerve damage [35], which affects the patient’s ability to ADL. The active A/A exercise can carry out targeted muscle strength training on the palmar interossei and the dorsal interossei, and fully open the range of motion of the MCP joint [36]. However, few existing robots can achieve active A/A training and cannot fully open the joint mobility of the fingers, which affects the rehabilitation outcome and patient experience. As for the control strategy, it is mainly based on the PID, and the corresponding strategy is developed for the characteristics of the developed equipment.This paper presents the design and development of an end-effector finger rehabilitation robot (EFRR) (see Figure 1). EFRR utilizes a fixed pulley-track module for finger F/E motion, and a novel synchronous pulley set has been proposed for active A/A motion driven by a single motor. This allows patients to open up their joint mobility fully. EFRR has two thumb rehabilitation structures with left/right symmetry, which makes it possible for functional impairment of the left/right hand to train on the device and can reduce the cost greatly. The design above is also the result of a comprehensive consideration of wearing convenience, hand weight bearing, and manufacturing cost. In terms of control strategy, an adaptive control strategy based on fuzzy PD is designed according to the characteristics of the EFRR, which makes it compliant during the training process and ensures the safety of patients.
The rest of this paper is organized as follows. Section 2 presents the innovative structural design of the EFRR, including the design principles and rationale; Section 3 introduces the adaptive control strategy based on fuzzy PD; Section 4 shows the preliminary experiments conducted at the EFRR and the related analysis; finally, Section 5 concludes this study and provides suggestions for future work.[…]
[WEB] Noted Ability of Mozart’s Music to Reduce Seizures Explained?
Posted by Kostas Pantremenos in Epilepsy, Music/Music therapy on June 29, 2021

Listening to Mozart has a notable impact on seizure reduction in patients with epilepsy — and now researchers believe they know why, new research suggests.
Investigators found that the acoustic characteristics of Mozart’s Sonata for Two Pianos in D Major (K448) suppresses brain activity in patients with epilepsy while a piece by the 18th century classical composer Franz Joseph Haydn did not have this effect.
Listening to this Mozart sonata and perhaps other musical pieces may eventually become a treatment for preventing epileptic seizures, said study investigator Ivan Rektor, MD, CSc, Epilepsy Centre at the Hospital St Anne and professor at the Central European Institute of Technology, Masaryk University, Brno, Czech Republic.
“This research into the impact of listening to music could lead to the development of a music-related type of palliative neurostimulation therapy,” Rektor told Medscape Medical News.
The findings were presented at the virtual Congress of the European Academy of Neurology (EAN) 2021 and published online in the European Journal of Neurology.
Clinically Controversial?
Epilepsy affects 6 million people in Europe. Furthermore, estimates show that about 15 million Europeans have had at least one seizure at some time in their lives. In addition, about 30% of patients with epilepsy are not adequately treated with antiseizure medications.
Researchers have been studying the impact of Mozart’s music on brain-wave activity since the 1990s. Various studies report a reduction in epileptiform discharges in patients with epileptic seizures, coma, and refractory nonconvulsive status.
[WEB] Analysis Highlights Potential Treatment Gap in Adults Living with Spasticity
Posted by Kostas Pantremenos in Spasticity on June 29, 2021
Posted by Debbie Overman

Ipsen announces findings from a new US healthcare database analysis to assess the current treatment patterns of adults living with spasticity in a real-life setting.
The analysis focused on the proportion of people living with active spasticity who received botulinum neurotoxin type A (BoNT-A) treatment. The abstract, Analysis of US Commercial Claims to Understand Patient Treatment Pathways in Spasticity, was presented recently during the International Society of Physical and Rehabilitation Medicine (ISPRM) 2021 Congress.
Spasticity is usually caused by damage to the parts of the brain or spinal cord that control voluntary movement, leading to a change in the balance of signals between the nervous system and the muscles, which results in increased activity in the muscles. When injected into specific muscles of people living with movement disorders, BoNT injections cause temporary muscle relaxation, which can ease symptoms and aid rehabilitation. BoNT-A injections are considered as a recommended first-line treatment for adults living with spasticity in several countries, including the US, a media release from Ipsen explains.
Claims Analysis
Ipsen analyzed data from two large US commercial claims databases: IBM Watson’s MarketScan and the IQVIA Anonymous Longitudinal Patient Data (APLD) database:
- A total of 4,974,859 records were accessed in the MarketScan database, and 10,685,964 records in the IQVIA database.
- Spasticity was identified from the two sources using International Classification of Disease (ICD) codes for spastic conditions (eg, monoplegia, diplegia, hemiplegia and contracture).
- This revealed 126,465 and 1,151,127 people living with spasticity in the MarketScan and IQVIA databases, respectively.
- In the MarketScan database, only 5,111 people living with spasticity (4%) were treated with BoNT-A. In the IQVIA database, an even smaller percentage were treated with BoNT-A (31,176 patients, 3%).
“While effective treatment of spasticity requires a multidisciplinary approach, which may involve a combination of exercise, physical therapy, medication, or surgery, it is concerning to see that many people living with spasticity in the US are not receiving a recommended first-line treatment. The pandemic has been disruptive to the management of spasticity; these new data have, however, put a spotlight on the broader issues in the treatment of this condition that pre-date the pandemic.”
— Isabelle Bocher-Pianka, Chief Patient Affairs Officer at Ipsen
“We need to address barriers to treatment and find innovative ways to address the access issues in the treatment of this debilitating condition. Despite being a recommended first-line treatment, these data highlight a significant disconnect between the patient journey and the guidelines, since BoNT-A is only used for a small proportion of people living with spasticity in the US and this is likely to be true in other parts of the world.”
— Dr Alberto Esquenazi, Sheerr Gait and Motion Analysis Laboratory, MossRehab
“Poor control of spasticity can result in the breakthrough of painful symptoms such as muscle stiffness, spasms and involuntary contractions, which means the person living with spasticity may find it difficult to walk or perform certain tasks. These data show there is an urgent need to build on these findings and gather further insights into the underlying reasons for this disconnect.”
— Dr. Andreas Lysandropoulos, Vice President, Head of Global Medical Affairs Neuroscience at Ipsen
[Source(s): Ipsen, Business Wire]
[Abstract] The effect of listening to SMT music made using musical expectancy violations on brain concentration and activation – Full Text PDF
Posted by Kostas Pantremenos in Music/Music therapy, REHABILITATION on June 29, 2021
Abstract
This study investigated the effect of listening to self-music therapy training (SMT) music, which was specially developed using musical expectancy violations, on improving brain concentration and activation. It was performed with a sample of 12 adults. Electroencephalograms (EEG) were obtained and analyzed after allowing the participants to listen to SMT music. An EEG device with eight channels was used to measure the brain waves. The changes in the EEGs were recorded when listening to SMT music in three states (stable, basic, and stimulated) after attaching the electrodes to the prefrontal cortex (Fp1 and Fp2), and the frontal (F3 and F4), temporal (T3 and T4), and parietal lobes (P3 and P4) according to the International 10/20 system. The EEG data were analyzed to determine the m-β wave appearance rate and absolute total power (ATP) for the three conditions, and a t-test was performed. The results showed that the rate of m-β wave appearance was higher in the stimulated and basic states than in the stable state (Fp1, Fp2, F4, T3, T4, P3, and P4) and higher in the stimulated state than in the basic state (Fp1, Fp2, T3, T4, and P4). The ATP was lower in the basic state than in the stable state (Fp2, F3, F4, and T3), but the ATP in the stimulated state was higher than in the basic or stable state in all areas excluding the left and right parietal lobes (Fp1, Fp2, F3, F4, T3, and T4). These results demonstrated that listening to SMT music by normal adults could increase brain concentration and activation.
[ARTICLE] The State of Music Therapy Studies in the Past 20 Years: A Bibliometric Analysis – Full Text
Posted by Kostas Pantremenos in Music/Music therapy, REHABILITATION on June 29, 2021
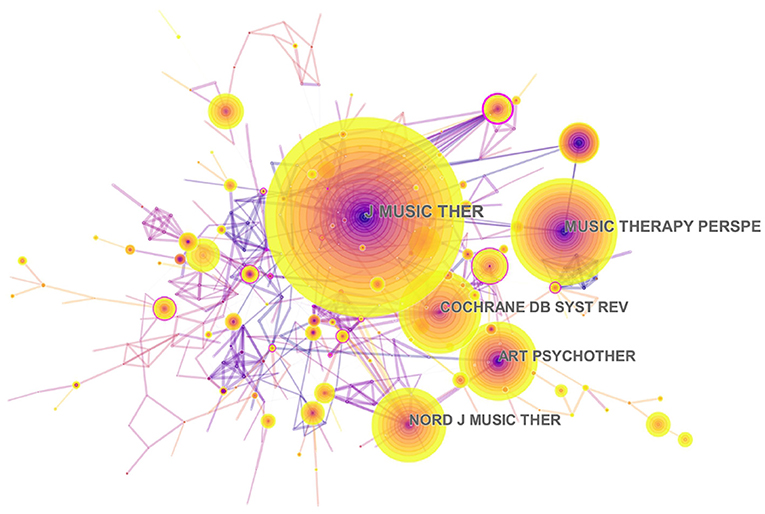
Purpose: Music therapy is increasingly being used to address physical, emotional, cognitive, and social needs of individuals. However, publications on the global trends of music therapy using bibliometric analysis are rare. The study aimed to use the CiteSpace software to provide global scientific research about music therapy from 2000 to 2019.
Methods: Publications between 2000 and 2019 related to music therapy were searched from the Web of Science (WoS) database. The CiteSpace V software was used to perform co-citation analysis about authors, and visualize the collaborations between countries or regions into a network map. Linear regression was applied to analyze the overall publication trend.
Results: In this study, a total of 1,004 studies met the inclusion criteria. These works were written by 2,531 authors from 1,219 institutions. The results revealed that music therapy publications had significant growth over time because the linear regression results revealed that the percentages had a notable increase from 2000 to 2019 (t = 14.621, P < 0.001). The United States had the largest number of published studies (362 publications), along with the following outputs: citations on WoS (5,752), citations per study (15.89), and a high H-index value (37). The three keywords “efficacy,” “health,” and “older adults,” emphasized the research trends in terms of the strongest citation bursts.
Conclusions: The overall trend in music therapy is positive. The findings provide useful information for music therapy researchers to identify new directions related to collaborators, popular issues, and research frontiers. The development prospects of music therapy could be expected, and future scholars could pay attention to the clinical significance of music therapy to improve the quality of life of people.
Introduction
Music therapy is defined as the evidence-based use of music interventions to achieve the goals of clients with the help of music therapists who have completed a music therapy program (Association, 2018). In the United States, music therapists must complete 1,200 h of clinical training and pass the certification exam by the Certification Board for Music Therapists (Devlin et al., 2019). Music therapists use evidence-based music interventions to address the mental, physical, or emotional needs of an individual (Gooding and Langston, 2019). Also, music therapy is used as a solo standard treatment, as well as co-treatment with other disciplines, to address the needs in cognition, language, social integration, and psychological health and family support of an individual (Bronson et al., 2018). Additionally, music therapy has been used to improve various diseases in different research areas, such as rehabilitation, public health, clinical care, and psychology (Devlin et al., 2019). With neurorehabilitation, music therapy has been applied to increase motor activities in people with Parkinson’s disease and other movement disorders (Bernatzky et al., 2004; Devlin et al., 2019). However, limited reviews about music therapy have utilized universal data and conducted massive retrospective studies using bibliometric techniques. Thus, this study demonstrates music therapy with a broad view and an in-depth analysis of the knowledge structure using bibliometric analysis of articles and publications.
Bibliometrics turns the major quantitative analytical tool that is used in conducting in-depth analyses of publications (Durieux and Gevenois, 2010; Gonzalez-Serrano et al., 2020). There are three types of bibliometric indices: (a) the quantity index is used to determine the number of relevant publications, (b) the quality index is employed to explore the characteristics of a scientific topic in terms of citations, and (c) the structural index is used to show the relationships among publications (Durieux and Gevenois, 2010; Gonzalez-Serrano et al., 2020). In this study, the three types of bibliometric indices will be applied to conduct an in-depth analysis of publications in this frontier.
While research about music therapy is extensively available worldwide, relatively limited studies use bibliometric methods to analyze the global research about this topic. The aim of this study is to use the CiteSpace software to perform a bibliometric analysis of music therapy research from 2000 to 2019. CiteSpace V is visual analytic software, which is often utilized to perform bibliometric analyses (Falagas et al., 2008; Ellegaard and Wallin, 2015). It is also a tool applied to detect trends in global scientific research. In this study, the global music therapy research includes publication outputs, distribution and collaborations between authors/countries or regions/institutions, intense issues, hot articles, common keywords, productive authors, and connections among such authors in the field. This study also provides helpful information for researchers in their endeavor to identify gaps in the existing literature.[…]
[BLOG] Self-Directed Neuroplasticity
Posted by Kostas Pantremenos in Neuroplasticity on June 28, 2021
“What flows through your mind sculpts your brain. Thus, you can use your mind to change your brain for the better.” – Rick Hanson, PhD
As a human, you’re uniquely capable of deliberate mind training.
No other animal has this ability.
Of course, other animals learn, and their brains undergo neuroplastic changes (forming new neural circuits). But none can do so consciously.
This process is called self-directed neuroplasticity, and it’s your ticket to a fit mind.
What is Self-Directed Neuroplasticity?
First, let’s briefly look at regular old neuroplasticity.
Until a couple of decades ago, neuroscience was unaware that the adult brain could change. The consensus at the time was that your brain steadily declines once it reaches maturity.
More recently, it’s become clear that your brain continues to wire itself up until your last breath. It’s always adapting.
According to Hebb’s Law, “neurons that fire together, wire together,” meaning that your brain forms new neural connections depending on how you use it.
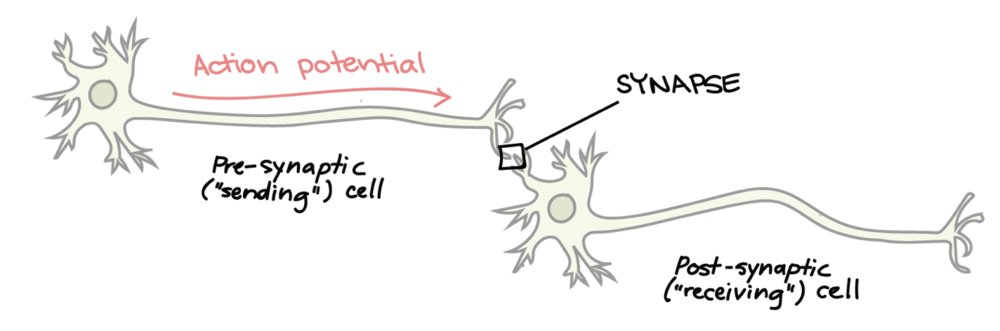
The human brain contains 85-100 billion neurons, which are constantly receiving chemical messages from other neurons and passing them on.
When you repeat an action, like swinging a tennis racket, the related neural synapses form stronger connections. So next time you swing a racket, that movement requires less energy. Neuroplasticity is science’s term for this structural and functional change in the brain as it adapts.
Self-directed neuroplasticity, then, is your ability to change your own brain by applying it in a particular way. The “self-directed” piece refers to your ability to intentionally choose how your brain models itself.
For example, thinking positive thoughts has been shown to produce epigenetic changes in the brain.[1] Whatever is on your mind today is building your brain of tomorrow. That can be good or bad depending on the mindset that you’re engraving into your brain.
Since the brain creates thousands of new neurons every day, constantly rearranging its neural connections, it becomes critical to shape it in helpful ways.
So how do you take full advantage of self-directed neuroplasticity?
How Meditation Trains the Brain
Meditation is a system of mental training. You can build positive qualities of mind like focus, vitality, and joy.
The main mechanism behind meditation’s transformative potential is self-directed neuroplasticity.
You’re using your mind to change the brain, like a child crafting Playdough. It’s empowering to know that you’re in control of your own mental fitness.
Let’s say you want to improve your attention muscles. If you practice a concentration meditation technique, repeatedly bringing your wandering mind back to your breath, for example, you’ll begin to sculpt a strong attention.
[Note: For guided self-directed neuroplasticity exercises, check out the FitMind meditation app.]
You know those people who seem so naturally attentive, happy, and full of energy? We all have access to this way of being. Your mind is not a fixed entity.
That’s the most inspiring part about self-directed neuroplasticity: it means you can shape your mind any way you’d like. Each of us has the power (and even responsibility) to create the mind we want.
The Brain of an Olympic Meditator
Indeed scientists have found that experienced meditators’ brains look different.
They exhibit an enlarged prefrontal cortex (responsible for rational decision-making),[2] smaller amygdala (the fear center of the brain),[3] thicker hippocampus (key for learning and memory),[4] and overall increased grey matter (brain cell bodies important for processing power and linked to intelligence).[5]

This rewiring doesn’t happen overnight, of course, but you can start the process with as little as five minutes per day, which has been shown to create neuroplastic changes.
What few people realize is that anyone can sculpt their mind, improving their perception of the world in each moment.
P.S. — If you’re serious about learning methods of self-directed neuroplasticity, check out the FitMind meditation app.
Sources:
[1] See: Blackburn, E., & Epel, E. (2017). The telomere effect: a revolutionary approach to living younger, healthier, longer. Hachette UK.
[2] Lazar, S. W., Kerr, C. E., Wasserman, R. H., Gray, J. R., Greve, D. N., Treadway, M. T., … & Fischl, B. (2005). Meditation experience is associated with increased cortical thickness. Neuroreport, 16(17), 1893.
[3] Taren, A. A., Creswell, J. D., & Gianaros, P. J. (2013). Dispositional mindfulness co-varies with smaller amygdala and caudate volumes in community adults. PloS one, 8(5), e64574.
[4] Hölzel, B. K., Carmody, J., Vangel, M., Congleton, C., Yerramsetti, S. M., Gard, T., & Lazar, S. W. (2011). Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry research: neuroimaging, 191(1), 36-43.
[5] Luders, E., Cherbuin, N., & Kurth, F. (2015). Forever Young (er): potential age-defying effects of long-term meditation on gray matter atrophy. Frontiers in Psychology, 5, 1551.
Image Credits:
pre-post synaptic connected by khanacademy
synapse and neuron cells by Andrii Vodolazhskyi
meditation and the brain by UA Magazine
[Abstract] A personalized home-based rehabilitation program using exergames combined with a telerehabilitation application in a chronic stroke survivor: a mixed-methods case study.
Posted by Kostas Pantremenos in REHABILITATION, Tele/Home Rehabilitation, Video Games/Exergames on June 25, 2021
Abstract
Background
In Canada, only 11% of stroke survivors have access to outpatient and community-based rehabilitation after discharge from inpatient rehabilitation. Hence, innovative community-based strategies are needed to provide adequate post-rehabilitation services. The VirTele program, which combines VIRtual-reality exergames and TELErehabilitation application, was developed to give stroke survivors with residual upper extremity (UE) deficits the opportunity to participate in a personalized home rehabilitation program.
Objective
1) To determine the feasibility of VirTele for remote UE rehabilitation in a chronic stroke survivor; 2) To explore the preliminary efficacy of VirTele on UE motor function, the amount and quality of UE use, impact on quality of life and motivation; 3) To explore the determinants of behavioral intention and use behavior of VirTele and indicators of empowerment.
Methods
A 63-year-old male stroke survivor (3 years) with moderate UE impairment participated in a two-month VirTele intervention. He was instructed to use Jintronix-exergames (5 games for UE) for 30 minutes, five-times per week, and the Reacts application to conduct videoconference sessions with a clinician at least once per week. Motivational interviewing was incorporated into video conference sessions to empower the participant to continue exercising and using his UEs in everyday activities. UE motor function (Fugl-Meyer Assessment-UE), amount and quality of UE use (Motor-Activity-Log-30), impact on quality of life (Stroke-Impact-Scale-16) and motivation (Treatment-Self-regulation-Questionnaire) were measured before (T1), after (T2) VirTele intervention and during a one (T3) and two-month (T4) follow-up period. Qualitative data were collected through logs and a semi-directed interview. Feasibility data (eg, number and duration of video-conference sessions, adherence) were documented at the end of each week.
Results
The participant completed 48 exergame sessions (33 hours) and 8 videoconference sessions. The results suggest that the VirTele intervention (combining Reacts audio-video platform with Jintronix-exergames) and the study protocol could be feasible to use with stroke survivors. The participant exhibited clinically meaningful improvements at T2 on the Fugl-Meyer-UE and Stroke-Impact-Scale-16 and maintained these gains at T3 and T4. During the follow-up periods, the amount and quality of UE use (Motor-Activity-Log-30) showed meaningful change, suggesting more involvement of the affected UE in daily-activities. The participant demonstrated a high level of autonomous motivation (Treatment-Self-regulation-Questionnaire), which may explain his adherence. Performance, effort and social influence have meaningful weight in the behavioral intention of VirTele-use. However, the lack of control over technical and organizational infrastructures may influence the long-term use of the technology. At the end of VirTele, the participant demonstrated considerable empowerment on both behavioral and capacity level.
Conclusions
VirTele was shown to be feasible to use with a chronic stroke survivor for remote UE rehabilitation. Meaningful determinants of behavioral intention and use behavior of VirTele were identified. Preliminary efficacy results are promising but further research is needed to investigate the VirTele-use among varied population.
[WEB] DaxibotulinumtoxinA Injection for Upper-Limb Spasticity Study Receives Positive Results
Posted by Kostas Pantremenos in Paretic Hand, Spasticity on June 25, 2021
Posted by Debbie Overman

Revance Therapeutics Inc announces positive topline data from its JUNIPER Phase 2, randomized, double-blind, placebo-controlled, multi-center clinical trial of its investigational drug candidate DaxibotulinumtoxinA for Injection for the treatment of adults with moderate to severe upper limb spasticity.
The JUNIPER study was designed to evaluate the efficacy and safety of DaxibotulinumtoxinA for Injection for adults with upper limb spasticity after stroke or traumatic brain injury and to identify a dose to advance into a Phase 3 program. Three doses (250 units, 375 units, 500 units) were studied, and subjects were randomized in a 1:1:1:1 ratio across the active doses or placebo.
The trial was originally designed to include 128 subjects. Due to the ongoing COVID-19 challenges related to continued subject enrollment and the scheduling of in-person study visits, Revance made the decision in June 2020 to curtail enrollment at 83 subjects, according to a media release from Revance Therapeutics Inc.
“As an investigator in the JUNIPER trial, I am delighted to see the efficacy and safety data that will support the advancement of DaxibotulinumtoxinA for Injection in adult upper limb spasticity. What impresses me most is the duration of effect covering at least 24-weeks across all dose groups studied, while also being well tolerated.
“The need for longer duration botulinum toxin treatments for upper limb spasticity is considerable, as the frequent re-emergence of symptoms around 12 weeks continues to be a painful, costly and a time-consuming burden for patients. The data indicates that DaxibotulinumtoxinA for Injection has the potential to reduce the frequency of adult upper limb spasticity treatments by up to 50% annually, delivering meaningful pharmacoeconomic benefits, improvement in patients’ quality of life, and the opportunity to expand treatment care.”
— Atul Patel, MD, MHSA, Medical Director, Kansas Institute of Research
About the JUNIPER Study
The company’s JUNIPER study was a Phase 2, randomized, double-blind, placebo-controlled, parallel group, dose-ranging, multi-center trial to evaluate the efficacy and safety of DaxibotulinumtoxinA for Injection for the treatment of adult upper limb spasticity in adults following stroke or traumatic brain injury. The study was conducted at 30 sites in the United States and has enrolled 83 male and female patients between the age of 18 to 75 years old.
Patients were randomized into one of four treatment groups: 275 units, 350 units, 500 units and placebo. The study was designed to run up to 36 weeks, with two co-primary outcome measures: mean change from baseline in muscle tone measured with the MAS in SMG of the elbow, wrist, or finger flexors at Week 6; and mean score of the PGIC at Week 6. The first 73 subjects, who were dosed before enrollment was paused in March due to the COVID-19 pandemic, were followed up for 36 weeks, and the succeeding 10 subjects were followed up to Week 12.
Study Endpoints
The study’s co-primary endpoints were improvement from baseline in the Modified Ashworth Score (MAS) and the Physician Global Impression of Change (PGIC) score at Week 6. In the JUNIPER study, proof of concept was demonstrated with all three doses being numerically higher than placebo for the improvement in the MAS score, with the 500-unit dose demonstrating a clinically meaningful and statistically significant reduction from baseline in muscle tone versus placebo (p=0.0488). Additionally, each of the three doses demonstrated a numerical improvement compared with placebo on the PGIC assessment but did not reach statistical significance with the reduced enrollment.
On a key secondary endpoint, DaxibotulinumtoxinA for Injection delivered a median duration of at least 24 weeks across all three doses. Duration of effect was defined as the time from injection (in weeks) until the loss of improvement as measured by the MAS (for the suprahypertonic muscle group or SMG) and the PGIC, or a request for retreatment by the subject.
All three doses of DaxibotulinumtoxinA for Injection were generally safe and well tolerated with no increase in the incidence of adverse events observed in the higher dose treatment groups. The majority of treatment-related adverse events were mild or moderate in severity and were similar to or lower than those reported in prior botulinum toxin studies in adult upper limb spasticity, the release continues.
“I am very proud of our team and their efforts to successfully complete our Phase 2 trial during what has proven to be a very challenging time for trial enrollment and follow up. Although we reduced the subject enrollment size in response to COVID-19 concerns, we were able to generate sufficient data to inform our dosing strategy for our Phase 3 program, while also demonstrating a long duration profile that is consistent across our therapeutic and aesthetic clinical programs.
“Our next step is to schedule an end-of-Phase 2 meeting with the FDA prior to finalizing a Phase 3 program. I want to thank the patients, investigators, CROs and the Revance team for their time and commitment in making this trial possible.”
— Mark J. Foley, President and Chief Executive Officer at Revance
[Source(s): Revance Therapeutics Inc, Business Wire]
[Abstract] Combined action observation- and motor imagery-based brain computer interface (BCI) for stroke rehabilitation: a case report – Full text PDF
Posted by Kostas Pantremenos in Paretic Hand on June 22, 2021
Abstract
Introduction:
Upper extremity impairment is a problem usually found in poststroke patients, and it is seldom completely improved even following conventional physical therapy. Motor imagery (MI) and action observation (AO) therapy are mental practices that may regain motor function in poststroke patients, especially when integrating them with brain-computer interface (BCI) technology. However, previous studies have always investigated the effects of an MI- or AO-based BCI for stroke rehabilitation separately. Therefore, in this study, we aimed to propose the effectiveness of a combined AO and MI (AOMI)-based BCI with functional electrical stimulation (FES) feedback to improve upper limb functions and alter brain activity patterns in chronic stroke patients. Case presentation: A 53-year-old male who was 12 years post stroke was left hemiparesis and unable to produce any wrist and finger extension. Intervention: The participant was given an AOMI-based BCI with FES feedback 3 sessions per week for 4 consecutive weeks, and he did not receive any conventional physical therapy during the intervention. The Fugl-Meyer Assessment of Upper Extremity (FMA-UE) and active range of motion (AROM) of wrist extension were used as clinical assessments, and the laterality coefficient (LC) value was applied to explore the altered brain activity patterns affected by the intervention. Outcomes: The FMA-UE score improved from 34 to 46 points, and the AROM of wrist extension was increased from 0 degrees to 20 degrees. LC values in the alpha band tended to be positive whereas LC values in the beta band seemed to be slightly negative after the intervention.
Conclusion:
An AOMI-based BCI with FES feedback training may be a promising strategy that could improve motor function in poststroke patients; however, its efficacy should be studied in a larger population and compared to that of other therapeutic methods.
