Archive for March, 2021
[Proceedings] Robotic Orthosis for Upper Limb Rehabilitation – Full Text PDF file.
Posted by Kostas Pantremenos in Paretic Hand, REHABILITATION, Rehabilitation robotics on March 31, 2021
Abstract
Individuals with impaired upper limb have motor limitations that interfere with functionality. An alternative to rehabilitation consists of Robot Assisted Therapy, a method that increases the effectiveness of treatment. New robotic actuators have been developed to assist in the rehabilitation of the upper limb. One of them aims to actively perform finger extension and flexion passively, using a servo motor coupled to a rope system. At the elbow, a DC motor combined with a gearbox was coupled to a system of pulleys and ropes designed to actively perform flexion and extension movements. To activate the system, an Arduino-NANO® and a mobile application for Android were used. The performance of the prototype was evaluated in four post-stroke volunteers.
The ability to perform the proposed movements with the device was observed. Structural reinforcement was necessary, after twisting the elbow support structure, with pronation of the forearm, resulting in increased component weight. This work presented new robotic devices that can assist in the rehabilitation of post-stroke individuals.
[Abstract] Home‐based Virtual Reality Therapy for Hand Recovery After Stroke
Posted by Kostas Pantremenos in Paretic Hand, Tele/Home Rehabilitation, Virtual reality rehabilitation on March 31, 2021
ABSTRACT
Introduction
Many stroke survivors suffer from arm and hand weakness, but there are only limited efficacious options for arm therapy available.
Objective
To assess the feasibility of unsupervised home‐based use of a virtual reality device (Smart Glove) for hand rehabilitation post stroke.
Design
Prospective single‐arm study consisting of a 2‐week run‐in phase with no device use followed by an 8‐week intervention period.
Setting
Participants were recruited at the Stanford Neuroscience Outpatient Clinic.
Participants
Twenty chronic stroke patients with upper extremity impairment.
Interventions
Participants were instructed to use the Smart Glove 50 minutes per day, 5 days per week for 8 weeks.
Main Outcome Measures
We measured (1) compliance, (2) patients’ impression of the intervention, and (3) efficacy measures including the upper extremity Fugl‐Meyer (UE‐FM), the Jebsen‐Taylor hand function test (JTHFT) and the Stroke Impact Scale (SIS).
Results
Of 20 subjects, 7 (35%) met target compliance of 40 days use, and 6 (30%) used the device for 20‐39 days. Eighty‐five percent of subjects were satisfied with the therapy, with 80% reporting improvement in hand function. During the run‐in phase there were no improvements in hand function. During the intervention, patients improved by a mean of 26.6 ± 48.8 seconds on the JTHFT (P = 0.03), by 16.1 ± 15.3 points on the hand‐domain of the SIS (P < 0.01) and there was a trend towards improvement on the UE‐FM (2.2 ± 5.5 points, P = 0.10).
Conclusions
Unsupervised use of the Smart Glove in the home environment may improve hand/arm function in subacute/chronic stroke patients. A randomized controlled trial is needed to confirm these results.
[WEB PAGE] Can Anxiety Cause Seizures?
Posted by Kostas Pantremenos in Epilepsy on March 31, 2021
- Anxiety and seizures
- PNES (pseudoseizures)
- Panic attacks and seizures
- Panic attack vs. PNES
- PNES symptoms
- PNES diagnosis
- PNES treatment
- Bottom line
Anxiety is a necessary human emotion designed to alert us to potential dangers and protect us from potential threats. For most people, feelings of anxiety are short-lived, but in some people, anxiety can become a chronic condition that greatly impacts quality of life.
Anxiety can cause a wide range of physical and mental symptoms, one of which may include psychogenic nonepileptic seizures (PNES), also called pseudoseizures.
In this article, we’ll explain what PNES are, how they differ from neurological seizures, and everything you need to know about anxiety and PNES.
Can anxiety cause seizures?
A seizure is a brief period of uncontrolled electrical activity in the brain that can provoke a wide variety of changes in the body. Epilepsy is a chronic condition that causes unpredictable, recurrent seizures.
Seizures can be caused by a variety of triggers, including increased stress and anxiety. In fact, according to the British Epilepsy AssociationTrusted Source, stress is one of the most commonly self-reported seizure triggers in people with epilepsy.
Research has also shown that even in people without epilepsy, stress and anxiety can trigger what’s known as psychogenic nonepileptic seizures (PNES), or pseudoseizures. PNES are physiologically different from the neurological seizures found in epilepsy.
What are a psychogenic nonepileptic seizures (PNES), or pseudoseizures?
Pseudoseizures (PNES) aren’t the same type of neurological seizures that are caused by uncontrolled activity in the brain. Instead, PNES are an extreme response to stress and anxiety and are therefore considered psychiatric in nature.
According to the literatureTrusted Source, PNES are classified as a type of functional neurological disorder (FND), or conversion disorder. Conversion disorders are triggered by emotional stress that causes physical symptoms that can’t be explained by other underlying conditions.
PNES most often occur in people who struggle to manage stress, anxiety, or other traumatic emotions through traditional coping strategies. When these emotions become overwhelming enough, the body may shut down as a defense mechanism. In some people, this can present as a PNES.
Can a panic attack cause a seizure?
Sometimes, anxiety symptoms can manifest as a sudden, intense episode called a panic attack. Panic attack symptoms mimic many of the same symptoms you may feel when you’re anxious. However, you may also notice other intense symptoms, such as:
- difficulty breathing or swallowing
- sharp chest pains
- chills or hot flashes
- tingling or numbness in the extremities
- feelings of panic or dread
- feelings of disconnection from yourself or reality
Panic attacks aren’t a known cause of neurological seizures in people without epilepsy. However, there may be a correlation between panic attacks and PNES in people who experience them.
In one meta-analysisTrusted Source from 2018, researchers investigated the link between panic and hyperventilation and PNES. Eighteen studies were analyzed for a potential relationship between panic attacks, hyperventilation episodes, and PNES.
According to the results, up to 83 percent of individuals who had PNES also reported having accompanying panic attacks. In addition, the researchers found that up to 30 percent of individuals with voluntarily induced hyperventilation also experienced PNES.
While these results seem to suggest that panic attacks and panic attack symptoms may be a trigger for PNES, more research is still needed.ADVERTISEMENTExplore new calming exercises with Calm
Manage your anxiety with the award-winning Calm app. Try a guided meditation, a sleep story, or stretches designed by experts to help you focus and relax. Start your free trial today.START FREE TRIAL
What’s the difference between a panic attack and a PNES?
Panic attacks and PNES can both happen as a result of stress and anxiety. However, there are differences between the two experiences that distinguish them from each other.
Panic attacks
These episodes feature many, if not all, of the classic symptoms of anxiety. Panic attacks come on suddenly and pass within about 10 minutes. Many people who have panic attacks are still able to retain some level of function during the attack. However, symptoms vary from person to person.
PNES (pseudoseizures)
These episodes may not feature any symptoms of panic or anxiety at all. PNES tend to come on gradually and last longer than panic attacks. Many people who have PNES also experience panic symptoms, but some don’t.
In some cases, panic attacks can even be used as a diagnostic tool to help differentiate PNES from neurological seizures. In one studyTrusted Source from 2014, researchers found that panic attack symptoms were more likely to appear in a PNES than in an epileptic seizure.
What are the symptoms of PNES?
Although PNES and neurological seizures may appear similar, there are some differences in symptoms between the two conditions. For example, PNES may feature some of the symptoms found in neurological seizures, such as:
- lowered awareness
- loss of body control
- flailing or thrashing
- head arching
- tongue biting
In addition to the symptoms above, PNES may also present with symptoms not traditionally found in neurological seizures, such as:
- side to side head movements
- nonsynchronized body movements
- muscle contractions
- closed or fluttering eyes
- crying during the episode
- avoidance behaviors
- memory recall or avoidance
Another distinguishing factor of PNES is that these symptoms tend to appear more gradually and last longer than in neurological seizures.
How are PNES diagnosed?
If you have been experiencing PNES, your doctor will most likely refer you to an inpatient setting for testing. Video-electroencephalography (vEEG) is the most common diagnostic test for pseudoseizures.
During your inpatient stay, you will be connected to an electroencephalography (EEG) machine and a video monitoring system. The EEG machine tracks electrical activity in the brain, while the video monitoring system records any physical symptoms.
Any seizures or PNES that happen during your stay will be analyzed to determine the correct diagnosis. If you appear to have a seizure, but there’s no unusual brain activity, the most likely diagnosis is PNES.
In some cases, further imaging of the brain with a CT scan or MRI scan may be warranted. Your doctor may also want to perform further testing to eliminate any other underlying conditions, such as deficiency or infection.
They may also order additional psychological testing to narrow down any potential causes or triggers for your PNES.
How are PNES treated?
Since PNES are psychological in nature, treatmentTrusted Source of the underlying anxiety is important. Treatment options for anxiety-induced PNES may include:
- Psychotherapy. Cognitive-behavioral therapy (CBT) is the first line of treatment for anxiety disorders. With CBT, an individual can learn how to better cope with stressful or anxious thoughts, feelings, and behaviors. This may help reduce the frequency of pseudoseizures. In addition, trauma-focused therapy may be helpful for individuals with trauma-based disorders who experience pseudoseizures.
- Medications. Anti-epileptic drugs aren’t useful for pseudoseizures because these seizures aren’t neurological. Instead, selective serotonin reuptake inhibitors (SSRIs) may be prescribed to help reduce the symptoms of anxiety that can cause pseudoseizures. SSRIs have been found to be most effectiveTrusted Source when used in conjunction with psychotherapy.
- Lifestyle. Both psychotherapy and medications can help an individual more easily cope with stress and anxiety. In turn, this can reduce the potential for emotionally triggered pseudoseizures. However, lifestyle changes can also help to reduce the symptoms of anxiety. Focusing on good sleep, a balanced diet, daily exercise, and mindfulness practices can further reduce anxiety and greatly improve quality of life.
Ultimately, you and your doctor will work together to come up with the best treatment approach for your personal situation.
The bottom line
While anxiety is unlikely to trigger neurological seizures in people without epilepsy, it can trigger PNES in individuals with underlying mental health conditions. Since these episodes have a psychiatric origin, treatment of the underlying anxiety can help reduce or eliminate these episodes.
If you’re concerned that you have been having PNES, reach out to your doctor for an appropriate diagnosis and treatment.
Last medically reviewed on March 29, 2021
[WEB PAGE] Wireless neuromodulation technology could improve the lives of patients with brain disorders
Posted by Kostas Pantremenos in Depression, Epilepsy on March 31, 2021
Reviewed by Emily Henderson, B.Sc.
Scientists make pivotal discovery of method for wireless modulation of neurons with X-rays that could improve the lives of patients with brain disorders. The X-ray source only requires a machine like that found in a dentist’s office.
Many people worldwide suffer from movement-related brain disorders. Epilepsy accounts for more than 50 million; essential tremor, 40 million; and Parkinson’s disease, 10 million.
Relief for some brain disorder sufferers may one day be on the way in the form of a new treatment invented by researchers from the U.S. Department of Energy’s (DOE) Argonne National Laboratory and four universities. The treatment is based on breakthroughs in both optics and genetics. It would be applicable to not only movement-related brain disorders, but also chronic depression and pain.
Our high precision noninvasive approach could become routine with the use of a small X-ray machine, the kind commonly found in every dental office.”
Elena Rozhkova, Nanoscientist, Argonne’s Center for Nanoscale Materials
This new treatment involves stimulation of neurons deep within the brain by means of injected nanoparticles that light up when exposed to X-rays (nanoscintillators) and would eliminate an invasive brain surgery currently in use.
“Our high-precision noninvasive approach could become routine with the use of a small X-ray machine, the kind commonly found in every dental office,” said Elena Rozhkova, a lead author and a nanoscientist in Argonne’s Center for Nanoscale Materials (CNM), a DOE Office of Science User Facility.
Traditional deep brain stimulation requires an invasive neurosurgical procedure for disorders when conventional drug therapy is not an option. In the traditional procedure, approved by the U.S. Food and Drug Administration, surgeons implant a calibrated pulse generator under the skin (similar to a pacemaker).
They then connect it with an insulated extension cord to electrodes inserted into a specific area of the brain to stimulate the surrounding neurons and regulate abnormal impulses.
“The Spanish-American scientist José Manuel Rodríguez Delgado famously demonstrated deep brain stimulation in a bullring in the 1960s,” said Vassiliy Tsytsarev, a neurobiologist from the University of Maryland and a co-author of the study. ”He brought a raging bull charging at him to a standstill by sending a radio signal to an implanted electrode.”
About 15 years ago, scientists introduced a revolutionary neuromodulation technology, ”optogenetics,” which relies on genetic modification of specific neurons in the brain. These neurons create a light-sensitive ion channel in the brain and, thereby, fire in response to external laser light. This approach, however, requires very thin fiberoptic wires implanted in the brain and suffers from the limited penetration depth of the laser light through biological tissues.
The team’s alternative optogenetics approach uses nanoscintillators injected in the brain, bypassing implantable electrodes or fiberoptic wires. Instead of lasers, they substitute X-rays because of their greater ability to pass through biological tissue barriers.
“The injected nanoparticles absorb the X-ray energy and convert it into red light, which has significantly greater penetration depth than blue light,” said Zhaowei Chen, former CNM postdoctoral fellow.
“Thus, the nanoparticles serve as an internal light source that makes our method work without a wire or electrode,” added Rozhkova. Since the team’s approach can both stimulate and quell targeted small areas, Rozhkova noted, it has other applications than brain disorders. For example, it could be applicable to heart problems and other damaged muscles.
One of the team’s keys to success was the collaboration between two of the world-class facilities at Argonne: CNM and Argonne’s Advanced Photon Source (APS), a DOE Office of Science User Facility. The work at these facilities began with the synthesis and multi-tool characterization of the nanoscintillators.
In particular, the X-ray excited optical luminescence of the nanoparticle samples was determined at an APS beamline (20-BM). The results showed that the particles were extremely stable over months and upon repeated exposure to the high-intensity X-rays.
According to Zou Finfrock, a staff scientist at the APS 20-BM beamline and Canadian Light Source, ”They kept glowing a beautiful orange-red light.”
Next, Argonne sent CNM-prepared nanoscintillators to the University of Maryland for tests in mice. The team at University of Maryland performed these tests over two months with a small portable X-ray machine. The results proved that the procedure worked as planned. Mice whose brains had been genetically modified to react to red light responded to the X-ray pulses with brain waves recorded on an electroencephalogram.
Finally, the University of Maryland team sent the animal brains for characterization using X-ray fluorescence microscopy performed by Argonne scientists. This analysis was performed by Olga Antipova on the Microprobe beamline (2-ID-E) at APS and by Zhonghou Cai on the Hard X-ray Nanoprobe (26-ID) jointly operated by CNM and APS.
This multi-instrument arrangement made it possible to see tiny particles residing in the complex environment of the brain tissue with a super-resolution of dozens of nanometers.
It also allowed visualizing neurons near and far from the injection site on a microscale. The results proved that the nanoscintillators are chemically and biologically stable. They do not wander from the injection site or degrade.
“Sample preparation is extremely important in these types of biological analysis,” said Antipova, a physicist in the X-ray Science Division (XSD) at the APS. Antipova was assisted by Qiaoling Jin and Xueli Liu, who prepared brain sections only a few micrometers thick with jeweler-like accuracy.
“There is an intense level of commercial interest in optogenetics for medical applications,” said Rozhkova. ”Although still at the proof-of-concept stage, we predict our patent-pending wireless approach with small X-ray machines should have a bright future.”Source:
(DOE)/Argonne National LaboratoryJournal reference:
Chen, Z., et al. (2021) Wireless Optogenetic Modulation of Cortical Neurons Enabled by Radioluminescent Nanoparticles. ACS Nano. doi.org/10.1021/acsnano.0c10436.
[ARTICLE] A Hand Motor Skills Rehabilitation for the Injured Implemented on a Social Robot – Full Text
Posted by Kostas Pantremenos in Paretic Hand, Rehabilitation robotics on March 31, 2021
Abstract
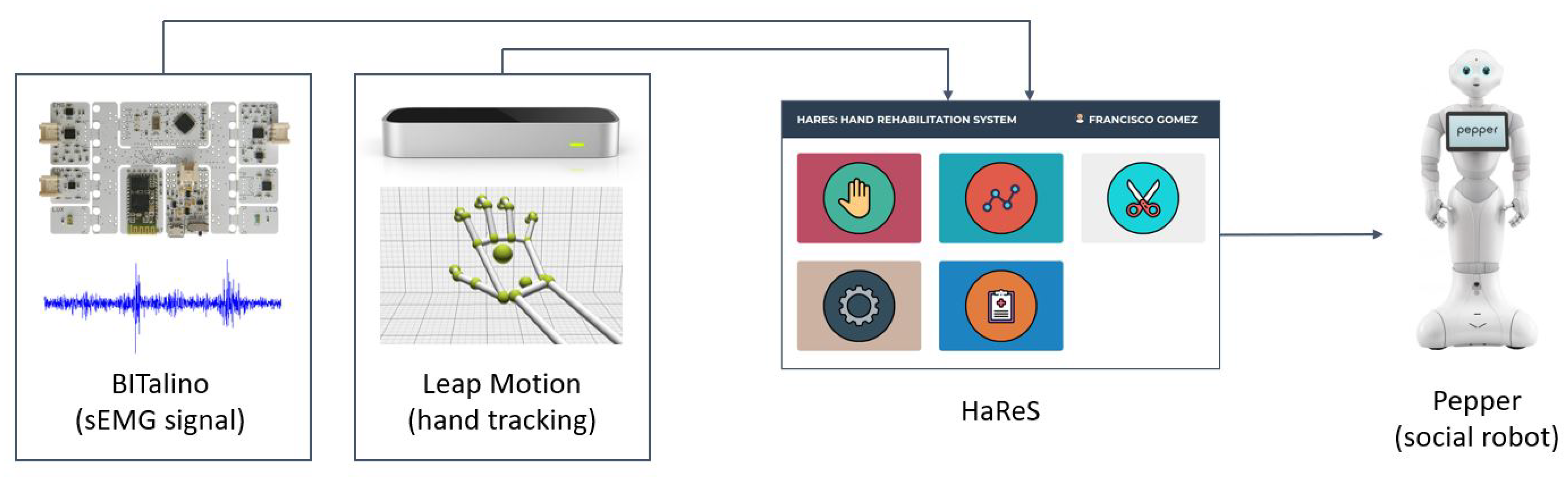
In this work, we introduce HaReS, a hand rehabilitation system. Our proposal integrates a series of exercises, jointly developed with a foundation for those with motor and cognitive injuries, that are aimed at improving the skills of patients and the adherence to the rehabilitation plan. Our system takes advantage of a low-cost hand-tracking device to provide a quantitative analysis of the performance of the patient. It also integrates a low-cost surface electromyography (sEMG) sensor in order to provide insight about which muscles are being activated while completing the exercises. It is also modular and can be deployed on a social robot. We tested our proposal in two different facilities for rehabilitation with high success. The therapists and patients felt more motivation while using HaReS, which improved the adherence to the rehabilitation plan. In addition, the therapists were able to provide services to more patients than when they used their traditional methodology.
1. Introduction
Rehabilitation of the brain- and motor-injured is an important task. These kinds of challenged individuals have reduced motion in their muscles as a result of an accident, acquired diseases, or birth conditions. However, they can improve their motor skills by following a rehabilitation plan. Nonetheless, foundations such as ADACEA, which is a Spanish-based organization for the brain- and motor-injured, are usually under founded and short staffed, and sometimes they cannot provide the required rehabilitation services. In addition, there is a lack of an established protocol to quantitively evaluate a patient’s performance on rehabilitation exercises.So far, the therapists of ADACEA carry out exercises with patients one by one, and do not have any quantitative method to evaluate the patients’ performance. The patients have the rehabilitation sessions scheduled, but since these kinds of foundations are usually short staffed, as mentioned before, the patients do not execute the amount of rehabilitation sessions they should. In addition, the evaluation is purely qualitative. In this sense, the therapists take notes about the performance and significant events such as pain or unusually poor execution of the exercises based on the therapists’ experience. These eventualities negatively impact the way they follow the rehabilitation process and what they take away from it.Having this need in mind, we developed HaReS, a hand rehabilitation system, which is a system for motor rehabilitation. By using HaReS, patients can perform rehabilitation exercises on their own, without requiring the presence of a therapist. Furthermore, HaReS automatically grades the performance of users, so therapists have a quantitative measurement of patients’ performance. This way, the therapists can provide an optimized and enhanced service to more patients.HaReS is composed of a surface electromyography (sEMG) sensor and a hand-tracking device that allows to record and provide quantitative measurements and feedback of the rehabilitation sessions that a patient is performing. The exercises are set up by a therapist for each user. In addition, HaReS can take advantage of a social robot to show the exercises and to interact with patients. Thus, enhancing their adherence and engaging them. The system is modular, so it is able to work without the sensors or the robot. Apart from the robot, the rest of the system is fairly low cost. It is important to note that it is executed on a desktop or laptop computer, so all components are connected to it. The hand-tracking device, the sEMG sensor, and the social robot are all connected to the computer, which is in charge of running HaReS. In this sense, the robot is not executing HaReS, nor are the sensors connected to it. The role of the robot within the HaReS framework is to display the system in its built-in screen and interact with the patient using gestures, lights, and its speech capabilities.The main contributions of this paper are the following:
- A hand rehabilitation system that integrates a series of exercises for the motor- and brain-injured;
- Use of low-cost sensors for hand tracking and muscle signal monitoring;
- An automatic and quantitative evaluation of the exercises to be analyzed by the therapists;
- Optional use of a social robot to improve patient adherence to rehabilitation
The rest of the paper is structured as follows. First, some related work to this matter are presented in Section 2. Then, Section 3 describes the proposal in detail. Next, the evaluation we performed to validate the system is given in Section 4. Finally, Section 5 states the conclusion of this work and future research directions.[…]
[ARTICLE] A Depth Camera–Based, Task-Specific Virtual Reality Rehabilitation Game for Patients With Stroke: Pilot Usability Study – Full Text
Posted by Kostas Pantremenos in REHABILITATION, Video Games/Exergames, Virtual reality rehabilitation on March 31, 2021

Abstract
Background:The use of virtual reality is popular in clinical rehabilitation, but the effects of using commercial virtual reality games in patients with stroke have been mixed.
Objective:We developed a depth camera–based, task-specific virtual reality game, Stomp Joy, for poststroke rehabilitation of the lower extremities. This study aims to assess its feasibility and clinical efficacy.
Methods:We carried out a feasibility test for Stomp Joy within representative user groups. Then, a clinical efficacy experiment was performed with a randomized controlled trial, in which 22 patients with stroke received 10 sessions (2 weeks) of conventional physical therapy only (control group) or conventional physical therapy plus 30 minutes of the Stomp Joy intervention (experimental group) in the clinic. The Fugl-Meyer Assessment for Lower Extremity (FMA-LE), Modified Barthel Index (MBI), Berg Balance Scale (BBS) score, single-leg stance (SLS) time, dropout rate, and adverse effects were recorded.
Results:This feasibility test showed that Stomp Joy improved interest, pressure, perceived competence, value, and effort using the Intrinsic Motivation Inventory. The clinical efficacy trial showed a significant time-group interaction effect for the FMA-LE (P=.006), MBI (P=.001), BBS (P=.004), and SLS time (P=.001). A significant time effect was found for the FMA-LE (P=.001), MBI (P<.001), BBS (P<.001), and SLS time (P=.03). These indicated an improvement in lower extremity motor ability, basic activities of daily living, balance ability, and single-leg stance time in both groups after 2 weeks of the intervention. However, no significant group effects were found for the FMA-LE (P=.06), MBI (P=.76), and BBS (P=.38), while a significant group interaction was detected for SLS time (P<.001). These results indicated that the experimental group significantly improved more in SLS time than did the control group. During the study, 2 dropouts, including 1 participant who fell, were reported.
Conclusions:Stomp Joy is an effective depth camera–based virtual reality game for replacing part of conventional physiotherapy, achieving equally effective improvement in lower extremity function among stroke survivors. High-powered randomized controlled studies are now needed before recommending the routine use of Stomp Joy in order to confirm these findings by recruiting a large sample size.
Introduction
There are 800,000 new or recurring incidences of stroke annually in the United States; the number is rising as the population ages. More than half of stroke survivors live with at least one type of motor impairment [1]. In China, there are approximately 2 million incidences of a stroke every year. Among these stroke survivors, 70% to 80% cannot live independently as a result of multiple impairments, such as motor impairments with loss of strength, stereotypic movements, changes in muscle tone, and limitations in activities [2]. For many patients with stroke, balance and weight shift management constitute a risk for secondary injury. Lower extremity (LE) functional deficits in patients after stroke have aroused a great amount of attention because they play a vital role in stroke survivors’ quality of life [1,2]. Although stroke (new and recurring) remains prevalent, the number of available therapists is far from meeting the need, since the development of physical therapy has still not matured [3,4]. Rehabilitation technologies have the potential to increase the intensity and dose of rehabilitation, improve access to rehabilitation, reduce the workload of therapists, measure and provide feedback about performance and recovery, and engage and motivate patients [5–7]. Evidence-based medicine shows that high-intensity, repetitive, task-specific training tends to benefit patients greatly [8]. However, it is difficult to implement high-intensity, repetitive, task-specific training in a real clinical setting for a variety of reasons, including limited necessary resources and difficulty maintaining patients’ interest. Therefore, virtual reality–based gaming systems have become popular in medical rehabilitation and can be used as a novel alternative therapy method for motor recovery after stroke.
Kinect (Microsoft) is the leader in commercially available low-cost virtual reality (VR) hardware. This is because most of the Kinect’s games are aimed at the average person, and there are many more games designed by research teams for people with stroke, especially for upper limb motor function. However, there are few games focused on lower limb motor function [9]. VR, also known as immersive multimedia or computer-simulated reality, is a computer technology that replicates an environment, real or imagined, and simulates the user’s physical presence and environment to allow for user interaction and immersion. Virtual realities artificially create sensory experience, which can include sight, touch, hearing, and smell [10]. VR systems consist of a development platform, display system, interaction system, and integrated control system [11]. To realize the complete information interaction between computers and humans, normally we need some external device or devices to record the user’s movements. Among the kinds of external devices are force or tactile feedback systems, position trackers, data gloves or 6-degrees-of-freedom space mice, joysticks, and the Kinect sensor [11–13]. Kinect allows users to play without holding a game controller, which means they will not be bothered by wearing sensors that can be intrusive. This also saves time. Zhu et al [14] showed that the Kinect motion capture system was reliable and that the correlation coefficient of the dynamic track was quite good. A large number of clinical studies have shown that the accuracy of the Kinect somatosensory technology sensor for posture control and evaluation can fully meet the needs of body motion evaluation [15–17]. Eltoukhy et al [18] indicated that Kinect-based assessment might provide clinicians a simple tool to simultaneously assess reach distances while developing a clearer understanding of lower extremity movement patterns. Park et al [19] showed that the use of additional VR training with the Xbox Kinect gaming system was an effective therapeutic approach for improving motor function during stroke rehabilitation.
However, these systems were not specifically developed for patients after stroke, and those training sessions might produce multiple effects [20]. Those studies did not assess the flow experience of users, and few of them conducted a clinical randomized controlled trial. To address these issues, we developed a depth camera–based game, Stomp Joy, specifically for the lower limbs of patients with stroke. We also applied two principles of game design that are highly relevant to rehabilitation. The aim of this study was twofold: (1) develop a depth camera–based, task-oriented rehabilitation game for patients with stroke and (2) assess its usability and conduct a pilot study for stroke survivors’ LE rehabilitation.[…]
[ARTICLE] Recovering arm function in chronic stroke patients using combined anodal HD-tDCS and virtual reality therapy (ReArm): a study protocol for a randomised controlled trial – Full Text
Posted by Kostas Pantremenos in Paretic Hand, tDCS/rTMS, Virtual reality rehabilitation on March 30, 2021

Abstract
Background
After a stroke, 80% of the chronic patients have difficulties to use their paretic upper limb (UL) in activities of daily life (ADL) even after rehabilitation. Virtual reality therapy (VRT) and anodal transcranial direct current stimulation (tDCS) are two innovative methods that have shown independently to positively impact functional recovery of the paretic UL when combined with conventional therapy. The objective of the project will be to evaluate the impact of adding anodal high-definition (HD)-tDCS during an intensive 3-weeks UL VRT and conventional therapy program on paretic UL function in chronic stroke.
Methods
The ReArm project is a quadruple-blinded, randomized, sham-controlled, bi-centre, two-arm parallel, and interventional study design. Fifty-eight chronic (> 3 months) stroke patients will be recruited from the Montpellier and Nimes University Hospitals. Patients will follow a standard 3-weeks in-patient rehabilitation program, which includes 13 days of VRT (Armeo Spring, 1x30min session/day) and conventional therapy (3x30min sessions/day). Twenty-nine patients will receive real stimulation (4×1 anodal HD-tDCS montage, 2mA, 20min) to the ipsilesional primary motor cortex during the VRT session and the other 29 patients will receive active sham stimulation (2mA, 30s). All outcome measures will be assessed at baseline, at the end of rehabilitation and again 3 months later. The primary outcome measure will be the wolf motor function test. Secondary outcomes will include measures of UL function (Box and Block test), impairment (Fugl Meyer Upper Extremity), compensation (Proximal Arm Non-Use), ADL (Actimetry, Barthel Index), pain, fatigue, effort and performance, kinematics and motor cortical region activation during functional motor tasks.
Discussion
This will be the first trial to determine the impact of adding HD-tDCS during UL VRT and conventional therapy in chronic stroke patients. We hypothesise that improvements in UL function will be greater and longer-lasting with real stimulation than in those receiving sham.[…]
Continue
[ARTICLE] Development of a Virtual Reality Simulator for an Intelligent Robotic System Used in Ankle Rehabilitation – Full Text
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, Rehabilitation robotics, Virtual reality rehabilitation on March 29, 2021

Abstract
The traditional systems used in the physiotherapy rehabilitation process are evolving towards more advanced systems that use virtual reality (VR) environments so that the patient in the rehabilitation process can perform various exercises in an interactive way, thus improving the patient’s motivation and reducing the therapist’s work. The paper presents a VR simulator for an intelligent robotic system of physiotherapeutic rehabilitation of the ankle of a person who has had a stroke. This simulator can interact with a real human subject by attaching a sensor that contains a gyroscope and accelerometer to identify the position and acceleration of foot movement on three axes. An electromyography (EMG) sensor is also attached to the patient’s leg muscles to measure muscle activity because a patient who is in a worse condition has weaker muscle activity. The data collected from the sensors are taken by an intelligent module that uses machine learning to create new levels of exercise and control of the robotic rehabilitation structure of the virtual environment. Starting from these objectives, the virtual reality simulator created will have a low dependence on the therapist, this being the main improvement over other simulators already created for this purpose.
1. Introduction
In parallel with the achievements in engineering in recent years, medicine has evolved a lot, but there are still unresolved problems. A rather important problem remains stroke in both its forms (ischemic and hemorrhagic) which is considered the leading cause of disability and the second leading cause of death worldwide [1], becoming a growing problem of contemporary society and any progress made in treating this disease is a step forward in the fight against this disease. Recovery after a stroke is different for each person, depending on the condition of each, and to make a successful recovery in both forms of stroke, treatment will often involve specific therapies and support, such as: speech therapy, occupational therapy, physical recovery post-AVC, support groups, support from friends and family [2]. Rehabilitation after a stroke should be done as soon as possible with intensive and repetitive exercises, although this may reduce the patient’s motivation. One way to motivate and help patients regain their motoric skills is to introduce virtual reality technology [3].
This article presents a simulator using virtual reality for a robotic system that is controlled by an intelligent module that uses machine learning to optimize the ankle recovery treatment of a stroke patients, using visual stimulation in the recovery process. The patient is in real-time interaction with the system via a special sensor device that is attached to the patient’s limb. On this device the sensors are connected to a microcontroller that contains a client application through which it sends data collected from the sensors via the Wi-Fi connection to a server application that is on the computer via the TCP/IP protocol, and this data is retrieved and processed by the intelligent module. This module uses a machine learning algorithm that will result in the type of exercise that the patient will perform and the level of difficulty of this exercise. The real person will be able to do various ankle rehabilitation exercises by interacting with the VR simulator. This simulator can be used in the home of any patient who has had a stroke, without incurring additional costs. Usually, a rehabilitation process takes place in specialized physiotherapy centres where a professional in the area supervises or helps.
A recent clinical study involving a number of 23 patients with different neuro-motor impairments demonstrated that following a 7-day rehabilitation program applied at the level of the upper limb, no significant differences were identified between the robotic assisted and the manual therapy. Taking into account that the robotic system used in this experiment is still in development the results are supporting the idea of using robotic systems in rehabilitation illustrating also the potential advantages that additional, support technologies could improve the outcome of physical therapy [4]. Moreover, the engagement of patients in the therapy could bring benefits for the rehabilitation procedures. In other words, if the patient is not bored and is actively engaged in the exercises (e.g., by playing games in an interactive way) the rehabilitation may have better outcomes by improving the patient’s motivation and reducing the work of the therapist [5].
This article is structured as follows: after introduction, the next section reviews the current state of the art, continuing with its robotic system architecture in Section 3. Section 4 presents development of the software application followed in Section 5 by conclusions, acknowledgments, and references. Compared to other rehabilitation systems, the robotic rehabilitation system presented in this paper has as a novelty the use of an intelligent module implemented using KNN. This intelligent module, based on the data provided by the sensors and the user’s previous results, can determine without the intervention of the therapist the level of difficulty of the exercise to be performed by the user.[…]
[BLOG POST] Weighted Blankets: Uses, Benefits, Risks, and Safety
Posted by Kostas Pantremenos in Uncategorized on March 28, 2021
What Is a Weighted Blanket?
Pros and Cons About the Popular “Pressure Therapy” Device
By Martta Kelly Medically reviewed by Steven Gans, MD
Weighted blankets, also known as gravity blankets, have been used for years by mental health professionals as a form of pressure therapy. Today, they have gained mainstream popularity with those who believe that the pellet-filled blankets, which weigh anywhere from 5 to 30 pounds, can relieve stress, improve sleep, calm children with attention deficit hyperactivity disorder (ADHD) or autism spectrum disorder (ASD), and aid in the treatment of anxiety disorders.
Although many people report improvements in their health and well-being from these popular blankets, there remains considerable debate as to whether they offer the benefits that proponents claim.
:max_bytes(150000):strip_icc():format(webp)/GettyImages-1257811910-122405448cf14ee2b02ec9fbb706e4b7.jpg)
Uses
Many adults associate snuggling under a comfy blanket with a sense of security, which harkens back to “security blankets” they may have had as a child. Blankets are often referred to as “comfort objects” by child psychologists—that is, an item used to ease frustration or anxiety at times of stress.1
An older study by psychologist and security object expert Richard Passman, now retired from the University of Wisconsin at Milwaukee, found that approximately 60% of children are attached to a toy, blanket, or pacifier during the first three years of life.2
More recent studies have examined adult attachment to transitional objects, such as blankets and stuffed animals. In one study using a non-clinical community sample of 80 participants, researchers found that people who reported intense attachments to objects were significantly more likely to meet the criteria for borderline personality disorder than those who did not; they also reported more childhood trauma.3
Weighted blankets aim to evoke the same therapeutic effects of a security blanket by intensifying the sensation of being held, stroked, cuddled, or squeezed.
The science behind using a weighted blanket is a well-known and proven relaxation therapy that is frequently used for people with stress and anxiety. Known by various names, it is commonly referred to as deep pressure stimulation (DPS).
DPS, offered by trained practitioners who apply pressure to certain parts of the body, stimulates what is known as the parasympathetic nervous system. The nervous system reacts to stressful situations naturally, by inducing its sympathetic or “alert” state, which can produce anxiety and stress. The parasympathetic system counterbalances this sympathetic activation.
DPS and weighted blankets can stimulate the parasympathetic response. When the parasympathetic nervous system kicks in, it can instill feelings of calm, slowing many of the body’s autonomic functions. There are also psychological calming effects, akin to being cocooned in your favorite duvet on a cold winter night, knowing you are protected from the outside world.4
Weighted blankets may help adults and children with sensory processing disorder feel calmer and more relaxed.5 Persons with this disorder have difficulty processing sensory information such as textures, sounds, smells, tastes, brightness, and movement.
These difficulties can make ordinary situations overwhelming, interfere with daily living, and even isolate individuals and their families. Sensory integration therapy uses activities in ways designed to change how the brain reacts to various stimuli.6
Applying deep pressure has also been shown to be beneficial for children with high levels of anxiety or arousal due to sensory overload. According to research, the application of deep pressure provided by a weighted vest or blanket can produce a calming or relaxing effect in children with certain clinical conditions who have sensory processing issues.5
Benefits
Although more studies are needed, research has been conducted on the use of weighted blankets to treat the following conditions:
- General anxiety
- Anxiety during certain medical procedures
- Insomnia
- Insomnia in children with autism spectrum disorder
- Sleep problems in children with ADHD
General Anxiety
Some studies show that the use of weighted blankets may help reduce nighttime levels of cortisol, a stress hormone that can contribute to anxiety.7 Cortisol is best known for being involved in the “fight or flight” response, a reaction that evolved as a means of survival, enabling people to react to what could be a life-threatening situation.
Over time, however, elevated cortisol levels can have a negative impact on a person’s physical and mental health.8 By providing deep pressure, weighted blankets can promote relaxation and help break this cycle. For example, one study examined the use of a 30-pound weighted blanket in a sample of 32 adults; 63% reported lower anxiety after using the blanket.9
Anxiety During Certain Medical Procedures
A 2016 study, believed to be the first one investigating the effect of deep pressure stimulation during wisdom tooth extraction, examined heart rate variability and anxiety in healthy adults using weighted blankets while undergoing the procedure. Researchers found that the weighted blanket group experienced lower anxiety symptoms than the control group.10
A similar follow-up study was performed a few years later on healthy adolescents using a weighted blanket during a molar extraction. Those results also found less anxiety in those using a weighted blanket.11
Since medical procedures tend to cause anxiety symptoms, such as increased heart rate, researchers concluded that weighted blankets may be beneficial in calming those symptoms.12
Insomnia
Most research on weighted blankets and insomnia has focused on their use in children with clinical disorders, such as ASD, as discussed below. However, the majority of these studies do not examine sleep objectively.
A Swedish study published in the Journal of Sleep Medicine & Disorders concluded that the use of weighted blankets had a positive impact on sleep, both objectively and subjectively, where a number of physiological and behavioral measures were improved in a cohort of 31 adults. However, the study was biased in that it was conducted by a blanket manufacturer and had design limitations, such as the lack of a control group.5
A systematic literature review, which evaluated eight studies, concluded that while weighted blankets have the potential to be beneficial in limited settings and populations and may be an appropriate therapeutic tool in reducing anxiety, there is not enough evidence to suggest that they are beneficial in alleviating insomnia.13
Insomnia in Children with ASD
Children with ASD sleep poorly compared with their peers. A study published in Pediatrics involving 67 children with ASD found that the use of a weighted blanket did not help them fall asleep significantly faster, sleep for a longer period of time, or awaken less often.14
Sleep Problems in Children with ADHD
Similarly to children with ASD, many children with ADHD have sleep disturbances, such as trouble falling asleep and waking up several times throughout the night. Unlike children with ASD, however, weighted blankets proved useful in some instances in children with ADHD who had difficulty sleeping.
A study involving 21 children ages 8 to 13 years with ADHD and 21 healthy controls found that the use of a weighted blanket improved the time it took to fall asleep and the number of awakenings.15
A more recent study examined 120 patients who were randomized (1-to-1) to either a weighted metal chain blanket or a light plastic chain blanket for four weeks. Researchers found that weighted chain blankets are an effective and safe intervention for insomnia in patients with ADHD and other psychiatric disorders.16
It is important to note that, despite positive findings in several of these studies, they are limited by their small size, short duration, and/or lack of diverse subjects. Further research on the benefits of weighted blankets is needed in all of these therapeutic areas.
Other Conditions
Although there have been studies on the benefits of massage therapy for osteoarthritis and chronic pain, there is currently no evidence that weighted blankets are effective in the treatment of these conditions.
Some manufacturers make unsubstantiated claims about weighted blankets benefiting certain health and psychological conditions, but, ultimately, it’s up to the consumer to do their own research and make an educated decision.
Risks
As a general rule, weighted blankets are safe for healthy adults, older children, and teenagers. Weighted blankets, however, should not be used for toddlers under age 2, as they may pose a suffocation risk. Even older children with developmental disabilities or delays may be at risk of suffocation.
There have been at least two reports of deaths in children due to weighted blankets, one in a 7-month-old baby and one in a 9-year-old boy who had autism.17 Parents should consult their pediatrician before using a weighted blanket for children of any age.
People with certain health conditions should also avoid weighted blankets. These include chronic respiratory conditions, such as asthma, chronic obstructive pulmonary disease (COPD), and obstructive sleep apnea.
In addition, a weighted blanket may also be unsuitable for those people who are claustrophobic, as it may cause anxiety rather than ease it.
Safety
As a general rule, a weighted blanket should be 10% of an adult person’s body weight, according to most manufacturers’ websites. Other guidelines include:18
- Adults can use medium-to-large weighted blankets ranging from 12 to 30 pounds.
- For a 30- to 70-pound child, a small weighted blanket should weigh from 5 to 8 pounds.
- For a 30- to 130-pound child, a medium-weighted blanket should weigh from 5 to 15 pounds.
Young children should never be left unsupervised with a weighted blanket, particularly those made for an adult.18
A Word From Verywell
While there is no conclusive evidence that weighted blankets are effective for the treatment of any health condition, they are popular with many people due to the comfort they provide.
Some studies have shown positive results in reducing anxiety and helping children with ADHD get a good night’s sleep. If you are a healthy adult, there is little risk of trying one—other than to your wallet, as they start around $100.
[Abstract] Why is music therapeutic for neurological disorders? The Therapeutic Music Capacities Model
Posted by Kostas Pantremenos in Music/Music therapy on March 28, 2021
Abstract
Music has cognitive, psychosocial, behavioral and motor benefits for people with neurological disorders such as dementia, stroke, Parkinson’s disease (PD) and Autism Spectrum Disorder (ASD).
Here we discuss seven properties or ‘capacities’ of music that interact with brain function and contribute to its therapeutic value. Specifically, in its various forms, music can be engaging, emotional, physical, personal, social and persuasive, and it promotes synchronization of movement. We propose the Therapeutic Music Capacities Model (TMCM), which links individual properties of music to therapeutic mechanisms, leading to cognitive, psychosocial, behavioral and motor benefits.
We review evidence that these capacities have reliable benefits for people with dementia, stroke, PD and ASD when employed separately or in combination. The model accounts for the profound value that music affords human health and well-being and provides a framework for the development of non-pharmaceutical treatments for neurological disorders.
