Posts Tagged lower extremity
[NEWS] Intensive rehabilitation can provide improvements long after stroke event
Posted by Kostas Pantremenos in Constraint induced movement therapy CIMT, Gait Rehabilitation - Foot Drop on November 25, 2023
by Claes Björnberg, Umea University

Lower-extremity constraint-induced movement therapy (LE-CIMT), i.e., high-intensity treatment with exercise six hours a day for two weeks, appears to improve the function of the leg and the ability to walk and move in its environment. The improvements are seen even if a long time has passed since the stroke, and the achieved effects were maintained, as shown in a new thesis by Ingela Marklund.
LE-CIMT is a treatment option that can be performed both in day rehabilitation in hospital and in outpatient care. People with stroke treated with LE-CIMT were interviewed for the study. Based on the patient’s ability to walk a distance of six minutes, their health-related quality of life in terms of physical function can be predicted, emphasizing the importance of walking and locomotion training in post-stroke rehabilitation.
“We found that the high-intensity treatment produced significant improvements in leg function with increased strength, improved balance and the ability to walk and do two things at the same time,” says Marklund, Department of Community Medicine and Rehabilitation.
Remaining improvements
In addition, walking speed and the ability to walk a longer distance improved in people with stroke. They maintained or even improved their weight bearing on the more affected leg to a more symmetrical load in standing. The improvements achieved were maintained at follow-up three and six months after the end of treatment.
“We also found a strong correlation between time since illness and age in the functional tests that were carried out. Those who completed LE-CIMT within six months of their illness improved their walking speed to a greater degree than those who completed LE-CIMT after seven months or more. Younger participants had better balance than older ones in one of the balance tests.”
Analysis of the interviews conducted about the participants’ experiences generated an overarching theme, that the LE-CIMT gave them knowledge about themselves and how their body works. This knowledge facilitated the possibility of living life more easily. They felt that there was still hope and opportunity for functional improvement, which gave them increased independence and self-esteem. Although the treatment was intense and challenging, it was felt to be absolutely necessary.
Increased participation
Compared to the general population in Sweden, the participants had a significantly lower health-related quality of life in terms of physical function, physical capacity, general health and social function. There was a strong correlation between their results on the six-minute walk test and the physical function domain.
“With increased function in the affected leg, conditions are created for increased participation in society for those who suffer a stroke. Strength, balance and the ability to walk and do two things at the same time are important factors in reducing the risk of falling,” says Marklund.
More information: Lower-extremity constraint-induced movement therapy in individuals with stroke—Improvements, experiences and health-related quality of life. umu.diva-portal.org/smash/record.jsf?pid=diva2%3A1807834&dswid=3870
Provided by Umea University
[ARTICLE] Lower-extremity constraint-induced movement therapy improved motor function, mobility, and walking after stroke – Full Text
Posted by Kostas Pantremenos in Constraint induced movement therapy CIMT, Gait Rehabilitation - Foot Drop on April 24, 2023
ABSTRACT
BACKGROUND: To regain the ability to walk is one of the most commonly stated goals for people who have had a stroke due to its importance in everyday life. Walking ability affects patients’ mobility, self-care, and social lives. Constraint-induced movement therapy (CIMT) is known to be effective in improving upper extremity outcomes post-stroke. However, there is insufficient evidence regarding its efficacy in improving lower extremity outcomes
AIM: To investigate whether a highly intensive CIMT for lower extremity (LE-CIMT) function post-stroke can improve motor function, functional mobility, and walking ability. Furthermore, it also aimed to investigate whether age, gender, stroke type, more-affected side, or time after stroke onset affect the efficacy of LE-CIMT on walking ability outcomes.
DESIGN: Longitudinal cohort study.
SETTING: Outpatient clinic in Stockholm, Sweden.
POPULATION: A total of 147 patients mean age 51 years (68% males; 57% right-sided hemiparesis), at the sub-acute or chronic phases post-stroke who had not previously undergone LE-CIMT.
METHODS: All patients received LE-CIMT for 6 hours per day over 2 weeks. The Fugl-Meyer Assessment (FMA) of the lower extremity, Timed Up and Go (TUG) test, Ten-Meter Walk Test (10MWT), and six-Minute Walk Test (6MWT) were used to assess functional outcomes before and directly after the 2-week treatment was complete as well at 3-month post-intervention.
RESULTS: Compared to baseline values, FMA (P<0.001), TUG (P<0.001), 10MWT (P<0.001) and 6MWT (P<0.001) scores were statistically significantly improved directly after the LE-CIMT intervention. These improvements persisted at the 3-month post-intervention follow-up. Those who completed the intervention 1-6 months after stroke onset had statistically significant larger improvements in 10MWT compared to those who received the intervention later than 6 months after stroke onset. Age, gender, stroke type, and more-affected side did not impact 10MWT results.
CONCLUSIONS: In an outpatient clinic setting, high-intensity LE-CIMT statistically significant improved motor function, functional mobility, and walking ability in middle-aged patients in the sub-acute and chronic post-stroke phases. However, studies with more robust designs need to be conducted to deepen the understanding of the efficacy of LE-CIMT.
CLINICAL REHABILITATION IMPACT: High-intensity LE-CIMT may be a feasible and useful treatment option in outpatient clinics to improve post-stroke walking ability.
Regaining their walking ability is one of the most commonly stated goals for patients in post-stroke rehabilitation.1 Walking ability is of high importance for everyday life, as it affects patients’ mobility, self-care, and social lives.2, 3 While 50-80% of all stroke patients regain the ability to walk,4 over 60% experience an abnormal gait pattern and reduced walking ability.5 Abnormal gait patterns also occur in the unaffected half of the body due to compensatory movements in the arms, torso, pelvis, and legs.5, 6 Stroke patients walk slower, have higher energy consumption, and are at an increased risk of falling.7, 8 They quickly become exhausted, causing them to often opt out of various activities, limiting their participation in social activities and impacting their quality of life.2, 3 Reduced walking ability and overall mobility can present challenges for patients to resume activities in daily living (ADL), work, and leisure activities.9 However, walking ability and mobility can be improved using evidenced-based rehabilitation.
Constraint-induced movement therapy (CIMT) was developed in line with neurophysiological research and the knowledge regarding the brain’s plasticity and ability to reorganize itself.10 Brain reorganization is impacted by injury location, injury size, time since onset, biological age, and treatment-induced behaviour changes.11 CIMT has been shown to be effective in improving upper extremity outcomes post-stroke.12, 13 CIMT consists of four components: 1) intensive training of the more affected arm; 2) training with a behavioral technique called shaping; 3) the ‘transfer package,’ where problem-solving is used to overcome perceived barriers to more-affected arm use in ADL; 4) restraint of the less affected arm for 90% of waking hours during the treatment period.10 However, the restraint component has been found to have little influence on outcomes.14
A recent systematic review evaluated the effectiveness of CIMT for the lower extremity (LE-CIMT).15 The 16 studies included in the review used diversified designs and treatment lengths to investigate LE-CIMT and shown improvements in motor function, balance, mobility, gait speed, oxygen uptake, weight-bearing, lower limb kinematics, and quality of life in stroke patients. In the meta-analysis of 6 randomised controlled trials,16-20 significant improvements were only found in quality of life post-intervention and during follow-ups. However, only two of the included studies21, 22 with an experimental design had an intervention that lasted 6 hours a day for 2 weeks, and neither was included in the meta-analysis. The use of restraint in LE-CIMT presents a challenge. As humans are bipedal, two legs are often required for most daily activities, particularly during walks. However, there is insufficient evidence regarding the efficacy of LE-CIMT as limited studies investigating this have been published, and those that have been only involve a small number of participants.15
This study aims to investigate whether LE-CIMT (i.e., highly intensive task-specific training for the lower extremity) can improve motor function, functional mobility, and walking ability among post-stroke patients in an outpatient clinical setting. Whether age, gender, stroke type, more-affected side, or time after stroke onset affect the efficacy of LE-CIMT on walking ability outcomes will also be investigated.[…]
[VIDEO] The 10 most viewed neurology videos on Youtube – The Neurology Lounge
Posted by Kostas Pantremenos in Video on November 28, 2022
The Neurology Lounge has already reviewed the changing terrain of neurology, throwing a light on the increasing role of social media, online video sites, and online databases, all competing and complementing the classroom and the clinic. Our previous posts on this subject include:
Outstanding neurology video channels and sites
Which are the most reliable neurology reference sources?
Which are the most useful neurological applications?
Youtube remains the clear leader when it comes to videos. Buried among the cat and dog snippets, hiding behind the crazy stunts and funny clips, and camouflaged by the ubiquitous vlogs, are many enlightening neurological stuff. And of the many neurology videos on Youtube, some have attracted more attention than others. Is there a secret? There’s only one way to find out!
Here then are the top 10 most viewed neurology videos on Youtube:
10.
9.
8.
7.
6.
5.
4.
3.
2.
1.
***
If there is any lesson here, it’s all about the simple things. No complicated syndromes, no convoluted guidelines. In some cases, no master at all! Viewers just want to see the complex simplified!
PS. To widen the variety of video sources, I have restricted each source to one video.
[BLOG POST] The VR Device For ALL Your Rehab Needs.
Posted by Kostas Pantremenos in REHABILITATION, Virtual reality rehabilitation on November 26, 2022


-Shoulder & Elbow Function
-Grip & Release Strengthening
-Gross Muscle Strengthening
-Upper Extremity Robotic Compatible
-Functional Reaching

-Hip, Knee, & Ankle Function
-Gross Muscle Strengthening
-Bike, Nu-Step, & Standing Frame Compatible
-Weight Bearing & Weight Shifting

-Cervical ROM
-Cervical & Trunk Proprioception
-Vestibular Rehab
-Posture
-Functional Balance & Stability
-Weight Shifting & Weight Bearing

-Chronic/Acute Pain
-Distraction
-Controlled Breathing
-Decompression
-Anxiety Alleviation

-Audio Que Recognition
-Visual-Spatial Awareness
-Attention
-Money Management
-Listening Skills

-Functional Reaching
-Functional Balance and Stability
-Grocery Shopping
-Money Management
[ARTICLE] Effects of a lower limb rehabilitation robot with various training modes in patients with stroke: A randomized controlled trial – Full Text
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, Rehabilitation robotics on November 16, 2022
Abstract
Background:
The effect of robot-assisted gait training has been demonstrated to improve gait recovery in patients with stroke. The aim of this study was to determine effects of robot-assisted gait training with various training modes in patients post stroke.
Methods:
Forty-seven patients post stroke were randomly assigned to one of 4 groups: Healbot T with pelvic off mode (pelvic off group; n = 11); Healbot T with pelvic control mode (pelvic on group; n = 12); Healbot T with constraint-induced movement therapy (CIMT) mode (CIMT group; n = 10); and conventional physiotherapy (control group; n = 10). All patients received a 30-minute session 10 times for 4 weeks. The primary outcomes were the 10-meter walk test (10MWT) and Berg Balance Scale (BBS). The secondary outcomes were functional ambulation category, timed up and go (TUG), and motricity index of the lower extremities (MI-Lower).
Results:
The pelvic off group showed significant improvements in BBS, TUG, and MI-Lower (P < .05). The pelvic on and CIMT groups showed significant improvement in 10MWT, BBS, TUG, and MI-Lower (P < .05). Compared with control group, the pelvic on group showed greater improvement in the TUG and BBS scores; the CIMT group showed greater improvement in 10MWT and MI-Lower (P < .05).
Conclusion:
This study suggested that Healbot T-assisted gait training benefited patients with stroke. The Healbot T with pelvic motion and CIMT modes were more helpful in improving balance and walking ability and lower limb strength, respectively, compared with conventional physiotherapy.
1. Introduction
Stroke is one of the main causes of acquired disability.[1] Many patients experience gait impairments after a stroke. There are many available rehabilitation therapies that are beneficial for motor and gait recovery in patients post stroke such as cycling, treadmill walking, and functional electrical stimulation (FES).[2,3] Bilateral FES in conjugation with treadmill walking and FES with cycling improved gait function. The recently preferred treatment concept is task-oriented, repetitive, and high-intensity physical therapy.[4] The current rehabilitation treatments being performed are inefficient and ineffective due to the physical burden.[1,5–7] Various methods and systems are being developed to solve these problems and provide effective rehabilitation. Robot-assisted rehabilitation is not only suitable for applying intensive and repetitive training according to the disability level of the patients but also has the advantage of preventing falls when using a weight support system.[1,4,6,8]
Pelvic movements, including pelvic rotation, pelvic tilt, and pelvic dislocation, are important for efficient walking and overall posture.[9] Abnormal pelvic movements while walking in patients with stroke affect trunk and pelvis rotation and lower extremity stability, resulting in decreased balance and walking ability. Furthermore, prolonged incorrect posture produces inadequate tension in adjacent muscles and joints, causing pain.[10] However, most robotic devices for gait training on the market usually fix the pelvis, which may limit gait training robots.[11]
Constraint-induced movement therapy (CIMT) has been proven an efficient rehabilitation approach in the paretic upper limb after stroke.[12] This therapy stimulates the use of the paretic limb, decreasing the effects of learned disuse and helping to promote positive changes in the brain structure and function. Although CIMT of paretic lower limbs has fewer studies than the upper limb, applying this technique to the lower limbs has had good results with important motor function and functional activities performed with these limbs after stroke.[12]
There are several studies on the effect of robot therapy on the improvement of functional gait in patients with stroke.[13,14] However, few studies regarding robot therapy use a gait training system, including the concept of movement control through pelvic motion and CIMT in lower extremities.[15,16] Healbot T is a new exoskeleton-type lower limb rehabilitation robot. Unlike other robot devices used for gait therapy, it provides pelvic movement, including pelvic rotation and lateral translation and CIMT that limits the range of motion of the healthy-side lower limb during gait. The effect of pelvic movements of a gait training system using Healbot T for patients post stroke were demonstrated.[17] However, there have been no studies on the effects of various modes of Healbot T. This study aimed to investigate the effects of Healbot T-assisted gait training with various training modes in patients with stroke.[…]
Healbot T. (A) Schematics of the Healbot T. (B) Overview of Healbot T-assisted gait training with 3 modes (pelvic off, pelvic on, and constraint-induced movement therapy [CIMT] modes). The pelvic on mode provides pelvic movements such as pelvic rotation and lateral translation during gait; the CIMT mode limits the range of motion of joints of the healthy-side lower limb and provides pelvic movement; the pelvic off mode fixes the pelvis and allows both legs to move symmetrically during gait.
[Abstract] Constraint-induced movement therapy for lower extremity use in activities of daily living in people with chronic hemiparesis – multiple case study
Posted by Kostas Pantremenos in Constraint induced movement therapy CIMT, Gait Rehabilitation - Foot Drop on August 10, 2022
Abstract
Lower extremity constraint-induced movement therapy (LE-CIMT) is an intensive intervention protocol recently reported to improve lower extremity use in individuals with chronic hemiparesis. To test if the LE-CIMT that uses essential CIMT components, including the transfer package and intensive task-oriented training, is a feasible and potentially effective intervention to improve the lower extremity real-world use and functional ability in a group of individuals with chronic hemiparesis. A quasi-experimental pre- and post-test design study with 12 individuals with chronic stroke and impaired ambulation skills engaged in a 10-weekday LE-CIMT. Intervention feasibility was assessed, examining the training adherence, acceptability, and safety. The lower extremity motor activity log (LE-MAL), lower extremity motor function test (LE-MFT), timed up and go (TUG) and spatiotemporal gait parameters were used as clinical outcomes. Clinical data were collected at baseline, 3-day post-CIMT protocol and 30-day follow-up assessment. At baseline, LE-MAL and LE-MFT outcomes were tested over 2-week apart to ensure a stable measurement and determine the smallest real difference (SRD) in the study sample. The LE-CIMT showed excellent adherence, acceptability and safety. Ten out of 12 participants showed improvements over SRD in LE-MAL composite score (1.2 point) and eight participants in LE-MFT adjusted scores (0.8 point) in post-CIMT and 30-day follow-ups. LE-CIMT is a feasible intervention that has the potential to promote improvements in real-world use and functional ability of the paretic lower extremity in individuals with chronic stroke.
[ARTICLE] A Novel Virtual Reality Training Strategy for Poststroke Patients: A Randomized Clinical Trial – Full Text
Posted by Kostas Pantremenos in Virtual reality rehabilitation on July 17, 2022
Abstract
Stroke patients suffer impairments including sensory, motor, visual, and cognitive areas, as well as gait and balance manifestations making activities of daily living difficult. In such conditions, virtual reality training can be a potential rehabilitation tool in comparison to conventional physical therapy to cater to the burden of this disability; hence, this randomized clinical trial compared the effects of virtual reality training and conventional physical therapy on balance and lower extremity function in stroke patients. The sample of 68 poststroke participants from Kanaan Physical Therapy and Spine Clinic, Lahore, Pakistan, were divided into N = 34 cases each using the lottery method with one group given virtual reality training and the other received conventional physical therapy. Each group received 60 minutes intervention, 3 days per week for 6 weeks. The Berg balance scale and the Fugl-Meyer assessment-lower extremity scale were employed for data collection preintervention, immediate postintervention, and 6 weeks postintervention. The statistically significant differences between virtual reality and conventional physical therapy groups for the Berg Balance score (), Fugl-Meyer assessment (FMA)-lower extremity domains of FMA-motor function (), FMA-joint pain, and joint range (); however, there is no significant difference for time vs. group interaction and significant () for the time main effect for FMA sensation. Hence, virtual reality training is more effective to restore balance and lower extremity function compared to conventional physical therapy in stroke patients. The results of the study have significant implications for the clinicians with better case management enhancing quality of life of patients along with the dearth of local literature, thus providing base for future research from a developing country’s perspective.
1. Introduction
Stroke or cerebrovascular accidents (CVA) are considered as the leading cause of disability globally with more youth being affected in developing countries [1]; however, there is equal gender prevalence marring quality of life (Qol) at every level. Stroke has a global lifetime risk of 24.9% estimated in 2016 and extrapolated estimates by 2030 with 4% of population having a stroke event during the lifetime mounting medical costs to $ 183.13 billion [2]. The patients with stroke may have a wide variety of impairments in motor, sensory, visual, and cognitive areas including gait deficits and balance-related manifestations [3]. Hence, they experience restrictions to participate in activities of daily living (ADLs) and compromising the Qol. In addition to improved preventive and acute care facilities, neurorehabilitation is a ray of hope to cater to the burden of disability among this population [1, 4].
Looking at the prospects of mobility, conventional physical therapy (PT) is employed in lower limb rehabilitation including exercises and certain balance techniques. A study by de Rooij et al. involving community dwellers examined by virtual reality (VR) gait training and non-VR gait training containing conventional functional gait exercises and treadmill training was seen as effective in stroke patients; however, VR training showed better results compared to conventional therapeutic interventions [5].
Researchers have elaborated on the advancement of the neuroplastic changes connected with poststroke motor impairment and the inherent repair mechanisms [6]. An important role has been determined with PT focusing on the sensory input reflecting improvement in the neuroplasticity with sensory and motor learning [7]. When the patient observes his/her movements, the plasticity changes that depend on the use of sensory areas belonging to the mirror neuron system are strengthened. This exemplifies, among other factors, the improvements the Wii can provide in such patients. Moreover, this feedback could lead to a strengthening of the learning mechanisms of different motor and sensory activities that would ultimately improve quality of life [8].
The poststroke balance rehabilitation using different therapies is in use, and further research has been proposed [9]. A local study by Saleem has also emphasized on the need of clinical trials comparing VR gaming with conventional rehabilitation for stroke patients in Pakistan [10].
VR has achieved a greater attention in recent times, and it is an adjuvant rehabilitation method capable of producing neuroplasticity with the help of visual, sensory, as well by evoking cognitive interactions at the intercortical level. Its application by robotics has shown to restore the lower limb function by inducing neuroplasticity [11]. A number of randomized clinical trials have appraised the Nintendo Wii-based rehabilitation of stroke patients especially the balance. The research by Cho et al. worked on the balance training of stroke patients by using Nintendo Wii gaming. The results showed significant improvement of dynamic balance [12]. In contrast, another study conducted by Fritz et al. [13] revealed only slight improvement in balance in the Nintendo Wii group as compared to the control group. While VR has shown improvement in motor function and functional capacity in Nintendo Wii®, electronic game for the stroke survivors to improve sensorimotor rehabilitation [14] has shown to have higher impact on improvement of balance and fall prevention than conventional PT [15]. It has also been noted to be cost-effective therapeutic intervention [16] and hence needs to be considered for a developing country like Pakistan.
Stroke is 5–10 times more prevalent in certain countries including Pakistan compared to the west, with South Asia sharing 20% of the world’s population and shouldering the highest burden of cardiovascular disease. This is marred with high incidence of stroke in the middle-aged group with 1/3rd strokes occurring in those <45 years age accompanied with more prevalent risk factors especially nontraditional ones including the use of local drugs like naswar, smoking of pipe, and chewing betel leaf (paan) and higher incidence of diseases like rheumatic heart disease and liver diseases [17–19]. This is also associated with higher prevalence of hypertension at younger age with increased frequency of lacunar infarcts among ischemic stroke, a subtype of stroke in Pakistan that differs from Western literature as reported [20–22]. With the rate of prevalence and the fact is that Pakistan, harbouring a young population of 63% aged between 15 and 33 years, could be facing a grave health peril [23]. Hence, the need to focus on younger age groups for research seems inevitable. Good posture and adequate balance maintenance are essential prerequisites for performing active ADLs and therefore should be targeted in rehabilitation interventions [12].
Thus keeping in view the unique position of stroke in Pakistan with epidemiological and the clinical dissimilarities with the Western literature, especially due to the involvement of the younger population and the cost-effectiveness of VR, there is a need to establish the fact that neurorehabilitation using virtual therapy to improve the balance and gait of poststroke cases is a better option compared to conventional therapies, and in this connection, there is need of randomized clinical trials (RCT) for evaluation of impact of VR on balance [24].
Hence, this study was conducted to compare the effects of VR training and routine PT on balance and lower extremity function in stroke patients, with the hypothesis that VR training is better than conventional PT for balance and lower extremity function restoration in 40–60 years old stroke patients.[…]
[ARTICLE] Effects of control strategies on gait in robot-assisted post-stroke lower limb rehabilitation: a systematic review – Full Text
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, Rehabilitation robotics on June 9, 2022
Abstract
Background
Stroke related motor function deficits affect patients’ likelihood of returning to professional activities, limit their participation in society and functionality in daily living. Hence, robot-aided gait rehabilitation needs to be fruitful and effective from a motor learning perspective. For this reason, optimal human–robot interaction strategies are necessary to foster neuroplastic shaping during therapy. Therefore, we performed a systematic search on the effects of different control algorithms on quantitative objective gait parameters of post-acute stroke patients.
Methods
We conducted a systematic search on four electronic databases using the Population Intervention Comparison and Outcome format. The heterogeneity of performance assessment, study designs and patients’ numerosity prevented the possibility to conduct a rigorous meta-analysis, thus, the results were presented through narrative synthesis.
Results
A total of 31 studies (out of 1036) met the inclusion criteria, without applying any temporal constraints. No controller preference with respect to gait parameters improvements was found. However, preferred solutions were encountered in the implementation of force control strategies mostly on rigid devices in therapeutic scenarios. Conversely, soft devices, which were all position-controlled, were found to be more commonly used in assistive scenarios. The effect of different controllers on gait could not be evaluated since conspicuous heterogeneity was found for both performance metrics and study designs.
Conclusions
Overall, due to the impossibility of performing a meta-analysis, this systematic review calls for an outcome standardisation in the evaluation of robot-aided gait rehabilitation. This could allow for the comparison of adaptive and human-dependent controllers with conventional ones, identifying the most suitable control strategies for specific pathologic gait patterns. This latter aspect could bolster individualized and personalized choices of control strategies during the therapeutic or assistive path.
Introduction
In the context of the digital revolution, there is a new paradigm for which digitalisation is approached in a sustainable and accessible way. Data is seen as a resource with great potential for the improvement of social and economic problems, as well as the growth of productivity and innovation.
In this framework, robotics has an important role in collecting new patient-specific data and using it to provide support during therapy or daily life assistance, especially when leveraging exoskeletons with embedded Artificial Intelligence (AI) algorithms. Nowadays, AI algorithms are increasing the implementation efficacy of learning processes and are capable of collecting and labelling new data almost instantly. This, viewed through the iron triangle framework of healthcare systems, could bolster accessibility, improving quality while cutting costs [1, 2]. In healthcare, the application of such a new framework could lead to improvements in terms of personalised therapies or innovative treatments. Moreover, in an assistive context, user-tailored devices could promote their accessibility and distribution in daily life, fostering the long-term improvement of the quality of life of patients in chronic conditions. […]
[ARTICLE] Active Assistive Design and Multiaxis Self-Tuning Control of a Novel Lower Limb Rehabilitation Exoskeleton – Full Text
Posted by Kostas Pantremenos in Mirror therapy, Rehabilitation robotics on May 3, 2022
Abstract
This paper presented the mechanical design and control of a lower limb rehabilitation exoskeleton named “the second lower limb rehabilitation exoskeleton (LLRE-II)”. The exoskeleton with a lightweight mechanism comprises a 16-cm stepless adjustable thigh and calf rod. The LLRE-II weighs less than 16 kg and has four degrees of freedom on each leg, including the waist, hip, knee, and ankle, which ensures fitted wear and comfort. Motors and harmonic drives were installed on the joints of the hip and knee to operate the exoskeleton. Meanwhile, master and slave motor controllers were programmed using a Texas Instruments microcontroller (TMS320F28069) for the walking gait commands and evaluation boards (TMS320F28069/DRV8301) of the joints. A self-tuning multiaxis control system was developed, and the performance of the controller was investigated through experiments. The experimental results showed that the mechanical design and control system exhibit adequate performance. Trajectory tracking errors were eliminated, and the root mean square errors reduced from 6.45 to 1.22 and from 4.15 to 3.09 for the hip and knee, respectively.
1. Introduction
The mobility of the aging population is restricted owing to sarcopenia or physical disabilities. An exoskeleton is a wearable orthosis that provides human body assistance via integrated robotic mechanisms. Exoskeletons started being investigated many decades ago and have garnered significant interest owing to the current development of the aging society [1,2,3,4,5].
In the 1960s, the exoskeleton “Hardiman”, which is powered by electrical motors and a master–slave control system, was the first exoskeleton to be developed by General Electric Company; however, it failed to operate as intended owing to its complex and heavy structure [6]. Recently, researchers at Tsukuba University developed a hybrid assistive limb (HAL) for patients with lower-limb illnesses. The HAL comprises posture and power-assist control and is powered by motors and a hybrid controller. Electromyography (EMG) sensors were installed on the HAL to capture foot reaction forces and detect the walking intention of the wearer [7]. Meanwhile, the Berkeley lower-extremity exoskeleton is an anthropomorphic model comprising seven degrees of freedom (DOFs) per leg, four of which are powered by linear hydraulic actuators. The exoskeleton enables the wearer to carry significant loads with minimal effort over different terrains. Furthermore, it allows various payloads to be mounted on a backpack-like frame [8,9].
More recently, the Harbin Institute of Technology proposed a lower-limb exoskeleton (LLE) to assist wearers in different situations. They used fuzzy logic to detect gait phases and a hybrid control strategy to improve stability and tracking precision [10]. At the Hefei University of Technology, a two-DOF LLE robot system with uncertainties and external disturbances was developed by optimizing the adaptive robust control and control gain parameters [11]. In another study, a lower-limb empowered rehabilitation named “moving up” was proposed. An adaptive fuzzy control scheme was introduced to achieve stable operation control for the assistant rehabilitation system, and the results showed that the system satisfied the requirements of the elderly [12]. For servo drive control, the dependence of the maximum bandwidths of servo drives on the sampling strategy and control design parameters was presented in [13]. An online auto-tuning method for the servo control loops of servo drives was proposed, where controller gains are tuned automatically by searching for the optimal bandwidth and identifying inertia [14]. Meanwhile, a multi-loop modulation method for servo drives applied to LLEs was proposed in another study [15], which resulted in improved system response and stability. Other controller developments, such as an improved particle swarm optimization adaptive PID controller, were proposed [16], based on which the human–exoskeleton system can operate effectively for trajectory tracking. An adaptive adjustment strategy was developed for a single-legged exoskeleton robot [17]. The algorithm for motions uses the walking data of the user to predict the joint angle data of the exoskeleton and achieve adaptive adjustment. A precision interaction force controller was proposed for a hydraulic leg exoskeleton [18]. Furthermore, a gain-tuning method was proposed to facilitate controller gain selection.
Previous studies typically focused on the mechanisms, medical applications, commercial equipment, and control methods of rehabilitation LLEs [19,20,21,22,23,24]. One of the control strategies is surface electromyography (sEMG)-based control, whose concept is based on human intent decoded from the electrical activities of muscles [25]. Electroencephalography-based control offers the advantages of direct volitional control, and a wearer with severe paralysis can command the exoskeleton [26]. Hybrid exoskeleton control has been used to assist walking and sit-to-stand tasks, where the hybrid exoskeleton is a rehabilitation device that combines functional electrical stimulation with robotic exoskeletons [27]. The authors of ref. [28] used a musculoskeletal simulator with trajectory tracking to estimate the gait phases of the wearer. Meanwhile, the authors of ref. [29] implemented a novel fuzzy logic algorithm to control the stroke of the hydraulic cylinder of an LLE robot using the angle of the hip and the stance or swing phase.
Not only the mechanical design but also the control strategy is an important factor for the development of exoskeletons. A suitable controller design can yield improved efficiency, particularly in rehabilitation exoskeletons, which must provide discreet safety, stability, and error tracking. Although the design and control of LLEs have been investigated, problems such as variable limb length, limited loading, and compact mechanical design remain unresolved. Therefore, in this study, the second lower-limb rehabilitation exoskeleton (LLRE-II) was developed to assist the wearer in motion. The study design of LLRE-II is illustrated in Figure 1. Figure 1a depicts the mechanical design of LLRE-II. Figure 1b,c illustrate the multiaxis motor system and control system development of LLRE-II, respectively. The system setup is illustrated in Figure 1d. The LLRE-II design comprises mechanical design, motor system design, and control system development. The main contributions of this study are as follows.
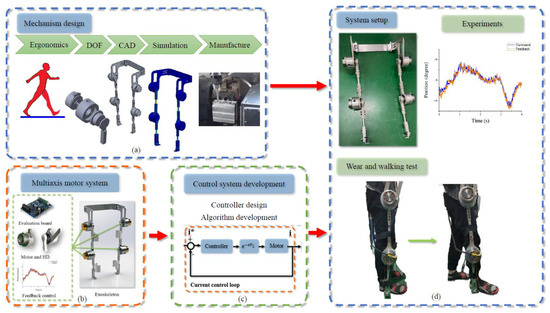
Figure 1. Study design of the LLRE-II. (a) Mechanical design, (b) multiaxis motor system, (c) control system development, and (d) system setup.
- A mechanical design involving a stepless (continuous variable lengths) adjustable length was adopted in the novel exoskeleton. To ensure the fit and comfort of the wearer, the axes of rotation were designed on the waist and ankle joints. The entire LLRE-II system weighed 16 kg.
- A multiaxis (multiple motor control) system was established. Planar motors were installed at the hips and knees of the LLRE-II. Harmonic drives (HDs) were fixed using a connecting plate to the motors to enhance the torque of each joint. The motor drive strategy was based on field-oriented control, including Clarke and Park transformations.
- The performance of the control system was evaluated. The trajectory tracking of the exoskeleton hip joint and knee during movement was achieved via a designed self-tuning controller. The responses of the exoskeleton system were analyzed.
[Abstract + References] A Novel Center of Mass (CoM) Perception Approach for Lower-Limbs Stroke Rehabilitation – Conference paper
Posted by Kostas Pantremenos in REHABILITATION on April 22, 2022
Abstract
Lower limb rehabilitation robots are of great significance for poststroke patients to regain locomotion ability. However, most rehabilitation robots fail to take the movement of CoM of human body into account. Considering that CoM is an essential index to assess the recovery effect and improve the treatment, we propose a simple, economic, portable, and highly efficient CoM perception approach based on Kinect camera. This novel method is capable of detecting the displacement and rotation of CoM in multi-planes. Results of walking tests show that our approach has competitive performance in capturing the variation trends of CoM compared with multi-cameras motion capture system, especially in some directions with large displacement variation. The high accuracy, simple and low-cost detection of CoM is a major step forward towards practical application in the assessment of rehabilitation after stroke.
References
- Detrembleur, C., van den Hecke, A., Dierick, F.: Motion of the body centre of gravity as a summary indicator of the mechanics of human pathological gait. Gait Posture 12, 243–250 (2000)CrossRef Google Scholar
- Forrester, L.W., Wheaton, L.A., Luft, A.R.: Exercise-mediated locomotor recovery and lower-limb neuroplasticity after stroke. J. Rehab. Res. Dev. 45(2), 205–220 (2008)Google Scholar
- Lin, J., Hu, G., Ran, J., Chen, L., Zhang, X., Zhang, Y.: Effects of bodyweight sup-port and guidance force on muscle activation during Locomat walking in people with stroke: a cross-sectional study. J. Neuroeng. Rehabil. 17, 1–9 (2020)CrossRef Google Scholar
- Sherman, M.F.B., Lam, T., Sheel, A.W.: Locomotor–respiratory synchronization after body weight supported treadmill training in incomplete tetraplegia: a case report. Spinal Cord 47, 896–898 (2009)CrossRef Google Scholar
- Burnfield, J.M., Buster, T.W., Goldman, A.J., Corbridge, L.M., Harper-Hanigan, K.: Partial body weight support treadmill training speed influences paretic and non-paretic leg muscle activation, stride characteristics, and ratings of perceived exertion during acute stroke rehabilitation. Hum. Mov. Sci. 47, 16–28 (2016)CrossRef Google Scholar
- van Kammen, K., et al.: The combined effects of guidance force, bodyweight support and gait speed on muscle activity during able-bodied walking in the Lokomat. Clin. Biomech. 36, 65–73 (2016)Google Scholar
- Jeong, B., Ko, C.-Y., Chang, Y., Ryu, J., Kim, G.: Comparison of segmental analysis and sacral marker methods for determining the center of mass during level and slope walking. Gait Posture 62, 333–341 (2018)CrossRef Google Scholar
- Eng, J.J., Winter, D.A.: Estimations of the horizontal displacement of the total body centre of mass: considerations during standing activities. Gait Posture 1, 141–144 (1993)CrossRef Google Scholar
- Windolf, M., Götzen, N., Morlock, M.: Systematic accuracy and precision analysis of video motion capturing systems—exemplified on the Vicon-460 system. J. Biomech. 41, 2776–2780 (2008)CrossRef Google Scholar
- Cardarelli, S., et al.: Single IMU displacement and orientation estimation of human center of mass: a magnetometer-free approach. IEEE Trans. Instrum. Meas. (2019). https://doi.org/10.1109/tim.2019.2962295CrossRef Google Scholar
- Airò Farulla, G., et al.: Vision-based pose estimation for robot-mediated hand telerehabilitation. Sensors 16, 208 (2016)CrossRef Google Scholar
- Zhi, Y.X., Lukasik, M., Li, M.H., Dolatabadi, E., Wang, R.H., Taati, B.: Automatic detection of compensation during robotic stroke rehabilitation therapy. IEEE J. Trans. Eng. Health Med. 6, 1–7 (2017)CrossRef Google Scholar
- Niu, J., Wang, X., Wang, D., Ran, L.: A novel method of human joint prediction in an occlusion scene by using low-cost motion capture technique. Sensors 20, 1119 (2020)CrossRef Google Scholar
- Manghisi, V.M., Uva, A.E., Fiorentino, M., Bevilacqua, V., Trotta, G.F., Monno, G.: Real time RULA assessment using Kinect v2 sensor. Appl. Ergon. 65, 481–491 (2017)CrossRef Google Scholar
- Cao, Z., Hidalgo, G., Simon, T., Wei, S.-E., Sheikh, Y.: OpenPose: realtime multi-person 2D pose estimation using part affinity fields. IEEE Trans. Pattern Anal. Mach. Intell. 43, 172–186 (2019)CrossRef Google Scholar
- Shaokun, S.: Detection Method and Equipment Implementation for Human Body Center of Gravity. Master (2015)Google Scholar

