Archive for May, 2022
[BLOG POST] Nutrition and Brain Injury Recovery
Posted by Kostas Pantremenos in REHABILITATION, TBI on May 31, 2022
Nutrition and Brain Injury Recovery
I am by no means a qualified dietician or nutritionist, but given the absence of guidance & support from most health specialists when it comes to nutrition and brain injury recovery, I thought it was important to share a snippet of my personal experience. If it isn’t an area that you have already explored, it might incite you to carry out some research on this topic or to seek the help of a dietician or nutritionist to get further advices.
Some of the tips shared in the following blog are from my personal trial and error in applying some of tweaks that were suggested to me and for me by a qualified dietician and nutritionist. Although there are often lots of common grounds between brain injuries, please note that a specialist may suggest a different course of action for you. Other fact to keep in mind…not all dietician and nutritionist are made equal. My first attempt in meeting a nutritionist really wasn’t successful. A year later, I explored this option again and the health professional that I met had a really sound knowledge of chronic fatigue and brain injury which lead to welcomed changes. Therefore, it you are willing to invest, it is worth asking question around their area of expertise so you can make sure that they are equipped to help you.
How can brain injury affect your gut?

Whether a person sustains a concussion, traumatic brain injury (TBI) or acquired brain injury (ABI) the brain trauma experienced tends to cause an inflammatory response. The inflammatory reaction is not isolated to the brain itself and more often than not results in structural and functional damage to the gut. The neuro trauma can increase intestinal permeability and lead to an immune response where gut inflammation and intestinal dysfunction travels back to the brain (via your central nervous system) perpetuating this cycle of inflammation. The overall inflammatory response tends to affect how your brain functions and can have a huge flow on effect on your whole body. Left untreated, symptoms such as brain fog, hormonal dysfunction, chronic fatigue, cognitive deficits, decreased physical activity and depression can sneak in making the brain injury recovery even more complex.
How did the cycle of inflammation affect me?
The reaction described above matches to the letter how my original brain injury started creating havoc in my body. In my case, encephalitis greatly affected the functioning of my nervous system. My heart rate would fluctuate in the most erratic ways, I felt constantly nauseous and I had diarrhoea just about everyday. Taken individually, these symptoms may not appear too debilitating, but when you add the daily grind of having to factor those symptoms on top of fatigue, blurry vision, sensory overload and a long list of cognitive deficits, they soon started to be one more thing that would affect my mental health. It’s as though no breaks were allowed.
When you first start to recover from a brain injury, you are very much in survival mode. At first, you tend to deal with the most obvious issues at hand and this chain of reaction is often not addressed until much later into your recovery.
Where some may be re-learning to walk, others may be dealing with fatigue, aphasia and so on. In my case, managing my levels of fatigue took priority over many of the other symptoms. At the time our sons were aged 8-7 and 4 so getting adequate sleep at night and a good rest after lunch in order to be somewhat functional once they got back from school/daycare was crucial. Other symptoms such as my fluctuating heart rate and my vision issues were also sitting at the top of the list, relaying gut health, hormonal imbalances and other ways in which I could support my overall wellbeing towards the bottom of the list.
My personal experience has also been that many mainstream health specialists look at a problem from their unique field of expertise, therefore missing out on the overall effects on the individual recovering from a brain injury. The brain does heal, but at a much slower pace than the rest of your body so supporting its recovery in any way you can from the start is key to avoid or minimise the chances of seeing this cycle of inflammation from taking over.
Nutrition tips that can support brain injury recovery?
My journey sure hasn’t been straightforward. Although information and research on the perpetuating inflammation cycle is becoming more readily accessible, it feels as though it still hasn’t become part of the mainstream information that is shared with people recovering from brain injury. I’ve found that you need to do your research, be your own advocate and keep challenging the health specialists in order to start assembling all the pieces of the complex puzzle that is brain injury recovery. Below are some of the ways in which you can support your recovering brain:
- Looking into low inflammation food and diet has initiated a much bigger shift than I ever thought possible. Cutting out or reducing the main inflammation culprits such as dairy, sugar and gluten has been really beneficial and translated in a big reduction of symptoms that I was having to factor in every day.
- Investing in my gut health has also been beneficial. Adding probiotics to my daily routine has been a simple action that has contributed to the well running of my body. My body isn’t constantly wasting time and energy in trying to recalibrate itself. Therefore more energy is available for the brain to work on healing.
- Omega-3 can help fight inflammation, maintain brain structure and have an overall positive effect on mental health so introducing fish oil with DHA & EPA is something that may be worth considering.
- In the early days of brain injury recovery, fatigue can be one of the most debilitating symptom experienced by brain injury survivors. Because fatigue can be so intense, prioritising a balanced and healthy diet isn’t always at the forefront of our minds. Therefore, introducing a good multi vitamin into your routine can be a way to help minimise nutritional deficiencies. If fatigue persists or mitochondria dysfunction sneaks into the mix, CoQ10 may be worth looking into as the Coenzyme Q10 acts on cells energy generation.
Having your hormones levels checked after brain energy is also very important. If there is an imbalance, which is fairly frequent in both women and men following brain injury, it can contribute to persisting symptoms, affect your sleep, stress response and reproductive system.
Words of advice from my personal experience
My advice to other brain injury survivors and their carers would be to seek the help and support of a qualified dietician and nutritionist to address the inflammation cycle early in the piece. It is another thing to do, but it’s a piece of the puzzle that is often overlooked. The sooner you break this cycle from taking hold, the better are your chances to avoid other secondary symptoms from creeping in. Our experience has been that not all dieticians or nutritionists have sound knowledge of diets that can best support brain injury recovery, so it is best to ask questions prior to investing and meeting with a specialist to make sure they are equipped to help you.
Where to next?
Brain injury recovery is very complex and there are so many aspects to consider. What’s important to remember is that it’s never too late to start working on pieces of the puzzle that were left untouched. You don’t know what you don’t know right, so be kind to yourself! Be open to the idea of looking into less traditional avenues and be curious about the possibilities it might bring. It could lessen some of the undesirable symptoms, perhaps get you off a plateau, translate into an increase in energy and have an overall positive effect on your physical and mental health.
Remember that you don’t have to implement everything at once. It’s ok to work on a section of the puzzle at a time and there is always time to move to the next step at a later time. I personally would much prefer to take longer to implement a strategy but make it sustainable than to rush into something that won’t last.
Nowadays there is more information available online on holistic ways to explore during brain injury recovery, but it needs to also reach the traditional systems as they are often our first port of call. Being your own advocate is crucial and it’s key to finding pieces of the puzzle that will enable you to move forward and live the best life you can following brain injury.
I am four and a half year into encephalitis recovery and I only started on this journey eight months ago after coming across a specialist that had sound knowledge of brain injury recovery. With her guidance, some of the changes implemented have been a real game changer so my advice is to keep looking and don’t give up hope.
[Abstract] Baseline Predictors of Response to Repetitive Task Practice in Chronic Stroke
Posted by Kostas Pantremenos in REHABILITATION on May 31, 2022
Abstract
Background
Repetitive task practice reduces mean upper extremity motor impairment in populations of patients with chronic stroke, but individual response is highly variable. A method to predict meaningful reduction in impairment in response to training based on biomarkers and other data collected prior to an intervention is needed to establish realistic rehabilitation goals and to effectively allocate resources.
Objectives
To identify prognostic factors and better understand the biological substrate for reductions in arm impairment in response to repetitive task practice among patients with chronic (≥6 months) post-stroke hemiparesis.
Methods
The intervention is a form of repetitive task practice using a combination of robot-assisted therapy and functional arm use in real-world tasks. Baseline measures include the Fugl-Meyer Assessment, Wolf Motor Function Test, Action Research Arm Test, Stroke Impact Scale, questionnaires on pain and expectancy, MRI, transcranial magnetic stimulation, kinematics, accelerometry, and genomic testing.
Results
Mean increase in FM-UE was 4.6 ± 1.0 SE, median 2.5. Approximately one-third of participants had a clinically meaningful response to the intervention, defined as an increase in FM ≥ 5. The selected logistic regression model had a receiver operating curve with AUC = .988 (Std Error = .011, 95% Wald confidence limits: .967–1) showed little evidence of overfitting. Six variables that predicted response represented impairment, functional, and genomic measures.
Conclusion
A simple weighted sum of 6 baseline factors can accurately predict clinically meaningful impairment reduction after outpatient intensive practice intervention in chronic stroke. Reduction of impairment may be a critical first step to functional improvement. Further validation and generalization of this model will increase its utility in clinical decision-making.
[Infographic] THIS IS YOUR BRAIN ON PIANO
Posted by Kostas Pantremenos in Educational on May 31, 2022

[BLOG POST] Measuring the Severity of a Stroke
Posted by Kostas Pantremenos in REHABILITATION on May 26, 2022
How Stroke Severity Is Measured
BY MARK SCHMIDT

A stroke can impact a senior’s emotional, physical, and cognitive abilities for the rest of his or her life. If your aging loved one has experienced a stroke, an assessment can be used to evaluate his or her abilities, determine the best possible treatment, and predict future outcomes.
Strokes are just one of the many serious health issues older adults are susceptible to. If your senior loved one has been diagnosed with a serious condition and needs help with tasks like meal prep, transportation, bathing, and grooming, reach out to Home Care Assistance, a leading provider of homecare services families can trust. We also offer comprehensive care for seniors with dementia, Alzheimer’s, and Parkinson’s.
Here’s some important information about assessing the severity of strokes.
Understanding The NIH Stroke Scale
The National Institutes of Health Stroke Scale (NIHSS) is the most widely used tool for evaluating the neurological status of stroke survivors, and it can not only predict brain lesion size but also measure stroke severity. This scale can also predict your loved one’s short-term and long-term outcomes.
The stroke scale analyzes many aspects, including horizontal eye movements, facial palsy, arm and leg movement, language abilities, sensation, and the ability to answer questions. These individual scores are used to calculate the NIHSS score, which ranges from 0 (no stroke symptoms) to 21–42 (severe stroke).
This test is an excellent predictor of outcome. Someone who has a baseline score of less than 6 has a very good chance of recovery. Keep in mind current stroke scales that measure impairment only partially explain the impact on the person’s disability and quality of life. Some people adapt better to the impairments of a stroke, while some people with minimal neurological impairment may be severely disabled after a stroke.
Most stroke survivors can live at home safely with the help of family members and professional caregivers. Many seniors prefer aging in place over moving to assisted living facilities. If your senior loved one needs assistance to remain safe and comfortable while living at home, reach out to Home Care Assistance, a leading Tucson senior home care agency. Our dedicated in-home caregivers can assist with meal prep, bathing and grooming, exercise, medication reminders, and many other important tasks.
A Better Stroke Outcome
While the severity of stroke plays a big role in outcome, early rehabilitation can also help your loved one recover better following a stroke. An in-home caregiver can also provide assistance with daily activities, encourage healthy recovery habits, and assist with personal care, medication reminders, transportation, and more.
Because every stroke is different in terms of the areas of the brain it affects and the deficits that occur, every recovery is different. Try to avoid making comparisons with another stroke survivor and have your loved one’s progress measured to determine how much rehabilitation should be provided.
Recovering from a stroke, managing the symptoms of Alzheimer’s, and a variety of other health-related situations can make it difficult for a senior to continue living at home without someone there to help. Tucson, AZ, live-in care professionals are trained to help seniors who need 24/7 assistance. With the help of a live-in caregiver, your elderly loved one can maintain a higher quality of life while aging in place. Trust your loved one’s care to the professionals at Home Care Assistance. Reach out to one of our compassionate Care Managers today at (520) 214-6779.
Related Posts:
[Abstract] The TWIST Tool Predicts When Patients Will Recover Independent Walking After Stroke: An Observational Study
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop on May 24, 2022
Abstract
Background
The likelihood of regaining independent walking after stroke influences rehabilitation and hospital discharge planning.
Objective
This study aimed to develop and internally validate a tool to predict whether and when a patient will walk independently in the first 6 months post-stroke.
Methods
Adults with stroke were recruited if they had new lower limb weakness and were unable to walk independently. Clinical assessments were completed one week post-stroke. The primary outcome was time post-stroke by which independent walking (Functional Ambulation Category score ≥ 4) was achieved. Cox hazard regression identified predictors for achieving independent walking by 4, 6, 9, 16, or 26 weeks post-stroke. The cut-off and weighting for each predictor was determined using β-coefficients. Predictors were assigned a score and summed for a final TWIST score. The probability of achieving independent walking at each time point for each TWIST score was calculated.
Results
We included 93 participants (36 women, median age 71 years). Age < 80 years, knee extension strength Medical Research Council grade ≥ 3/5, and Berg Balance Test < 6, 6 to 15, or ≥ 16/56, predicted independent walking and were combined to form the TWIST prediction tool. The TWIST prediction tool was at least 83% accurate for all time points.
Conclusions
The TWIST tool combines routine bedside tests at one week post-stroke to accurately predict the probability of an individual patient achieving independent walking by 4, 6, 9, 16, or 26 weeks post-stroke. If externally validated, the TWIST prediction tool may benefit patients and clinicians by informing rehabilitation decisions and discharge planning.
[WEB] Generalized and Focal Epilepsy Interaction
Posted by Kostas Pantremenos in Epilepsy on May 24, 2022
Article written by Brooke Dulka, Ph.D.

Traditionally, focal and generalized epilepsy are classified as distinct types of seizure disorders. However, generalized epilepsy and focal epilepsy can overlap, and this interaction can blur the line between the two disorders. This makes diagnosis challenging for people experiencing these types of episodes. What is the difference between these two seizure types? How do they interact? Finally, why does this interaction occur?
Generalized Epilepsy vs. Focal Epilepsy
The types of seizures that define focal and generalized epilepsy are focal or generalized seizures.
Focal Seizures
Focal seizures start in a single area of the brain (on one side). They can involve movement or lack of movement. A person may remain aware during these episodes or may lose awareness.
Generalized Seizures
Generalized seizures start in both halves of the brain (hemispheres) at the same time. These are tonic-clonic seizures. A person loses awareness during generalized seizures. This category includes absence seizures.
Therefore, the primary difference between generalized epilepsy and focal epilepsy is how and where seizure activity starts. Specialists used this principle to reclassify seizure disorders in 2017 to give them more accurate names and stress the importance of the seizure’s origin.
Focal to Generalized and Generalized to Focal Evolution
If a focal seizure spreads to involve a large enough area (or enough nodes) of the brain, it can turn into a generalized seizure. This is different from a primary generalized seizure, which starts on both sides of the brain at once.
The evolution of a focal seizure to a generalized seizure can happen very quickly, often taking only seconds. The person may initially experience a sudden uncontrollable movement or change in sensation like smell. They may be confused. The person may then progress into a classic tonic-clonic seizure, with loss of consciousness, jerking uncontrollable movements, and loss of bowel and bladder control. After the seizure finishes, the person may experience a period of confusion, drowsiness, change in mood, headache, and nausea.
The reverse is also possible. Research has shown that someone can have seizures that have a generalized onset but then evolve into a focal seizure. This has been proven clinically and also shown on electroencephalogram (EEG) testing, which measures brain waves.
It is also becoming more widely known that focal seizures can occur in cases of idiopathic generalized epilepsy. This group of disorders includes generalized seizure disorders of unknown causes that are thought to be largely driven by genetic factors. Unfortunately, the presence of focal seizures in idiopathic generalized epilepsy often leads doctors to misdiagnose it as focal epilepsy. Recently, people have also argued to classify generalized onset seizures with focal evolution as a unique seizure type.
Someone can have both types of seizures one after the other, and this can present a diagnostic dilemma.
Implications of the Interaction Between Generalized and Focal Epilepsy
The interaction between focal seizures and generalized seizures creates a problem because it complicates the diagnostic process. Not only does this interaction often lead to misdiagnosis, but it lengthens the time until the most appropriate treatment methods can start.
When treating seizure disorder, one of the first considerations is the type of seizure the person has. This will help dictate which medication is used. Broad-spectrum anticonvulsants are typically used first and for generalized seizures. Narrow-spectrum anticonvulsants are normally used for the treatment of partial seizures.
The identification of the correct seizure type in an individual will help neurologists avoid narrow-spectrum drugs that can worsen generalized seizures. This can also help people avoid some negative side effects of anticonvulsants, by ensuring they receive the right drugs earlier in their treatment process.
Finding Help for Epilepsy
MyEpilepsyTeam is the social network for people with epilepsy and their loved ones. On MyEpilepsyTeam, more than 100,000 members come together to ask questions, give advice, and share their stories with others who understand life with epilepsy.
Do you experience generalized or focal seizures? Share your experience in the comments below, or start a conversation by posting on MyEpilepsyTeam.
[WEB] Gait & Balance – Product Guide 2022 – Physical Therapy Products
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop on May 24, 2022
Posted by Deborah Overman

Even the youngest Baby Boomers are now rapidly approaching the age of 65. Since, statistically, fall risk increases as adults age, physical therapists will be increasingly needed to help this population avoid falls and restore gait patterns through the use of gait & balance products, including those engineered with advanced features for trending and analyzing data.

BITS
The Bioness Integrated Therapy System (BITS), from Bioness Inc, Valencia, Calif, aims to challenge and assess visual, cognitive, motor, and balance abilities of individuals, including those with deficits resulting from traumatic injuries and movement disorders. The third generation includes BITS Balance, in which proprietary motion sensors track patients’ movements and a balance platform challenges weight shift. Over 60 software programs allow clinicians to challenge, assess, and track patient progress throughout treatment. Across industries, therapists use BITS and BITS Balance to train patients with varying degrees of mobility, driving patient outcomes.
For more information, contact Bioness Inc, (855) 902-5252; www.bionesstherapy.com

ZENO ELECTRONIC WALKWAY SYSTEM
Managing and synthesizing accurate gait data is essential to outcomes-driven healthcare. The portable Zeno Walkway from ProtoKinetics, Havertown, Pa, has a wide, flat surface that allows for the capture of loading patterns of the patients’ footsteps without any impedance to assistive device performance. PKMAS software identifies typical footfall patterns instantly and is engineered to automatically eliminate walker tracks, while expertly identifying overlapping steps, to provide robust temporal-spatial measurements for even the most complicated gait patterns. Recent implementation of the enhanced Gait Variability Index (eGVI), instrumented Four Square Step Test (iFSST), and Limits of Stability (LoS) balance test are examples of rehabilitation-related outcome measures which can assist in clinical treatment planning and hospital discharge decisions.
For more information, contact ProtoKinetics, (610) 449-4879; www.protokinetics.com

INSTRUMENTED TRAINING TREADMILL
C-Mill is an advanced, instrumented treadmill with force plates and real-time feedback for the objective, in-depth assessment and training of impaired gait and balance in a visual, immersive environment. After measuring and analyzing a patient’s unique walking pattern, the C-Mill provides a safe environment that therapists can tailor to their patients’ abilities using dozens of fun and challenging visual and auditory cues. The patients are cognizant of their movements through immediate feedback projected on the treadmill, auditory feedback, video recordings, and clear reports. With the body weight support option, patients can benefit from the C-Mill therapy very early on. DIH therapy solutions support the treatment of patients across the continuum of care.
For more information, contact DIH, (877) 944-2200; www.dih.com or https://www.motekmedical.com/solution/c-mill or info.us@dih.com

PRESSURE MAPPING SYSTEM
The BodiTrak BioMetrics Pressure Mapping System from BodiTrak BioMetrics, a Vista Medical company, is designed to provide objective, real-time data and performance metrics to help aid clinical decision-making. Assess, retrain, and evaluate patients while enhancing engagement. Gain a better picture of symmetry, weight shift, compensations, balance and more for analysis, treatment progression, and return to function.
For more information, contact BodiTrak BioMetrics by Vista Medical; (855) 733-0123, ext 104; www.boditrakbiometrics.com

BALANCE SYSTEM
The Biodex Balance System SD, from Biodex Medical Systems Inc, Shirley, NY, is a versatile balance testing and training device that adds value with turnkey programs to help therapists grow their businesses. Access science-based technology solutions, from fall risk to concussion management. Objective data and reporting help meet requirements for value-based care.
For more information, contact Biodex, (800) 224-6339; www.biodex.com/balance or sales@biodex.com

IN-SHOE GAIT ANALYSIS SYSTEM
The F-Scan64 wireless in-shoe pressure measurement system from Tekscan, South Boston, offers quick set-up and flexibility to collect pressure, force, and temporal gait parameters. Featuring small and lightweight data acquisition electronics, F-Scan64 is designed to allow a natural gait-collection environment free from cords and excessive weight or bulk for patients. The combination of a simple set-up process and gait analysis software essentials helps clinicians save time when working with patients, without sacrificing data quality or reporting capabilities.
For more information, contact Tekscan, (800) 248-3669; www.tekscan.com
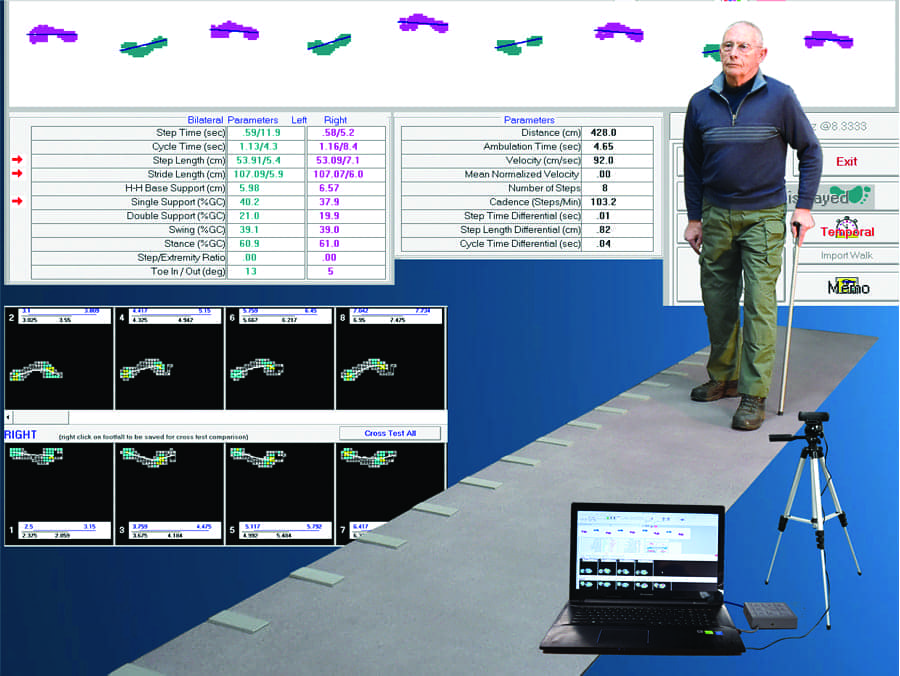
PORTABLE GAIT ANALYSIS
GAITRite from CIR Systems Inc, Franklin, NJ, is truly a portable pressure sensitive walkway in a single rollout with a quick and easy setup, under 2 minutes, measuring temporal spatial parameters, providing easy identification of gait anomalies. It is available in a variety of lengths, from 14 feet to 26 feet. GAITRite software records and analyzes multiple gait cycles in a single walk, allowing for accurate testing of patients with or without shoes, assistive devices, and ambulatory aids—crutches, walkers, or canes. GAITRite provides robust reporting and web publishing options to document current conditions and track recovery/rehabilitation. The application software controls the functionality of the walkway, processes the raw data into footfall patterns, and computes the temporal (timing) and spatial (distance) parameters. The software’s relational database stores tests individually under each patient and supports a variety of reports and analyses.
For more information, contact CIR Systems Inc, (888) 482-2362; www.gaitrite.com

FALL AND FRACTURE REDUCTION PROGRAM
Medical Fitness Solutions, Fallbrook, Calif, offers products that aim to provide a drug-free method of reducing falls and fractures. By addressing each component of a fall and fracture—strength, bone density, balance, and gait—the MFS fall and fracture reduction program should reduce falls, and severity of injury.
For more information, contact Medical Fitness Solutions, (800) 831-7665; www.medicalfitsolutions.com

EYE MOVEMENT ANALYSIS SYSTEM
VisualEyes 505 from Interacoustics, Eden Prairie, Minn, is a powerful eye movement analysis system designed to simultaneously record eye and patient movements as a tool for clinicians specializing in vestibular physical therapy. The video Frenzel system features a spontaneous nystagmus detection algorithm designed to provide objective slow phase velocity data for clinically accurate reports. PC-based, VisualEyes 505 is offered in a variety of video goggle sizes and configurations, including a headband option, and is available in either a monocular or binocular camera configuration. Modules that add a 3D head model to help therapists position patients, as well as a torsional nystagmus upgrade for improved accuracy in BPPV assessment, are available.
For more information, contact Interacoustics, (800) 947-6334; www.interacoustics.com/us

MOTOR-COGNITIVE TRAINING
By adding virtual reality experience to existing treadmills, GaitBetter could enable a personalized, safe, and effective motor-cognitive intervention for gait rehabilitation and falls prevention. GaitBetter was designed by leading researchers, scientists, and technologists to maximize therapy outcomes such as dynamic balance, gait speed, obstacles negotiation, decision-making, and motor-planning. The system was featured in a multi-center, randomized controlled trial in virtual reality for rehabilitation, published in The Lancet. Gamified exercise could help increase patients’ adherence and reduce no-shows. The system is operated by PTAs and PT techs, utilizes existing equipment, and features a flexible pricing model.
For more information, contact GaitBetter, (908) 883-3218; www.gaitbetter.com

BALANCE BOARD KIT
Calgary, Alberta, Canada-based Fitter International Inc offers the Fitterfirst Balance Board Kit. The company’s tri-level, 3/4-inch Baltic birch boards are great for clinics, clubs, and studio use. Each kit includes three boards and a durable stand that can hold up to five boards. The 20-inch Pro Rocker Board is a beginner board that provides a single plane of motion at 10-degree, 12-degree, and 15-degree angles. The 20-inch Pro Balance Board is an intermediate multi-directional round board that provides 10-degree, 12-degree, and 15-degree angles. The 16-inch Pro Balance Board is an advanced multi-directional round board that provides 15-degree 17-degree, and 20-degree angles. A 5-board kit complete with stand is also available.
For more information, contact Fitter International Inc, (800) fitter-1 (348-8371); www.fitter1.com
Related Content:
Product Guide 2021: Gait & Balance
[Abstract] Surface Electromyography-Driven Therapeutic Gaming for Rehabilitation of Upper Extremity Weakness: A Pilot Study
Posted by Kostas Pantremenos in Paretic Hand, Video Games/Exergames on May 24, 2022
Abstract
Summary:
In patients with severe upper extremity weakness that may result from peripheral nerve injuries, stroke, and spinal cord injuries, standard therapy in the earliest stages of recovery consists primarily of passive rather than active exercises. Adherence to prescribed therapy may be poor, which may contribute to suboptimal functional outcomes. The authors have developed and integrated a custom surface electromyography device with a video game to create an interactive, biofeedback-based therapeutic gaming platform. Sensitivity of the authors’ custom surface electromyography device was evaluated with simultaneous needle electromyography recordings. Testing of this therapeutic gaming platform was conducted with a single 30-minute gameplay session in 19 patients with a history of peripheral nerve injury, stroke, spinal cord injury, and direct upper extremity trauma, including 11 patients who had undergone nerve and/or tendon transfers. The device was highly sensitive in detecting low levels of voluntary muscle activation and was used with 10 distinct muscles of the arm, forearm, and hand. Nerve and tendon transfer patients successfully activated the donor nerve/muscle and elicited the desired movement to engage in gameplay. On surveys of acceptability and usability, patients felt the system was enjoyable, motivating, fun, and easy to use, and their hand therapists expressed similar enthusiasm. Surface electromyography-based therapeutic gaming is a promising approach to rehabilitation that warrants further development and investigation to examine its potential efficacy, not only for building muscle strength and endurance but also for facilitating motor relearning after nerve and tendon transfer surgical procedures.


