Posts Tagged home-based rehabilitation
[ARTICLE] Use of the Digital Assistant Vigo in the Home Environment for Stroke Recovery: Focus Group Discussion With Specialists Working in Neurorehabilitation – Full Text
Posted by Kostas Pantremenos in Apps, Artificial intelligence, Assistive Technology, Tele/Home Rehabilitation on April 22, 2023
Abstract
Background:There is a lack of resources for the provision of adequate rehabilitation after a stroke, thus creating a challenge to provide the necessary high-quality, patient-centered, and cost-efficient rehabilitation services at a time when they are needed the most. Tablet-based therapeutic programs present an alternative way to access rehabilitation services and show a new paradigm for providing therapeutic interventions following a stroke anytime and anywhere. The digital assistant Vigo is an artificial intelligence–based app that provides an opportunity for a new, more integrative way of carrying out a home-based rehabilitation program. Considering the complexity of the stroke recovery process, factors such as a suitable population, appropriate timing, setting, and the necessary patient-specialist support structure need to be thoroughly researched. There is a lack of qualitative research exploring the perspectives of professionals working in neurorehabilitation of the content and usability of the digital tool for the recovery of patients after a stroke.
Objective:The aim of this study is to identify the requirements for a tablet-based home rehabilitation program for stroke recovery from the perspective of a specialist working in stroke rehabilitation.
Methods:The focus group study method was chosen to explore specialists’ attitudes, experience, and expectations related to the use of the digital assistant Vigo as a home-based rehabilitation program for stroke recovery in domains of the app’s functionality, compliance, usability, and content.
Results:In total, 3 focus groups were conducted with a participant count of 5-6 per group and the duration of the discussion ranging from 70 to 80 minutes. In total, 17 health care professionals participated in the focus group discussions. The participants represented physiotherapists (n=7, 41.2%), occupational therapists (n=7, 41.2%), speech and language therapists (n=2, 11.8%), and physical medicine and rehabilitation physicians (n=1, 5.9%). Audio and video recordings of each discussion were created for further transcription and analysis. In total, 4 themes were identified: (1) the clinician’s views on using Vigo as a home-based rehabilitation system, (2) patient-related circumstances facilitating and limiting the use of Vigo; (3) Vigo’s functionality and use process (program creation, individual use, remote support); and (4) complementary and alternative Vigo use perspectives. The last 3 themes were divided further into 10 subthemes, and 2 subthemes had 2 sub-subthemes each.
Conclusions:Health care professionals expressed a positive attitude toward the usability of the Vigo app. It is important that the content and use of the app be coherent with the aim to avoid (1) misunderstanding its practical use and the need for integration in practice and (2) misusing the app. In all focus groups, the importance of close involvement of rehabilitation specialists in the process of app development and research was highlighted.
Introduction
During 2019, in Latvia, 5838 people were hospitalized because of a stroke [1]. More than 80% of these admissions were in stroke units, creating a heavy burden on specialists working in acute stroke care [1,2]. Unfortunately, there is a shortage of rehabilitation providers and a lack of resources for the provision of adequate rehabilitation after a stroke [2–4]. Thus, professionals and organizations are challenged to provide the necessary high-quality, patient-centered, and cost-efficient rehabilitation services at a time when they are needed the most. Increased pressure on hospitals and inpatient centers shows that new rehabilitation approaches need to be considered outside the hospital setting [5,6].
Home-based rehabilitation has the benefit of treating clients in a familiar environment, which stimulates mental and physical activity and prevents problems with transferring learned skills to their daily lives [4]. Research shows that home-based interventions can provide more cost-efficient services [7,8]. In recent years, the use of information and communication technologies (ICT) has been a research area of interest due to its potential to improve the efficiency, quality, and availability of rehabilitation care [9,10]. Tablet-based therapeutic programs present an alternative way to access rehabilitation services anytime and everywhere through the internet and technology under remote guidance of the therapist [11–13]. Tablet-based rehabilitation programs show a new paradigm for providing therapeutic interventions following a stroke [14]. Considering the complexity of the stroke recovery process, factors such as a suitable population, appropriate timing, setting, and the necessary patient-specialist support structure need to be thoroughly researched [15,16]. Research shows that personalized apps could give health professionals a better overview of patients’ rehabilitation process and provide follow-up after the patients are discharged from the inpatient rehabilitation center or stroke unit, with the condition that the apps would contain information about patients’ health status and functional impairment and the content would support the person-centered rehabilitation process [17,18].
At the time of discharge from the hospital or inpatient rehabilitation center, approximately 74% of physical and occupational therapists hand out a written home program. Even though written recommendations are a widely used approach for continuing rehabilitation at home, they lack 2 key components, adherence and feedback [14,19]. The digital assistant Vigo provides an opportunity for a new, more integrative way of carrying out a home-based rehabilitation program compared to traditional written recommendations. Previous research shows that patients have a positive attitude toward the use of the digital assistant Vigo as a tool for therapeutic home-based programs [20]. To integrate the digital assistant into practice, it is of upmost importance to research the use of the program, not only from a patient perspective, but also from the perspective of health care professionals working in neurorehabilitation. The aim of this study is to identify the requirements for a tablet-based home rehabilitation program for stroke recovery from the perspective of a specialist working in stroke rehabilitation.[…]
[BLOG POST] Home-based virtual-reality training improves functional recovery in chronic stroke and induces cortical reorganization
Posted by Kostas Pantremenos in Paretic Hand, Rehabilitation robotics, Tele/Home Rehabilitation, Virtual reality rehabilitation on January 31, 2023
1 Community-based and home-based rehabilitation – essential tools in chronic stroke
2 Robotic devices and virtual reality training in community and home-based rehabilitation
3 VR training for home-based rehabilitation in stroke patients
4 Benefits of VR training on motor recovery of upper limb function during home-based rehabilitation
5 VR training induces brain neuroplastic changes in stroke patients
Community-based and home-based rehabilitation – essential tools in chronic stroke
Can home-based virtual-reality training improves functional recovery in chronic stroke and induces cortical reorganization? Disability is a dramatic consequence of stroke, affecting 50% of survivors, while 30% lose their autonomy and depend on others for daily activities [1]. Rehabilitation is one of the most critical interventions in stroke, and there is evidence that it has benefits in all stroke stages. In the acute stage (first 3 weeks after stroke), rehabilitation is initiated in the stroke unit and continued during hospitalization. In the subacute stage (between 3 weeks and 6 months after the event), stroke severity and predicted outcome would guide the level of care: inpatient rehabilitation facilities or skilled nursing facilities. Despite intensive interventions, 25 to 75% of stroke patients are discharged with significant physical and functional limitations [2].
For more information on stroke, check out:
- Recovery of precise hand movements after stroke
- Motor function after stroke is promoted by early neural network reorganization
To get more insightful perspectives on neurology, watch:
- Interview with Dr. Dana Boering (EFNR Secretary General)
- Interview with Prof. Raad Shakir (Past President WFN)
In chronic stroke stages (after 6 months), rehabilitation training is still beneficial and should be provided in community-based facilities or at home with supervision. There is evidence that physical training is effective in chronic stroke, increasing quality of life and leading to cardiovascular benefits, and should be promoted by community programs. A physically active lifestyle should be encouraged by community and domiciliary interventions. Without constant participation in training programs, a decline in motor and functional acquisition is noticed in stroke patients, and gains obtained by previous inpatient interventions could be lost [2–3].
Robotic devices and virtual reality training in community and home-based rehabilitation
The major challenge for rehabilitation in stroke patients after discharge at home is the successful transition to the community, including an ongoing rehabilitation program. The barriers could be the limited availability of therapists and the distance to the rehabilitation center in the community. This may delay the training schedules and increase patient and caregiver dissatisfaction. One of the latest approaches in stroke rehabilitation is technology-assisted rehabilitation (TAR). TAR has the advantage of providing remote training for patients, adapted to each patient’s needs. Stroke patients could be able to frequently train with minimal therapist supervision and would be provided with constant feedback. TAR includes robotic training systems, virtual reality, and sensor-based training systems.
Previous evidence showed that Virtual Reality (VR) interventions are acceptable and effective in evaluating stroke patients and rehabilitation [4–6]. VR combines devices with specific interfaces with automated training sequences, delivering personalized rehabilitation to patients. One example of VR technology is the Rehabilitation Gaming System (RGS) which is effective in the upper limb rehabilitation of acute and chronic stroke patients [7].
VR training for home-based rehabilitation in stroke patients
A study by Ballester et al. aimed to assess the efficacy and limitations of home VR-based training in stroke patients compared to domiciliary occupational therapy. The authors focused on functional recovery of upper limb motility and cortical network reorganization after treatment [2].
The study, set in Barcelona in 2017, included 39 patients after a first stroke, at more than 12 months from stroke onset (in the late-chronic phase), with mild-to-moderate upper limb (UL) motor deficits (score >2 in proximal UL on the Medical Research Council MRC scale) and without significant cognitive impairment. The patients were familiar with the RGS device previously used during inpatient rehabilitation. Twenty patients were included in the RGS group, and 19 patients were in the control group. The control group received at-home occupational therapy, while the subjects were in the RGS group.
The Rehabilitation Gaming System (RGS) uses an image capture device and allows the patient to control on the screen a virtual body part (like a hand and arm avatar) while performing different tasks. The system is shown in Figure 1.

Figure 1. The Rehabilitation Gaming System. A: PC with a vision-based motion tracking device. The patient is wearing data gloves. The system captures the movements of the patient’s joint and transforms them into an avatar shown on the screen, miming the user’s actions. B: The avatar movements from the patient’s perspective are displayed on the screen. The task is to catch the colored objects moving with different trajectories and speeds. C: Protocol of evaluation at inclusion (W0), at 3 weeks (W3), and at 12 weeks (W12). RGS = Rehabilitation Gaming System; OT = Occupational Therapy; AEMF = Automated Evaluation of Motor Function; NBS = Navigated Brain Stimulation. (From Ballester et al. [2])
The tasks and the movements trained by the system are shown in Table 1.

Table 1. Task-oriented movements provided by RGS system during upper-limb training
The game parameters are modulated after each task completion and adapted to maintain a performance ratio between 60% and 80% to motivate the patient and provide an optimal challenge for each training session. The RGS system also includes software for the automated evaluation of a patient’s motor performance during training, called AEMF (Automated Evaluation of Motor Function), designed to assess UL motor function without therapist intervention [2]. The AEMF scenario is split into two tasks to evaluate proximal and distal motor function. In the first task, participants had to use planar wiping motions with their arms to remove small cubes from a virtual surface. In task 2, participants were told to flex and stretch their fingers to squeeze a virtual object. These AEMF activities were performed first with the non-paretic limb and subsequently with the paretic limb to ensure that the AEMF tasks were correctly understood. Participants did not receive any direct feedback about their performance. During task execution, the software collected data on hand position and joint rotation (fingers, elbows, and shoulders) to determine the horizontal planar area covered, finger flexion, and finger extension [2].
The study intervention provided subjects with daily sessions of home training with the RGS system, 20-60 minutes/session, 5 days/week, for 3 weeks. Each session consisted of subtasks on the upper limbs’ – hitting, grasping, and placing movements. The control group was performing individual OT at home for the same duration. The expectation was that all participants perform between 1-3 training sessions a day.
At the end of the intervention, all participants could use the gloves and set the VR training system without assistance. Moreover, the authors highlight the significant increase in task difficulty during training, reflecting better performance in both paretic and non-paretic limbs [2].
Benefits of VR training on motor recovery of upper limb function during home-based rehabilitation
In the study conducted by Ballester et al., the authors measured the motor function of the affected upper limb using standard clinical scales [2] presented in Figure 2 below:
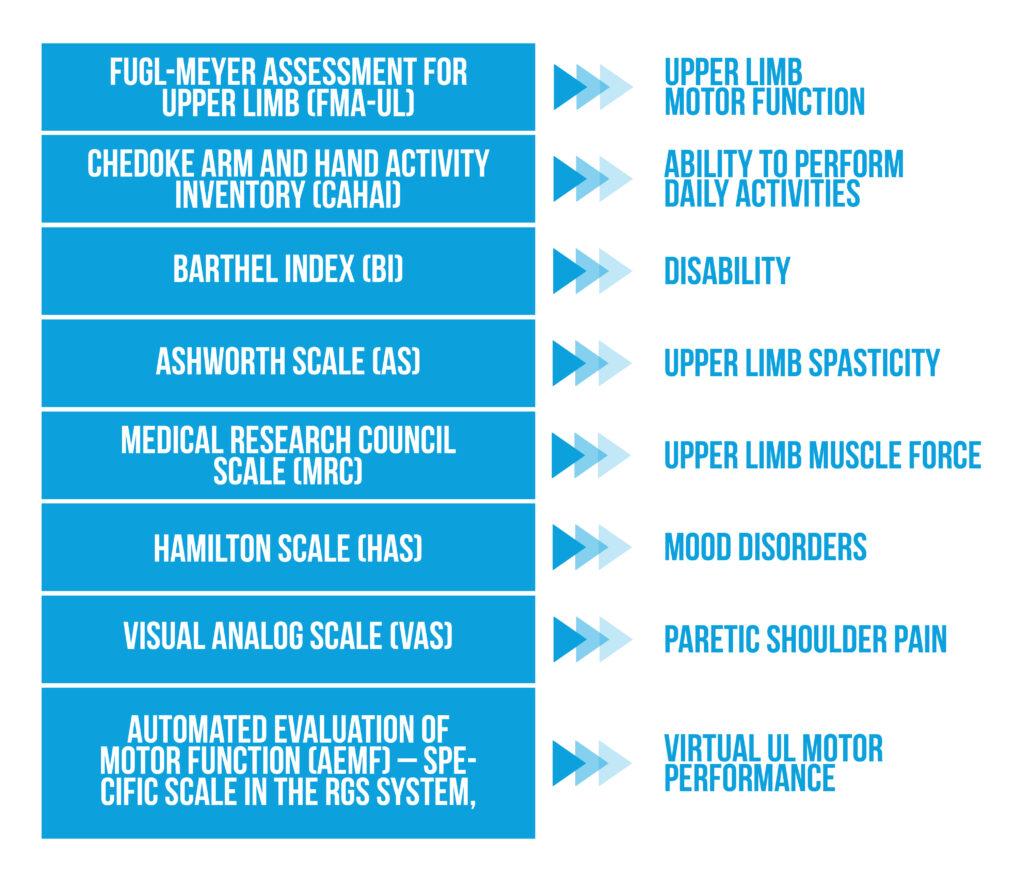
Figure 2. Clinical Scales
The measurements were performed at inclusion, after 3 weeks of intervention, and at 3-month follow-up. The originality of this study was developing a biomechanical model of the paretic upper limb using captured movements by data gloves and by the screen motion capture device.
No proximal and distal paretic UL motor function improvements were noticed on FMA-UL and MRC scales. Distal upper limb spasticity improved significantly 3 months after VR training (measured on AS). At the end of the intervention, the RGS group showed significantly better upper limb ability in performing daily activities (measured by the CAHAI scale), an effect that was not persistent at follow-up.
The authors pinpoint as an essential finding the detection of functional improvements in the distal part of the paretic upper limb after completing 2 or 3 weeks of VR home training. Repetitive tasks involving reaching and grasping hand movements increase the range of finger flexion and extension. This motor gain in the distal UL function was demonstrated using data collected by the AMEF system, which is another strong point in this study [2].
Looking at these results holistically, the authors noted as a limit to their research, that task difficulty descriptors, AEMF measurements, and NBS all converged, indicating that distal functional improvements were introduced through RGS-based training and were significantly greater for participants in the RGS group when compared to the control group. Furthermore, they also noted that the observed inter-group variabilities were due to the two different interventions applied [2].
VR training induces brain neuroplastic changes in stroke patients
The authors aimed to demonstrate that VR training could induce cortical reorganization in stroke patients. Navigated Brain Stimulation (NBS) procedures were used to demonstrate corticospinal tract integrity and to evaluate the motor map in the primary cortical motor area. The authors used the evaluation of the cortical representation of two hand muscles usually affected by stroke: abductor policis brevis (APB) and extensor-carpi radialis (ECR). The NBS procedure is shown in Figure 3.
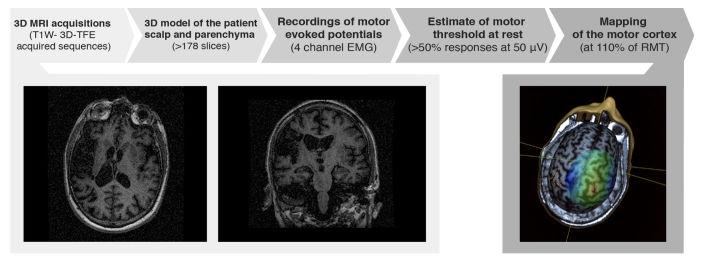
Figure 3. Navigated Brain Stimulation (NBS) procedure for brain mapping (from Ballester et al. [2])
The procedure implied a 3-Tesla MRI examination of the patient. A 3-dimensional model is provided for the skull and brain parenchyma. Recording of motor-evoked potentials (MEPs) was performed using transcranial magnetic stimulation (TMS) connected to an electromyographic (EMG) system. The motor threshold at rest (RMT) for both APB and ECR muscles was estimated, and the cortical maps were drawn in both cerebral hemispheres. Corticospinal connectivity was assessed by estimation of the center of origin of the motor fibers in the cortical area. The stimulation efficacy (SE) of each map region was estimated. Both normal and affected hemispheres were evaluated.
In this study, brain maps of 17 stroke patients were assessed using NBS procedures before and after VR training. The cortical areas representing ABP and ECR muscles were detected on the cortical map. Stimulation efficacy was recorded, and the center of the cortical area which produces MEPs was drawn in both cerebral hemispheres before and after 3 weeks of treatment.
The results showed enhanced excitability in the corticospinal tracts of the affected hemisphere after completing VR training. SE increases in the pathological cortical motor areas after the intervention. Moreover, changes in cortical connectivity were demonstrated by the displacement of the center of the cortical motor area, producing MEPs for both ABP and ECR muscles after the intervention. The authors postulated that these cortical organization changes correlate with the motor gains captured by the clinical scales [2].
Ballister and collab. highlight that the measurement of corticospinal connectivity using the NBS procedure could be used as a biomarker for detecting chronic stroke patients who will respond to rehabilitation treatment [2].
Conclusions
In chronic stroke patients, no motor improvements are expected, and the efficacy of rehabilitation treatments in this phase is still debated. Patients are discharged into the community with limited rehabilitation programs or therapist access. This study conducted by Ballester shows that rehabilitation using new technologies, such as Virtual Reality, is feasible at home without specialist supervision and is accepted by most patients. The Rehabilitation Gaming System (RGS) uses a goal-oriented approach in which the patient tries to control the avatar of its paretic and non-paretic upper limbs while executing complex motor tasks (such as catching moving balls on the screen). RGS parameters are automatically adapted to maintain the game challenge. At the end of the training period, patients were able to perform more difficult tasks, reflecting better performance in both paretic and non-paretic limbs.
This study demonstrates that VR training for 3 weeks induces improvements in motor function of the distal paretic upper limb in chronic stroke patients. Functional gains were obtained for finger flexion and extension movements. These data were obtained using the Automated Evaluation of Motor Function, included in the RGS system. Moreover, VR training decreased spasticity in the distal upper limb. The authors highlight the significant improvements observed in paretic hand abilities during daily activities after 3 weeks of training.
Ballester et al. [2] used brain imaging and neurophysiological methods to demonstrate that VR-based motor training enhanced the excitability of some corticospinal fibers controlling hand function Neuroplastic changes obtained after training reveal that cortical reorganization could be induced in the chronic stage post-stroke by technology-assisted rehabilitation methods, like virtual reality.
Bibliography
- Markus HS. Reducing disability after stroke. International Journal of Stroke. 2022;17(3):249-250. doi:10.1177/17474930221080904
- Ballester BR, Nirme J, Camacho I, Duarte E et al., Domiciliary VR-Based Therapy for Functional Recovery and Cortical Reorganization: Randomized Controlled Trial in Participants at the Chronic Stage Post Stroke. JMIR Serious Games. 2017 Aug 7;5(3):e15. doi: 10.2196/games.6773.
- Winstein CJ, Stein J, Arena R, Bates B et al., American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Quality of Care and Outcomes Research. Guidelines for Adult Stroke Rehabilitation and Recovery: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2016;47(6):e98-e169. doi: 10.1161/STR.0000000000000098.
- Cameirão MS, Badia SB, Duarte E, Frisoli A, Verschure PF. The combined impact of virtual reality neurorehabilitation and its interfaces on upper extremity functional recovery in patients with chronic stroke. Stroke. 2012 Oct;43(10):2720–8. doi: 10.1161/STROKEAHA.112.653196.
- McEwen D, Taillon-Hobson A, Bilodeau M, Sveistrup H, Finestone H. Virtual reality exercise improves mobility after stroke: an inpatient randomized controlled trial. Stroke. 2014 Jun;45(6):1853–5. doi: 10.1161/STROKEAHA.114.005362
- Rizzo A. Virtual reality and disability: emergence and challenge. Disabil Rehabil. 2009;24(11-12):567–9. doi: 10.1080/09638280110111315
- Ballester BR, Maier M, Duff A, Cameirão M et al., A critical time window for recovery extends beyond one-year post-stroke. J Neurophysiol. 2019;122(1):350-357. doi: 10.1152/jn.00762.2018.
[ARTICLE] Relationship between Activities of Daily Living of Home-Based Rehabilitation Users and Caregiver Burden-Induced Depression: A Retrospective Study – Full Text
Posted by Kostas Pantremenos in Caregivers, Depression, Tele/Home Rehabilitation on June 22, 2022
Abstract
This study was aimed at determining the cutoff values of activities of daily living (ADL) and the combination of related factors associated with high caregiver burden that induces depression among caregivers. The study participants included 50 pairs of home-based rehabilitation users and their primary caregivers. They were classified into two groups: high-burden and low-burden groups according to the short version of the Japanese version of the Zarit Caregiver Burden Interview score of ≥13 or ≤12, respectively. The cutoff values of ADL and the combination of related factors associated with high caregiver burden were examined using the receiver operating characteristic curve and decision tree analyses. The cutoff value associated with high caregiver burden was 5 points for the controlling bladder item of the Barthel index (BI) (sensitivity: 90%, specificity: 70%). Regarding the decision tree, the controlling bladder item of BI (≤5 or 10 points) was selected as the first layer and the recipient’s age (≤78 or ≥79 years) as the second layer. High caregiver burden was identified in 85.7% of the caregivers in whom the score of controlling bladder of BI was ≤5 points and the patient was aged ≤78 years. A score of ≤5 points for the controlling bladder item of BI along with young recipient age was associated with high caregiver burden that induces depression among caregivers. This approach is useful to identify caregivers with high caregiver burden who are at risk for depression.
1. Introduction
The health of family caregivers is crucial for older and disabled people to continue to live at home. Occupational therapists who provide home-based rehabilitation services should support the patients and pay attention to the mental state of family caregivers, reduce the burden of care, and provide necessary support. A large-scale population-based study on 4128 family caregivers of community-dwelling older people under the Long-Term Care Insurance program in Japan reported that 34.2% of the family caregivers were at risk for depression [1]. Furthermore, caregiver depression was associated with high caregiver burden in a large-scale survey in Japan [2] and in a meta-analysis study [3]. Additionally, Arai and Zarit [2] reported that a cutoff score of 13 points in the short version of the Japanese version of the Zarit Caregiver Burden Interview (J-ZBI_8) was associated with depression [4, 5]. Therefore, appropriate support is needed to maintain the J-ZBI_8 score below 13 points to prevent the incidence of depression among caregivers.
Caregiver burden is associated with various elements, including patient factors, caregiver characteristics, and the relationship between patients and caregivers. Patient factors include age [6–8], gender [7], educational level [9, 10], functional disability [7, 11], cognitive impairment [9, 12, 13], and poor activities of daily living (ADL) [10, 12–15]. Occupational therapists are often involved in ADL. Additionally, eating [16], grooming [17, 18], dressing [12, 17, 18], mobility [19, 20], transfer [21], bathing [12, 16, 18], and bowel and bladder management [7, 12, 17, 20, 22–24] have been reported to be associated with caregiver burden. However, to the best of our knowledge, the level of assistance and ADL items that increase the caregiver burden is unknown. Further, the combination of factors associated with high caregiver burden remains elusive.
Therefore, this study was aimed at determining the cutoff values of ADL and the combination of related factors associated with high caregiver burden that induces depression among caregivers. The findings will be useful for occupational therapists to determine ADLs that should be prioritized for intervention based on the caregiver burden. It may also be useful to identify caregivers at risk for depression. […]
[Abstract] A Home-based Tele-rehabilitation System with Enhanced Therapist-patient Remote Interaction: A Feasibility Study
Posted by Kostas Pantremenos in REHABILITATION, Tele/Home Rehabilitation on June 12, 2022
Abstract:
As a promising alternative to hospital-based manual therapy, robot-assisted tele-rehabilitation therapy has shown significant benefits in reducing the therapist’s workload and accelerating the patient’s recovery process. However, existing telerobotic systems for rehabilitation face barriers to implementing appropriate therapy treatment due to the lack of effective therapist-patient interactive capabilities. In this paper, we develop a home-based tele-rehabilitation system that implements two alternative training methods, including a haptic-enabled guided training that allows the therapist to adjust the intensity of therapeutic movements provided by the rehabilitation device and a surface electromyography (sEMG)-based supervised training that explores remote assessment of the patient’s kinesthetic awareness. Preliminary experiments were conducted to demonstrate the feasibility of the proposed alternative training methods and evaluate the functionality of the developed tele-rehabilitation system. Results showed that the proposed tele-rehabilitation system enabled therapist-in-the-loop to dynamically adjust the rehabilitation intensity and provided more interactivity in therapist-patient remote interaction.
[Abstract] A Survey of Technologies Facilitating Home and Community-Based Stroke Rehabilitation
Posted by Kostas Pantremenos in REHABILITATION, Tele/Home Rehabilitation on May 2, 2022
Abstract
Stroke is a cardiovascular and cerebrovascular disease that affects the aged population at a high rate. Patients’ functional disabilities can be reduced with effective rehabilitation training. However, due to a lack of hospital resources and a social yearning for family contact, patients frequently discontinue rehabilitation training sessions and return home to their local community. Such a shift emphasizes the value of home and community-based rehabilitation, where patients can perform daily training with remote support from therapists. In this survey, the technologies that assist stroke rehabilitation will be discussed in following aspects: (1) technologies for home-based stroke rehabilitation; (2) technologies for community-based stroke rehabilitation; (3) technologies for therapist’s engagement in remote rehabilitation. A comprehensive overview of technologies that support home and community-based stroke rehabilitation was presented, as well as insights into future research themes.
[Report] A Transnational Home-Based Rehabilitation Service Delivery Model – PDF file
Posted by Kostas Pantremenos in REHABILITATION, Tele/Home Rehabilitation on January 21, 2022
Introduction
The European Commission aims to assist the EU Member states to enhance their health systems and
the health of their citizens. In a report by the European Union (2018), it was observed that, in order
to be more effective, health care systems need to be more people-centred to efficiently handle the
care of people living with chronic conditions. The report also highlights the need for more prevention
and improving access to healthcare. Finally, it was stated that healthcare systems should be resilient,
i.e. able to adapt to changing environments and needs. Thus, it is vitally important that health care
system services are appropriately designed, evolved, and modelled to reflect and implement these
desired characteristics.
Service design is the activity of planning and organising people, infrastructure, communication, and
resources of a service in order to improve its quality and the interaction between the service provider
and its users. If service design is conducted successfully, it can help predict failures, extract critical
points, and consider the intangible and contextual part of the product (Marin et al., 2017). Research
work conducted by Strasser et al. noted that to achieve sustainability, remote and rural communities
require health service models that are designed within and for these settings and are responsive to
local population health needs (Strasser et al. 2018). While service models cover many aspects of health
services, this work will focus on developing a health service model for home-based rehabilitation.
There are a number of challenges in designing a service delivery model. For example, delivery models
usually involve multiple stakeholders having a diverse set of needsthat must be considered (European
Union, 2018). In addition, there are many technologies available that appear suitable to solve the
same problem. However, distinguishing which technology is the most appropriate for a specific
condition can be overwhelming for health professionals. There are a number of factors which must be
considered by health professionals when considering a particular technology. For example, factors
such as; validity, reliability, effectiveness, efficiency, accuracy, connectivity issues, usability in a reallife scenario, comfortability to wear, intuitiveness, or whether training or technical support will be
necessary all must be considered. For example, in the UK, it is not recommended that patients
purchase assistive living technology without seeking advice from their occupational therapist or
General Practitioner (GP) (Which?, 2020).
Given the significant challenges involved, the design of a service delivery model which incorporates
wearable technology will ultimately have to focus on solving a problem that goes further than the
development of the technology itself. According to Marin et al. (2019), it is necessary to consider the
specific context and how the technology will be utilised. During the development, we aim to identify
the key steps of the process, predict and prevent failures, and take into account intangible and
contextual aspects of the product. Therefore, the design of our service delivery model follows a
Person-Centred Care (PCC) approach. The Health Foundation states that PCC is a new and evolving
area with no single definition (The Health Foundation, 2015). It can be used to relate to several
activities and principles. The underpinning rationale is that it depends on a specific patient´s needs,
preferences, and circumstances, which are subject to change over time. The Health Foundation
identified a Framework that includes four principles of PCC (See Figure 1). These principles are: (1)
Affording people dignity, compassion and respect, (2) Offering coordinated care, support or
treatment, (3) Offering personalised care, support or treatment, and (4) Supporting people to
recognise and develop their own strengths and abilities to enable them to live an independent and
fulfilling life.[…]
[RESEARCH] Spatiotemporal, Kinematic and Kinetic Assessment of the Effects of a Foot Drop Stimulator for Home-Based Rehabilitation of Patients with Chronic Stroke — A Three-Dimensional Motion Analysis – Full Text
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, Tele/Home Rehabilitation on November 7, 2021
Abstract
Background: Gait disability affects the daily lives of patients with stroke in both home and community settings. An abnormal foot–ankle position can cause instability on the supporting surface and negatively affect gait. Our research team explored the ability of a portable peroneal nerve-targeting electrical stimulator to improve gait ability by adjusting the foot–ankle position during walking in patients with chronic stroke undergoing home-based rehabilitation.
Methods: This was a double-blinded, parallel-group randomized controlled trial. Thirty-one patients with chronic stroke and ankle–foot motor impairment were randomized to receive 3 weeks of gait training, which involved using the transcutaneous peroneal nerve stimulator while walking (tPNS group; n = 16, mean age: 52.25 years), or conventional home and/or community gait training therapy (CT group; n = 15, mean age: 54.8 years). Functional assessments were performed before and after the 3-week intervention. The outcome measures included spatiotemporal gait parameters, three-dimensional kinematic and kinetic data on the ankle-foot joint, and a clinical motor and balance function assessment based on the Fugl–Meyer Assessment of Lower Extremity (FMA-LE) and Berg Balance scales (BBS). Additionally, 16 age-matched healthy adults served as a baseline control of three-dimensional gait data for both trial groups.
Results: The FMA-LE and BBS scores improved in both the tPNS groups (p = .004 and .001, respectively) and CT groups (p = .034 and .028, respectively) from before to after training. Participants in the tPNS group exhibited significant differences in spatiotemporal gait parameters, including opposite foot off, double support, stride length, and walking speed, after training (p = .010, .042, .017 and .001, respectively). Additionally, the tPNS group exhibited significant differences in kinematic parameters, such as the ankle angle at the transverse plane (p = .021) and foot progression angle at the frontal plane (p = .009) upon initial contact, and the peak ankle joint angle at the transverse plane (p = .023) and foot progression angle at the frontal and transverse planes (p = .032 and .046, respectively) during gait cycles after 3 weeks of training.
Conclusions: Use of a portable tPNS device during walking tasks appeared to improve spatiotemporal gait parameters and ankle and foot angles more effectively than conventional home rehabilitation in patients with chronic stroke. Although guidelines for home-based rehabilitation training services and an increasing variety of market devices are available, no evidence for improvement of motor function and balance was superior to conventional rehabilitation.
Background
Stroke is one of the five leading causes of disability-adjusted life-years worldwide [1]. In China, the increasing incidence of stroke and decrease in related mortality have led to a rapid increase in the burden of decrease associated with this condition [2]. Gait dysfunction is common among stroke survivors and represents a major burden [3, 4]. After stroke, most patients experience abnormal lower extremity movement and a plantarflexion or inversion pattern of hemiplegia in the ankle and foot during the swing phase of gait [5]. Estimates suggest that 20–30% of stroke survivors experience ankle and foot drop and/or inversion, which causes abnormal gait [4]. Ankle–foot drop and inversion are caused by abnormal activation of the musculature in the distal lower limb and result in inefficient foot clearance and foot tremor during the swing phase of gait and a less stable stance. Consequently, stroke patients tend to exhibit a compensatory gait pattern involving the affected side, such as steppage gait, hip hiking, toe walking, and forefoot walking. These pathological deviations reduce the walking speed and increase the risk of fall, thus impeding an individual’s ability to walk efficiently both indoors and outdoors and restricting their participation in many activities of daily life and the community. Therefore, studies on stroke motor recovery have frequently identified inadequate ankle–foot control and stability during walking as a key factor to address when attempting to improve gait dysfunction [6-9].
Approaches such as ankle–foot orthosis (AFO), electrical stimulation (ES), and neuroprosthetic implants are used to treat drop foot in stroke survivors [10-12], and a meta-analysis revealed that these approaches yielded similar results [12]. AFO is a traditional treatment for ankle joint immobilization in the neutral position and can be used to support ankle dorsiflexion during the swing phase to improve gait stability. However, as a mechanical device, an AFO only restricts ankle movement when it is worn, leading to weakened muscles, reduced muscle activity and a restricted ankle range-of-motion over the long term [13, 14]. ES, an alternative approach, is widely used to achieve more physiological positioning of the ankle and foot and to improve ankle–foot function, for example neuromuscular electrical stimulation (NMES), functional electrical stimulation (FES) multichannel and neuroprosthetic implants with the development of electronic engineering technology[8, 15-17], but multichannel and implanted devices are not used widely in the clinical settings, which limits their translational use in community and home settings.
Studies conducted in the last 10 years have focused on volitional muscle activation combined with lower motor neuron stimulation, which contributes to several possible mechanisms of neuromuscular plasticity, including repeated muscle contractions leading to increased oxidative capacity; increased numbers of microcapillaries and changes in fiber type at the muscular level; and the convergence of orthodromic or antidromic impulses at the anterior horn, leading to the strengthening of synapses at the spinal level and changes in the cortex [17-19]. These effects of therapy culminate in increased volitional muscle activity in the weak dorsiflexors and evertors of the ankle. Such changes are thought to positively influence other biomechanical features and help restore the associated functions. Several studies have observed sustained improvements in volitional muscles after removal of therapeutic devices, particularly in terms of improved gait capacity during the chronic post-stroke stage [19-21] . One type of FES treatment, the transcutaneous peroneal nerve stimulator (tPNS), involves the placement of electrodes on the skin surface above the peroneal nerve, and based on the mechanisms of effects on volitional muscle activity combined with lower motor neurone stimulation during walking to acquire a more physiological positioning of ankle and foot. This clinically accepted rehabilitation intervention has been demonstrated to be more efficient than AFO, especially in terms of improving walking speed [22, 23]. However, a multicenter prospective randomized study found that the use of peroneal nerve FES was equivalent to device-free gait training in terms of the clinical outcomes of improvements in walking speed, the Fugl–Meyer Assessment of Lower Extremity (FMA-LE) score, ankle muscle strength and dorsiflexion performance [24].
Above studies in different views of the tPNS suggest that this therapeutic device is an appropriate alternative therapeutic device using at chronic stroke survivors for gait training. Other studies have focused on the physiological and biomechanical effects of tPNS on the kinematics and kinetics of the hip, knee, and ankle joints [16, 22, 25]. However, excessive pronation and supination of the foot and hyper-planta/dorsiflexion of the ankle joint directly result in an abnormal and unstable stance and toe clearance during walking, leading to a tilted posture and increasing the fall risk. This study focused on quantitative analysis of kinematics and kinetics of the ankle joint and foot progression angles and spatiotemporal gait and clinical assessment parameters. We aimed to determine the efficacy of tPNS and its feasibility for use as a rehabilitation training tool in home and community settings. This is important because most discharged stroke patients in China receive inadequate rehabilitation training at home due to a shortage of rehabilitation therapists. […]

[WEB] Motus Nova Stroke Rehab Recovery at Home
Posted by Kostas Pantremenos in REHABILITATION, Rehabilitation robotics, Tele/Home Rehabilitation on July 19, 2021
CLINICALLY PROVEN STROKE REHABILITATION
Motus users are making Recoveries from Stroke. Reach your recovery goals faster.
When conventional rehabilitation is too slow, Motus is the answer for stroke recovery: a home based program revolutionizing stroke rehabilitation whether you are ten days or ten years after brain injury.
REAL STROKE SURVIVORS. REAL RECOVERIES.
Our users Make Functional Gains. This is a step back in your life after stroke and brain injury.
Hemiparesis from stroke is not your life. This is technology to get you back to the real you. Prove them wrong–those that say you can’t get any better. Motus users say they’ve made more gains in weeks or months than they have in years of traditional rehab.
For more Visit site
[Abstract] Development of a Home-based Hand Rehabilitation Training and Compensation Feedback System
Posted by Kostas Pantremenos in Paretic Hand, Tele/Home Rehabilitation on December 19, 2020
Abstract
Stroke survivors often show a limited recovery in the hand function even after the recovery period (3-6 months after stroke) and at-home hand rehabilitation is common due to the long-term nature of hand rehabilitation and the limited medical resources. We designed a home-based hand rehabilitation training and compensation feedback system. A low-cost simple orthosis glove, a set of hand rehabilitation training games and a compensation detection and feedback module were designed and developed in this system. A preliminary test was carried out on the system and the results showed that the training section (the orthosis glove and the hand rehabilitation training games) of the system was friendly to the subjects and the subjects were more receptive to the system and the compensation detection and feedback module had a promising performance. This system can not only provide high intensity and incentive hand rehabilitation training, but also guide the stroke patients to correct wrong upper body postures during the training process, which can achieve better rehabilitation results. The system has the potential to become an effective home-based hand rehabilitation training and compensation feedback system.
[Abstract] Patient experience using digital therapy “Vigo” for stroke patient recovery: a qualitative descriptive study
Posted by Kostas Pantremenos in Artificial intelligence, Assistive Technology, REHABILITATION, Tele/Home Rehabilitation on November 7, 2020
Abstract
Background: The digital assistant “Vigo” is a computer-generated artificial intelligence-based application that serves as a digital assistant to a stroke patient and his family. With its conversational chatbot and gamification elements it counsels, educates, and trains the stroke patient and patient’s family on stroke, rehabilitation, care, and other related issues.
Aim: This study describes insights about The digital assitant “Vigo” usability from a patients’ perspective.
Methods: Twelve patients tested the application at their home environment. Three semi-structured interviews were conducted with each participant to obtain information on the usability of the application. Deductive thematic analyses were used to analyze trancripts.
Results: Participants expressed their opinions on music, pictures, video and audio files, chat options, layout, text, name of application and stand that is used for placement of devices on which “Vigo” is installed on. All participants generally evaluated application as transparent, understandable, and handy. The overall design of the application was rated as good. Participants were mostly unsatisfied with difficulty level and diversity of exercises.
Conclusions: Participants had a positive attitude towards using tablet tehchnologies in their home environment. Users of digital assistant “Vigo” acknowledged its ability to support, give educational information and increase participation in therapeutic activities. Implications for rehabilitation Tablet application can support, give educational information, and increase participation in therapeutic activities for persons after stroke. As home-based rehabilitation tool, the content of the application must be simple, flexible, and diverse, to face the challenges of meeting each individual’s goals, functional needs and abilities.
