Abstract and Introduction
Abstract
Stroke is the most common serious neurological disorder. To date, the focus for research and trials has been on prevention and acute care. Many patients are left with serious neurological impairments and limitations in activity and participation after stroke. Recent preliminary research and trials suggest that the brain is ‘plastic’ and that the natural history of stroke recovery can be improved by physical therapy and pharmacotherapy. Motor weakness and the ability to walk have been the primary targets for testing interventions that may improve recovery after stroke. Physical therapeutic interventions enhance recovery after stroke; however, the timing, duration and type of intervention require clarification and further trials. Pharmacotherapy, in particular with dopaminergic and selective serotonin-reuptake inhibitors, shows promise in enhancing motor recovery after stroke; however, further large-scale trials are required.
Introduction
This review is a framework around an emerging and exciting area of stroke care – maximizing recovery after stroke. Stroke care is a continuum from prevention to hyperacute care to acute care to rehabilitation to community reintegration and back (Figure 1). The traditional medical model of care artificially divides care across multiple healthcare providers and locations. Prevention is most often in the hands of general and primary care medicine with the goal of maximizing stroke risk reduction strategies such as controlling hypertension. Hyperacute stroke care is in the hands of neurologists with a primary goal of providing thrombolysis to as many patients as possible and as quickly as possible. Acute stroke care is in the hands of neurologists and very often in the hands of internal medicine specialists who manage patients according to best practices on acute stroke units in acute care hospitals. Rehabilitation is under the care of physical medicine and rehabilitation physicians and allied health professionals usually in rehabilitation hospitals. Reintegration into the community is in the hands of home care and out-patient providers in the community. One patient, one neurological disorder and so many different care providers and locations.
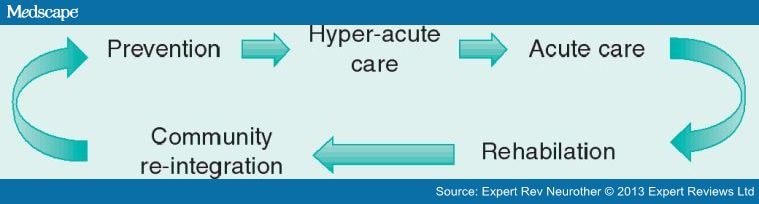
Figure 1.The continuum of stroke care.
Recent research suggests that we are at the edge of major advances in post-stroke care. Animal and human studies show that the brain is ready to heal immediately after a stroke. The brain is ‘plastic’ and responds to external influences, such as physical therapy. The timing, the intensity and the exact external influence may all be important factors in maximizing recovery. Pharmacotherapy may influence how the injured brain recovers. This complex array of influences and recent research addressing these areas will be elaborated on in this review (Figure 2).

Figure 2.
Multiple factors may influence recovery after stroke.