Archive for category COVID-19
[ARTICLE] Stroke Recovery During the COVID-19 Pandemic: A Position Paper on Recommendations for Rehabilitation – Full Text
Posted by Kostas Pantremenos in COVID-19, REHABILITATION on December 31, 2022
Abstract
Health care delivery shifted and adapted with the COVID-19 pandemic caused by the novel severe acute respiratory syndrome coronavirus 2. Stroke care was negatively affected across the care continuum and may lead to poor community living outcomes in those who survived a stroke during the ongoing pandemic. For instance, delays in seeking care, changes in length of stays, and shifts in discharge patterns were observed during the pandemic. Those seeking care were younger and had more severe neurologic effects from stroke. Increased strain was placed on caregivers and public health efforts, and community-wide lockdowns, albeit necessary to reduce the spread of COVID-19, had detrimental effects on treatment and recommendations to support community living outcomes. The American Congress of Rehabilitation Medicine Stroke Interdisciplinary Special Interest Group Health and Wellness Task Force convened to (1) discuss international experiences in stroke care and rehabilitation and (2) review recently published literature on stroke care and outcomes during the pandemic. Based on the findings in the literature, the task force proposes recommendations and interdisciplinary approaches at the (1) institutional and societal level; (2) health care delivery level; and (3) individual and interpersonal level spanning across the care continuum and into the community.
Statement of purpose
The COVID-19 pandemic caused by the novel severe acute respiratory syndrome (SARS) coronavirus (CoV) 2 posed unprecedented challenges to health care systems around the world. It is expected that the fallout from the COVID-19 pandemic will directly affect people who experience stroke during this time. The Health and Wellness Task Force within the American Congress of Rehabilitation Medicine Stroke Interdisciplinary Special Interest Group is concerned that during the ongoing pandemic, fewer people are seeking stroke care, and more people with stroke are living with the effects of untreated stroke or being discharged with minimal rehabilitation or without critical early and intensive rehabilitation that is recommended for improving stroke outcomes.1 The purpose of this position article is to describe ongoing challenges and opportunities to support the short- and long-term needs of people surviving stroke during the COVID-19 pandemic. The task force proposes potential solutions across the care continuum to support a multilevel and interdisciplinary approach that addresses this major public health problem.
Rationale for position paper
Enduring a stroke during the pandemic
Before the COVID-19 pandemic, stroke was widely regarded as a leading global cause of disability2, 3, 4 and the second leading cause of death (11.6% of global mortality).5 Despite advancements in medical interventions that increased stroke survival, disparities in stroke mortality and disability were prevalent, partly because of differences in country income and medical care quality (eg, cost, access, availability).3 The COVID-19 pandemic presented an additional risk factor for stroke: COVID-19 infection. While there is no exact mechanism linking COVID-19 to stroke, vascular symptoms associated with COVID-19 such as hypercoagulability and arterial and venous thrombosis are believed to be contributing factors to increased risk of stroke.6, 7 Other coronavirus respiratory syndromes of the same nature including the SARS-CoV-1 and Middle East Respiratory Syndrome coronavirus were also related to increased incidence of acute ischemic stroke.7 Further, people with stroke risk factors (eg, diabetes, smoking) have an increased COVID-19 mortality rate, possibly because of the same mechanisms attributed to stroke risk, such as large expression of angiotensin-converting enzyme 2 cell receptors for binding to SARS-CoV-2.8
Common deficits after stroke include impaired motor function; impaired ability to carry out activities of daily living; cognitive impairments in memory, language, attention, and executive function; and affected mood, sensation, and perception.9 10 Stroke attributed to the SARS-CoV-2 infection can cause greater severity of stroke,11 potentially leading to prolonged acute care and rehabilitation.12 Natural recovery of broad stroke-related impairments often occurs with haste within the first 6 months post stroke and then tends to plateau, although this may vary for cognitive, physical, and sensory-perceptual impairments.13 It is difficult to predict individual recovery because sequelae are multifaceted across multiple domains. As such, rehabilitation clinicians rely on their own judgment as to when to end rehabilitation post stroke.13 The long-term effects and recovery trajectory for individuals with simultaneous SARS-CoV-2 infection and stroke is unknown.
Stroke care
Before the COVID-19 pandemic, patients with stroke symptoms received hyperacute and acute treatment at the nearest specialist stroke unit, primary stroke center, or comprehensive stroke center.14 After acute treatment, the patient entered 1 of 2 main pathways for poststroke rehabilitation: (1) subacute rehabilitation (eg, inpatient rehabilitation, skilled nursing facility); or (2) community rehabilitation, normally delivered via an outpatient facility or in the patient’s home.15
A large-scale RCT of working-aged survivors of stoke across the UK, Australia, and Southeast Asia found that within 3 months post stroke, 67% of survivors of stroke received either inpatient or community rehabilitation, and only 8% of those were still receiving rehabilitation 12 months post stroke.15Those with milder strokes had the highest rates of receiving no rehabilitation (40%), followed by a lower proportion of those with moderate strokes (12%) and severe strokes (4%) who required no rehabilitation.15
During the pandemic, regions with high incidence of COVID-19 were forced to reorganize health care services. This included implementation of triage systems, separating patients with confirmed or suspected COVID-19 from patients without COVID-19 and redeploying health care professionals to the frontline to deal with the influx of patients with COVID-19.16, 17, 18
Resources and clinicians were spread across usual clinical care and COVID-19 specific care, increasing the potential short- and long-term negative consequences of high stress and burnout.19
An overwhelmed health care system, attributed to reassignment of staff or beds, increased patient admissions without adequate staffing, and increased resource strain, likely led to care and service limitations.20
Overarching rationale
Given the substantial number of adults enduring stroke annually, it is necessary to understand and address their needs during the ongoing COVID-19 pandemic. While it is well-documented that interdisciplinary stroke rehabilitation can enhance outcomes after stroke, the substantial shift in health care delivery during the COVID-19 pandemic may have major effects on short- and long-term outcomes. Researchers must further examine stroke outcomes related to the COVID-19 pandemic. Practitioners must be prepared to identify problems and challenges among this population to address the fallout the pandemic has imparted on a generation of survivors of stroke.[…]
[ARTICLE] A review of the potential neurological adverse events of COVID-19 vaccines – Full Text PDF
Posted by Kostas Pantremenos in COVID-19 on November 20, 2022
Abstract
Despite the advantages of getting access to the coronavirus disease 2019 (COVID-19) vaccines, their potential ability to induce severe adverse events (AEs) has been a significant concern. Neurological complications are significant among the various adverse events following immunization (AEFI) due to their likely durability and debilitating sequelae. Neurological AEs following COVID-19 vaccination can either exacerbate or induce new-onset neuro-immunologic diseases, such as myasthenia gravis (MG) and Guillain–Barre syndrome (GBS). The more severe spectrum of AEs post-COVID19 vaccines has included seizures, reactivation of the varicella-zoster virus, strokes, GBS, Bell’s palsy, transverse myelitis (TM), and acute disseminated encephalomyelitis (ADEM). Here, we discuss each of these neurological adverse effects separately.
Follow the link to read the full content: https://rdcu.be/cZ1Oz
[REVIEW] Do digital interventions increase adherence to home exercise rehabilitation? A systematic review of randomised controlled trials – Full Text
Posted by Kostas Pantremenos in COVID-19, REHABILITATION, Tele/Home Rehabilitation on November 7, 2022
Abstract
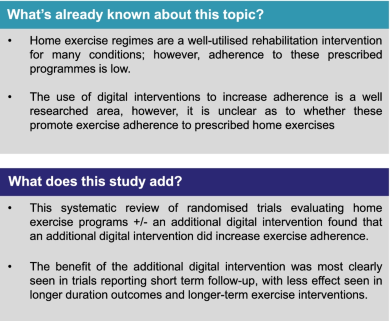
Background
Home exercise regimes are a well-utilised rehabilitation intervention for many conditions; however, adherence to prescribed programmes remains low. Digital interventions are recommended as an adjunct to face-to-face interventions by the National Health Service in the UK and may offer increased exercise adherence, however the evidence for this is conflicting.
Method
A systematic review was undertaken using MEDLINE and CINAHL databases using the PRISMA guidelines. Randomised controlled trials in any clinical population evaluating the adherence to prescribed home exercise interventions with and without additional digital interventions were included. Publication quality was assessed using the Cochrane Risk of Bias tool.
Results
The search strategy returned a total of 1336 articles, of which 10 randomised controlled trials containing data for 1117 participants were eligible for inclusion. 565 participants were randomised to receive the interventions, and 552 to the control. Seven of the ten trials reported a significant difference in adherence between the control and intervention groups favouring an additional digital intervention. Three trials reported equivalent findings. These three reported longer-term outcomes, suggesting an interaction between adherence and duration of intervention. There was substantial heterogeneity in outcome assessment metrics used across the trials prohibiting formal meta-analysis. This included studies were of low to moderate quality in terms of risk of bias.
Conclusion
The addition of a digital interventions to prescribed home exercise programmes can likely increase exercise adherence in the short term, with longer term effects less certain.
Introduction
The emerging use of digital technology in physiotherapy service delivery has been discussed for years; however, the recent Covid-19 pandemic caused major disruption to face-to-face clinical interactions with most outpatient appointments ceased abruptly in March 2020. There is a new focus on health services operating under a more blended approach, incorporating both face-to-face and digitally augmented appointments and treatments [1].
There is already a well-established use of digital technology to augment clinical management in conditions such as diabetes, chronic obstructive pulmonary disease (COPD), chronic heart failure and cardiovascular disease [2, 3]. Patient centred exercise prescription is a well-recognised therapeutic intervention [4], and home exercise programs are frequently provided to patients as part of clinical rehabilitation or to help self-manage long-term conditions [5]. Completing the recommended exercise prescription and adhering to these exercises brings about long-term benefits, which may include better physical function, reduced pain and being able to reach agreed goals [6]. Long-term adherence can also have a considerable benefit in patients’ quality of life and can have a positive benefit on the economy as it can reduce the burden on healthcare systems, as patients are able to self-manage more effectively [7]. A well-established problem when delivering rehabilitation interventions however is the low adherence rate to home exercise programs [8].
Adherence can be defined as ‘the degree a behaviour corresponds with an agreed-on recommendation’ [9]. It has been reported by Argent et al. [10] that adherence to home exercise programs supplied by physiotherapists could be as low as 50%. Low levels of adherence, specifically mid- to long-term, can limit the effectiveness of rehabilitation and may lead to reoccurrence of injuries or not being able to self-manage long-term conditions, resulting in pain, reduced function and subsequently negative outcomes [11].
Adherence, as a concept, is not well understood by researchers [12]. There are many reasons why a patient may struggle to adhere to exercise programmes, which may include perceived barriers such as not having enough time, work schedules, reduction in self-efficacy, the belief that the treatment is ineffective or seeing early positive results so they then feel they do not need to continue with the treatment [10].
There are many forms of digital technology; from mobile applications to websites to simple phone calls. These technologies can help patients self-manage long term conditions or rehabilitate after an injury by providing education, advice, information, feedback and communication from rehabilitation practitioners, which can in turn enhance a patient’s motivation [13].
The use of digital interventions to improve physical outcomes is well researched area, however, surprisingly, there is little consensus as to whether digital interventions promote exercise adherence in patients undergoing physiotherapy [13]. The aim of this review was therefore to evaluate whether the addition of digital interventions to physiotherapist prescribed home exercise programs for any specified clinical condition improved adherence to these programs.[…]
[Abstract] Experiences investigation for COVID‐19 vaccination in patients with epilepsy
Posted by Kostas Pantremenos in COVID-19, Epilepsy on November 2, 2022
Abstract
Objective
This study aimed to investigate the safety of COVID-19 vaccination in patients with epilepsy (PWE) and their willingness to undergo vaccination.
Methods
This was a survey study. A questionnaire was completed by patients of the outpatient clinic and hospital ward at The Third Xiangya Hospital in 2021. The survey included general, epilepsy-specific, and COVID-specific questions.
Results
In total, 120 valid questionnaires were returned. Eighty-nine of 120 patients (74.2%) were not vaccinated, and 31 (25.8%) received the COVID-19 vaccine. Of the 31 vaccinated PWE, one (3.2%) had worsening of seizures and four (12.9%) had adverse reactions that were characteristic of the COVID-19 vaccine. The other 26 patients (83.9%) reported no adverse reactions, Moreover, there was no significant difference between the 18 PWE with well-controlled seizureand the 13 PWE with poorly-controlled seizure. Of the 89 unvaccinated PWE, 69.7% (62/89) were willing to receive the COVID-19 vaccine, 28.1% (25/89) were unsure, and 2.2% (2/89) declined to be vaccinated.
Significance
Among PWE, few adverse reactions occurred following the COVID-19 vaccination. Most PWE were willing to receive the COVID-19 vaccine. COVID-19 vaccination is safe for PWE.
[Abstract] Safety and Adverse Events Following COVID-19 Vaccination among People with Epilepsy: A Cross-Sectional Study
Posted by Kostas Pantremenos in COVID-19, Epilepsy on October 13, 2022
Abstract
Objective
Epilepsy is an under-discussed non-communicable disease costing massive burden globally. It is known that there is increased prevalence of morbidity and mortality following COVID-19 infection among people with epilepsy (PWE). However, there is limited information about the adverse events following COVID-19 immunisation among PWE. Hence, this study aimed to assess the safety and adverse events following immunisation (AEFI) of COVID-19 vaccinations among PWE who follow up in our centre, with a focus on neurologic AEFI.
Methods
This cross-sectional study recruited 120 adult PWE who are under the follow-up of the Neurology Clinic, Universiti Kebangsaan Malaysia Medical Centre (UKMMC). Consent-taking was conducted via synchronous or asynchronous approaches, followed by a phone call interview session. The interview collected socio-demographic information, epilepsy-related variables, and vaccination-related variables. Univariate analysis and multiple logistic regression analysis were done to confirm factors associated with the AEFI of COVID-19 vaccinations.
Results
Among all types of COVID-19 vaccines, most of the PWE received the Cominarty® COVID-19 vaccination (52.5%). Overall, local AEFI was the quickest to develop, with an average onset of within a day. PWE with normal body mass index (BMI) have a higher risk of developing both local and systemic AEFI compared to those underweight and obese PWE. (OR: 15.09, 95% CI 1.70-134.28, p=0.02).
Significance
COVID-19 vaccine is safe for PWE. AEFI among PWE are similar to the general population following COVID-19 vaccination. Therefore, clinicians should encourage their PWE patients to take COVID-19 vaccine.
[ARTICLE] Neurological consequences of COVID-19 – Full Text
Posted by Kostas Pantremenos in COVID-19 on October 5, 2022
Abstract
In December 2019, cases of pneumonia caused by infection with the previously unknown severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), leading to coronavirus disease 2019 (COVID-19), were identified. Typical manifestations of COVID-19 are fever, cough, fatigue and dyspnoea. Initially, it was thought that the mechanism of action of SARS-CoV-2 was only associated with respiratory tract invasion, but it was later revealed that the infection might involve many other organs and systems, including the central and peripheral nervous systems. Neurological complications associated with SARS-CoV-2 infection include encephalopathy, encephalitis, meningitis, acute disseminated encephalomyelitis (ADEM), ischaemic and haemorrhagic stroke and cerebral venous sinus thrombosis. In cases of peripheral nervous system involvement, smell and taste disorders, myopathy or the signs and symptoms of Guillain‒Barré syndrome are observed. The most common early neurological complications, particularly during the first year of the epidemic, were anosmia and taste disorders, which, according to some studies, occurred in over 80 percent of patients with COVID-19. The proportion of patients with serious neurological manifestations was small compared to the global number of patients, but the numbers of SARS-CoV-2 infections and critical patients increased substantially. The experience from 2 years of the pandemic has shown that approximately 13% of infected patients suffer from severe neurological complications. The relationship between SARS-CoV-2 and the nervous system is not only a cause of neurological complications in previously healthy individuals but also directly and indirectly affects the courses of many nervous system diseases.
Introduction
Coronaviruses have been known for years as pathogens that commonly occur in humans and animals. They are responsible for approximately 10–20% of common cold and mild respiratory tract infections. At the end of 2019, a newly mutated form of coronavirus that causes severe pneumonia was identified in Wuhan, China. The disease spread rapidly, resulting in an epidemic in China and then a pandemic. In February 2020, the World Health Organization (WHO) defined ‘COVID-19’ as a disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. On 11 March 2020, the WHO declared COVID-19 a pandemic. Nearly 550 million people were affected by the disease, and over 6 million people died over the next 2 years. Although the pandemic has not yet ended, it is already considered to be one of the most tragic epidemics in our history. The virus mainly attacks the respiratory system, but neurological complications following COVID-19 are common and develop in approximately 50 percent of patients [2].
Individuals with concomitant diseases (diabetes, hypertension or obesity) are at a particularly high risk of contracting the virus and suffering severe infection [3]. Genetic factors are also important. Certain patients with COVID-19 were seriously ill, while others experienced few signs or symptoms. New research has helped identify over 1000 genes related to a severe course of COVID-19. Moreover, it has been shown that severe COVID-19 is highly associated with a poor reaction of two immune cell types: natural killer (NK) cells and T lymphocytes (the ‘CD56 bright’ subtype) [4].
Due to its relationship with the nervous system, SARS-CoV-2 infection not only causes neurological complications in previously healthy individuals but also affects the courses of many nervous system diseases.[…]
[WEB] Mental Health During the COVID-19 Pandemic
Posted by Kostas Pantremenos in COVID-19 on September 29, 2022
An Urgent Issue
Both SARS-CoV-2 and the COVID-19 pandemic have significantly affected the mental health of adults and children. In a 2021 study, nearly half of Americans surveyed reported recent symptoms of an anxiety or depressive disorder, and 10% of respondents felt their mental health needs were not being met. Rates of anxiety, depression, and substance use disorder have increased since the beginning of the pandemic. And people who have mental illnesses or disorders and then get COVID-19 are more likely to die than those who don’t have mental illnesses or disorders.
Mental health is a focus of NIH research during the COVID-19 pandemic. Researchers at NIH and supported by NIH are creating and studying tools and strategies to understand, diagnose, and prevent mental illnesses or disorders and improve mental health care for those in need.
How COVID-19 Can Impact Mental Health
If you get COVID-19, you may experience a number of symptoms related to brain and mental health, including:
- Cognitive and attention deficits (brain fog)
- Anxiety and depression
- Psychosis
- Seizures
- Suicidal behavior
Data suggest that people are more likely to develop mental illnesses or disorders in the months following infection, including symptoms of post-traumatic stress disorder (PTSD). People with long COVID may experience many symptoms related to brain function and mental health.
How the Pandemic Affects Developing Brains
The impact of the COVID-19 pandemic on the mental health of children is not yet fully understood. NIH-supported research is investigating factors that may influence the cognitive, social, and emotional development of children during the pandemic, including:
- Changes to routine
- Virtual schooling
- Mask wearing
- Caregiver absence or loss
- Financial instability
Not Everyone Is Affected Equally
While the COVID-19 pandemic can affect the mental health of anyone, some people are more likely to be affected than others. People who are more likely to experience symptoms of mental illnesses or disorders during the COVID-19 pandemic include:
- People from racial and ethnic minority groups
- Mothers and pregnant people
- People with financial or housing insecurity
- Children
- People with disabilities
- People with preexisting mental illnesses or substance use problems
- Health care workers
People who belong to more than one of these groups may be at an even greater risk for mental illness.
Telehealth’s Potential to Help
The pandemic has prevented many people from visiting health care professionals in person, and as a result, telehealth has been more widely adopted during this time. Telehealth visits for mental health and substance use disorders increased significantly from 2020 to 2021 and now make up nearly half of all total visits for behavioral health.
Widespread adoption of telehealth services may help people who otherwise would not be able to access mental health support, such as people in rural areas or places with few providers.

Frequently Asked Questions
I have a preexisting mental illness. Is COVID-19 more dangerous to me?
COVID-19 can be worse for people with mental illnesses. Data suggest that people who reported symptoms of anxiety or depression had a greater chance of being hospitalized after a COVID-19 diagnosis than people without those symptoms.
The Centers for Disease Control and Prevention (CDC) reports that having mood disorders and schizophrenia spectrum disorders can increase a person’s chances of having severe COVID-19. People with mental illnesses who belong to minority groups are also more likely to get COVID-19. And people with schizophrenia are significantly more likely to get COVID-19 and more likely to die from it.
Despite these risks, effective treatments are available. If you have a preexisting mental illness and get COVID-19, talk to your health care professional to determine the treatment plan that’s appropriate for you.
I’m experiencing symptoms of a mental illness or disorder. What should I do?
If you are experiencing symptoms of anxiety, depression, or any other mental illness or disorder, there are ways you can get help. For immediate help:
- Call 911
- Call or text the 988 Suicide & Crisis Lifeline at 988 (para ayuda en español, llame al 988)
- Call or text the Disaster Distress Helpline, 1-800-985-5990 (press 2 for Spanish)
- The Substance Abuse and Mental Health Services Administration can help you find mental health or substance use specialists.
- Talk to your health care professional or mental health care professional. Together, you can work on a plan to manage or reduce your symptoms.
What research is NIH doing on the mental health impacts of COVID-19?
The National Institute of Mental Health (NIMH) and other NIH Institutes have created research initiatives to address mental health for people in general and for the most vulnerable people specifically. Examples of this research include:
- NIMH launched a five-year research study called RECOUP-NY to promote the mental health of New Yorkers from communities hard-hit by COVID-19. The study will test the use of a new care model called Problem Management Plus (PM+) that can be used by non-specialists.
- A study funded by NIMH is examining the use of mobile apps to address mental health disparities.
- The Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) is funding research to understand the effects of mask usage for children, including any impacts on their emotional and brain development.
- NIMH is funding research on the impacts of the pandemic on underserved and vulnerable populations and on the cognitive, social, and emotional development of children.
- The National Institute on Alcohol Abuse and Alcoholism (NIAAA) is funding research on how COVID-19 and SARS-CoV-2 affect the causes and consequences of alcohol misuse.
- A collaborative study supported by NIMH and the National Center for Complementary and Integrative Health (NCCIH) enrolled more than 3,600 people from all 50 U.S. states to understand the stressors affecting people during the pandemic.
[ARTICLE] Covid-19 vaccines and neurological complications: a systematic review – Full Text
Posted by Kostas Pantremenos in COVID-19 on September 16, 2022
Abstract
The COVID-19 mainly causes respiratory disorders with high infection and severe morbidity and mortality. Neurologists have concerns about potential neurological side effects, profits, and timing of COVID-19 vaccines. This study aimed to review systematically research for the COVID-19 vaccine and neurological complications. Data was searched in Scopus, ISI web of knowledge, Medline, PubMed, Wiley, Embase, International Clinical Trials Registry Platform and Clinical Trials, Cochrane Library, and Google Scholar. Two reviewer authors individually searched and assessed the titles and abstracts of all articles. The third reviewer resolved disagreement between them. Data were documented regarding study location, study design, type of complications, number of patients, various types of COVID-19 vaccine, and type of neurological complications. Six studies in COVID-19 vaccine and neurological complications include two studies about neurological manifestations after the mRNA vaccines, four records about side effects of vector-based vaccine were included in the study. The main neurological complication associated mRNA vaccines were body aches, paresthesia, and difficulty walking, erythema migrans lesion, fatigue, myalgia, and pain in the left lateral deltoid region. The major neurological complication related to vector-based vaccines were urinary retention difficulty, feeding and ambulating, arm soreness, mild fatigue, chills, left-sided facial droop, headaches, a generalized epileptic seizure, hemianopia, and mild aphasia, acute somnolence and right-hand hemiparesis, acute transverse myelitis, deep vein thrombosis in her left leg, a vigilance disorder and a twitching, a severe immobilizing opsoclonus myoclonus syndrome, and encephalitis. A large spectrum of severe neurological unfavorable has been reported. These complications could occur as a result of molecular stimulation and later neuronal damage. Generally, the advantages of COVID‐19 vaccination are dominant on the risks of a neurological complication at both individual and population levels. Future investigations will be required to find any relationship between neurological complications and COVID‐19 vaccines principally as new strains of the virus and new vaccines are technologically advanced against them.
1 Introduction
COVID-19 infection is a global pandemic disease that was reported in Wuhan, China, in December 2019 for the first time. The COVID-19 mainly causes respiratory disorders with high infection and severe morbidity and mortality. The symptoms of COVID-19 include sore throat, myalgia, fever, cough, anosmia, and diarrhea [1]. The symptoms are incidence moderate to severe acute respiratory distress syndrome, multiple organ failure, and eventually death [2].
There are numerous vaccine platforms (i.e., mRNA, DNA, nonreplicating viral vectors, etc.) for administrating this global pandemic disease around the world [3]. The FDA approved two vaccines to prevent COVID-19 infection in December 2020. There are four major vaccine mechanisms for the COVID‐19 vaccines production, including protein‐based vaccines, mRNA‐based vaccines, DNA‐based vaccines, and inactivated virus that motivates the immune response [2], [3], [4].
At first, two patients incidence transverse myelitis after Oxford/AstraZeneca vaccination. Therefore, concerns about neurological complications from COVID‐19 vaccines increased [5]. One patient had pre‐existing multiple sclerosis; thus, it may not be related to the vaccination, whereas the other patient was determined to be probably associated with the vaccination [6]. The Clinical trials from the mRNA vaccine demonstrated that seven cases (of 37,000 vaccine recipients) had Bell’s palsy, and any case had not incident Guillain–Barre syndrome (GBS) [7]. One patient had the GBS in the Johnson & Johnson vaccine trial [8]. Likewise, no relationship between GBS and COVID‐19 infection has been found [9].
The most prevalent neurological signs included headache, dizziness, pain, myalgia, muscle spasms, and paresthesia, which are anticipated to transpire as acute, transient special effects after vaccination. Infrequent cases of dysphonia, diplopia, tremor, seizures, tinnitus, and repetition of herpes zoster have been reported [10]. However, some neurological patients also received the vaccination, thus neurological signs occur inside the post‐vaccination window accidentaly. To reports, there has not been an alert indicating more increased rates of neurological disorder related to the COVID‐19 vaccines.
The patients who receive immunosuppressive drugs should have special attentions around COVID‐19 vaccines, despite there is no absolute neurological disorder about COVID‐19 vaccination [11]. These patients potency be at developed risk for severe COVID‐19, doing vaccination principally vital. However, immunosuppressive drugs may decrease immune responses to vaccination [11]. Consequently, timing of the vaccine performance plays an essential role in matching immune response [12, 13].
Numerous neurological complications are associated with COVID-19 infection [2, 3]. Neurologists have concerns about potential neurological side effects, profits, and timing of COVID-19 vaccines. Therefore, this study aimed to review systematically research for the COVID-19 vaccine and neurological complications to achieve a comprehensive view and management of neurological diseases in COVID-19 periods.[…]
[Review] Should patients with epilepsy be vaccinated against coronavirus disease 2019? A systematic review and meta-analysis – Full Text
Posted by Kostas Pantremenos in COVID-19, Epilepsy on July 2, 2022
Highlights
•The vaccination coverage and willingness to be vaccinated against COVID-19 were still low in patients with epilepsy.
•Seizure status rather than seizure type associated with COVID-19 unvaccination.
•Vaccination against COVID-19 appears to be well-tolerated and safe in patients with epilepsy.
•Our findings supporting a positive outlook towards the vaccination in this population.
Abstract
Objective
The coronavirus disease 2019 (COVID-19) vaccination coverage, willingness, and safety profiles in patients with epilepsy remain poorly understood. We aimed to summarize the available evidences of COVID-19 vaccination coverage, willingness, and safety profiles among patients with epilepsy.
Methods
We performed a literature search in the Pubmed, EMBASE, and Cochrane Central Register database between 1 January 2020 and 30 April 2022. We included eligible studies that provided information on the COVID-19 vaccination coverage, willingness, and safety profiles among patients with epilepsy. We investigated the association between baseline characteristics of patients with epilepsy and unvaccination status using a fixed-effect model. We calculated the pooled overall willingness to be vaccinated against COVID-19. We systematically reviewed the safety profiles after COVID-19 vaccination in patients with epilepsy.
Results
Ten eligible observational studies and two case-reports yielded 2589 participants with epilepsy or their caregivers. Among 2145 participants that provided the information of vaccination status, 1508 (70.3%) patients with epilepsy were not administered COVID-19 vaccine, and 58% (95%CI 40% – 75%) of respondents were willing to be vaccinated against COVID-19. Seizure status (active versus inactive, OR 1.84 95%CI 1.41 – 2.39, I2 = 0%) rather than seizure type (focal versus non-focal, OR 1.22 95%CI 0.94 – 1.58, I2 = 0%) was associated with COVID-19 unvaccination status. Vaccines were well-tolerated; epilepsy related problems such as increase in seizure frequency and status epilepticus after COVID-19 vaccination were uncommon.
Conclusions
Our findings suggest a low COVID-19 vaccination coverage and willingness in patients with epilepsy. Vaccination against COVID-19 appears to be well-tolerated and safe in patients with epilepsy, supporting a positive outlook towards vaccination in this population.
Abbreviations
COVID-19
coronavirus disease 2019
SARS-CoV-2
severe acute respiratory syndrome coronavirus 2
PRISMA
Systematic Review and Meta-Analysis
EMBASE
Excerpta Medica database
AHRQ
Agency for Healthcare Research and Quality
ORs
odds ratios
DS
Dravet syndrome
DSUK
National Hospital for Neurology and Neurosurgery
CCE
Chalfont Centre for Epilepsy
ILAE
International League Against Epilepsy
HRQOL
Health-related quality of life
ASM
antiseizure medication
1. Introduction
As of 30 April 2022, coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection had affected more than 500 million confirmed cases and over six million fatalities worldwide [1]. The increased infectivity of the delta and omicron mutations of the SARS-CoV-2 exacerbates the public panic [2], [3]. Vaccines remain the most promising approach for controlling COVID-19 pandemic and reestablishing pre-pandemic routines.
Emerging COVID-19 vaccines protects from symptomatic SARS-CoV-2 infection. Neurologic complications of COVID-19 vaccines have been reported, including strokes, cranial neuropathies, peripheral neuropathies, acute disseminated encephalomyelitis, transverse myelitis, and acute idiopathic demyelinating polyneuropathy [4], [5], [6], [7], [8], [9], [10], [11], [12]. There are substantial concerns regarding the potential risks after vaccination in those with preexisting neurologic disorders. Epilepsy is one of the most common neurological disorders, affecting more than 70 million people worldwide [13]. A previous study suggested that patients with epilepsy were at a higher risk of experiencing unfavorable COVID-19 outcomes [14]. Taken the widespread of the COVID-19 pandemic, it is urgent to know the benefits and risks of vaccination for patients with epilepsy. To our knowledge, evidences of the COVID-19 vaccination coverage, willingness, and safety profiles in patients with epilepsy were limited. In this systematic review and meta-analysis, we aimed to summarize the currently available evidences regarding the COVID-19 vaccination coverage, willingness or hesitancy in patients with epilepsy. Moreover, we systematically reviewed the safety and tolerability of COVID-19 vaccines among patients with epilepsy.[…]
