Archive for December, 2022
[ARTICLE] Stroke Recovery During the COVID-19 Pandemic: A Position Paper on Recommendations for Rehabilitation – Full Text
Posted by Kostas Pantremenos in COVID-19, REHABILITATION on December 31, 2022
Abstract
Health care delivery shifted and adapted with the COVID-19 pandemic caused by the novel severe acute respiratory syndrome coronavirus 2. Stroke care was negatively affected across the care continuum and may lead to poor community living outcomes in those who survived a stroke during the ongoing pandemic. For instance, delays in seeking care, changes in length of stays, and shifts in discharge patterns were observed during the pandemic. Those seeking care were younger and had more severe neurologic effects from stroke. Increased strain was placed on caregivers and public health efforts, and community-wide lockdowns, albeit necessary to reduce the spread of COVID-19, had detrimental effects on treatment and recommendations to support community living outcomes. The American Congress of Rehabilitation Medicine Stroke Interdisciplinary Special Interest Group Health and Wellness Task Force convened to (1) discuss international experiences in stroke care and rehabilitation and (2) review recently published literature on stroke care and outcomes during the pandemic. Based on the findings in the literature, the task force proposes recommendations and interdisciplinary approaches at the (1) institutional and societal level; (2) health care delivery level; and (3) individual and interpersonal level spanning across the care continuum and into the community.
Statement of purpose
The COVID-19 pandemic caused by the novel severe acute respiratory syndrome (SARS) coronavirus (CoV) 2 posed unprecedented challenges to health care systems around the world. It is expected that the fallout from the COVID-19 pandemic will directly affect people who experience stroke during this time. The Health and Wellness Task Force within the American Congress of Rehabilitation Medicine Stroke Interdisciplinary Special Interest Group is concerned that during the ongoing pandemic, fewer people are seeking stroke care, and more people with stroke are living with the effects of untreated stroke or being discharged with minimal rehabilitation or without critical early and intensive rehabilitation that is recommended for improving stroke outcomes.1 The purpose of this position article is to describe ongoing challenges and opportunities to support the short- and long-term needs of people surviving stroke during the COVID-19 pandemic. The task force proposes potential solutions across the care continuum to support a multilevel and interdisciplinary approach that addresses this major public health problem.
Rationale for position paper
Enduring a stroke during the pandemic
Before the COVID-19 pandemic, stroke was widely regarded as a leading global cause of disability2, 3, 4 and the second leading cause of death (11.6% of global mortality).5 Despite advancements in medical interventions that increased stroke survival, disparities in stroke mortality and disability were prevalent, partly because of differences in country income and medical care quality (eg, cost, access, availability).3 The COVID-19 pandemic presented an additional risk factor for stroke: COVID-19 infection. While there is no exact mechanism linking COVID-19 to stroke, vascular symptoms associated with COVID-19 such as hypercoagulability and arterial and venous thrombosis are believed to be contributing factors to increased risk of stroke.6, 7 Other coronavirus respiratory syndromes of the same nature including the SARS-CoV-1 and Middle East Respiratory Syndrome coronavirus were also related to increased incidence of acute ischemic stroke.7 Further, people with stroke risk factors (eg, diabetes, smoking) have an increased COVID-19 mortality rate, possibly because of the same mechanisms attributed to stroke risk, such as large expression of angiotensin-converting enzyme 2 cell receptors for binding to SARS-CoV-2.8
Common deficits after stroke include impaired motor function; impaired ability to carry out activities of daily living; cognitive impairments in memory, language, attention, and executive function; and affected mood, sensation, and perception.9 10 Stroke attributed to the SARS-CoV-2 infection can cause greater severity of stroke,11 potentially leading to prolonged acute care and rehabilitation.12 Natural recovery of broad stroke-related impairments often occurs with haste within the first 6 months post stroke and then tends to plateau, although this may vary for cognitive, physical, and sensory-perceptual impairments.13 It is difficult to predict individual recovery because sequelae are multifaceted across multiple domains. As such, rehabilitation clinicians rely on their own judgment as to when to end rehabilitation post stroke.13 The long-term effects and recovery trajectory for individuals with simultaneous SARS-CoV-2 infection and stroke is unknown.
Stroke care
Before the COVID-19 pandemic, patients with stroke symptoms received hyperacute and acute treatment at the nearest specialist stroke unit, primary stroke center, or comprehensive stroke center.14 After acute treatment, the patient entered 1 of 2 main pathways for poststroke rehabilitation: (1) subacute rehabilitation (eg, inpatient rehabilitation, skilled nursing facility); or (2) community rehabilitation, normally delivered via an outpatient facility or in the patient’s home.15
A large-scale RCT of working-aged survivors of stoke across the UK, Australia, and Southeast Asia found that within 3 months post stroke, 67% of survivors of stroke received either inpatient or community rehabilitation, and only 8% of those were still receiving rehabilitation 12 months post stroke.15Those with milder strokes had the highest rates of receiving no rehabilitation (40%), followed by a lower proportion of those with moderate strokes (12%) and severe strokes (4%) who required no rehabilitation.15
During the pandemic, regions with high incidence of COVID-19 were forced to reorganize health care services. This included implementation of triage systems, separating patients with confirmed or suspected COVID-19 from patients without COVID-19 and redeploying health care professionals to the frontline to deal with the influx of patients with COVID-19.16, 17, 18
Resources and clinicians were spread across usual clinical care and COVID-19 specific care, increasing the potential short- and long-term negative consequences of high stress and burnout.19
An overwhelmed health care system, attributed to reassignment of staff or beds, increased patient admissions without adequate staffing, and increased resource strain, likely led to care and service limitations.20
Overarching rationale
Given the substantial number of adults enduring stroke annually, it is necessary to understand and address their needs during the ongoing COVID-19 pandemic. While it is well-documented that interdisciplinary stroke rehabilitation can enhance outcomes after stroke, the substantial shift in health care delivery during the COVID-19 pandemic may have major effects on short- and long-term outcomes. Researchers must further examine stroke outcomes related to the COVID-19 pandemic. Practitioners must be prepared to identify problems and challenges among this population to address the fallout the pandemic has imparted on a generation of survivors of stroke.[…]
[WEB] What Are Generalized Seizures?
Posted by Kostas Pantremenos in Epilepsy on December 31, 2022
Medically reviewed by Evelyn O. Berman, M.D.
Article written by Liz Aulino, Ph.D.
Generalized seizures are a type of epilepsy that affects up to 40 percent of people with epilepsy. Generalized seizures occur when abnormal electrical activity occurs simultaneously across both hemispheres of the brain. This seizure activity is what makes generalized onset seizures different from other seizure types. Focal seizures, or partial seizures, occur only on one side of the brain.
Types of Generalized Seizures
Generalized seizures can take different forms, each with their own set of signs and symptoms. The differences in symptoms in generalized seizures are caused by the location in the brain where the abnormal electrical activity is happening.
To determine the type of seizure a person is experiencing, a doctor investigates a person’s brain waves following the seizure event, often using an electroencephalogram (EEG). Unusual waves or spikes in the brain’s activity can provide helpful clues as to the type of seizure. There are several types of generalized seizures, grouped by the International League Against Epilepsy into two categories — motor and nonmotor.
Motor Seizures
Motor seizures include symptoms that affect movement.
Generalized Tonic-Clonic Seizures
Generalized tonic-clonic (GTC) seizures used to be called grand mal seizures. A GTC seizure consists of several phases, which can vary between individuals.
The prodromal phase of a seizure happens before the seizure begins. In this phase, a person may experience a distinct feeling they associate with seizures, or a warning sign they’ve learned over time. A person with epilepsy may experience mood swings, headache, or confusion. Only 20 percent of people with epilepsy who experience GTC seizures go through this phase.
An aura is often the first indication of a GTC seizure for many people with epilepsy. Like the prodromal phase, not everyone experiences an aura. Those who have aura may report symptoms such as numbness, loss of vision, a bitter taste, or other sensations, depending on how the brain is affected.
Auras occur in the first part of the ictal phase, or the time from the beginning of a seizure until the end of the seizure. During the ictal phase, a person can experience muscle contractions, twitching, loss of bowel or bladder control, and memory lapses, among many other symptoms. GTC seizures are named after these characteristic muscle contractions — “tonic” means stiffening, and “clonic” means jerking movements.
The time period following a GTC seizure is called the postictal phase. Some people with epilepsy recover quickly. For others, the postictal phase can last as long as several days. A person might experience symptoms like soreness, nausea, or headaches, as well as sadness, memory loss, or confusion during the postictal phase. The length of the postictal phase and the types of symptoms experienced can differ depending on how the brain was impacted during the seizure.
Tonic Seizures
During a tonic seizure, a person’s muscles suddenly stiffen or tighten. Then, the person loses consciousness. Their back arches because the muscles in their arms, legs, and chest tighten, and their eyes roll back in their head. The tightened chest muscles can make it difficult to breathe during a tonic seizure. This can cause a person’s lips or face to turn blue.
Clonic Seizures
During a clonic seizure, a person’s muscles twitch or rhythmically jerk. This usually affects the arms and legs, but muscles in the neck and face may also be affected. Generally the jerking will slow before it stops completely. As the seizure subsides, it is common for the person experiencing symptoms to let out a deep sigh.
Myoclonic Seizures
Myoclonic seizures can occur in clusters. They feature a rhythmic jerking motion as muscles rapidly tighten, then release.
Infants ages 3 to 12 months can develop a type of myoclonic epilepsy called infantile spasms. During this kind of seizure, an infant’s arms fly outward as their knees and back bend. Infantile spasms happen in a series or cluster, unlike colic cramps or reflux.
Nonmotor Seizures
Nonmotor seizures lack symptoms that affect movement. Instead, these seizures can cause changes in cognition, emotion, or sensation.
Absence Seizures
Absence seizures, once called petit mal seizures, are usually short and last less than 10 seconds. During an absence seizure, a person stops what they are doing and goes blank. They may look like they are daydreaming or staring off into space. The person will likely remain upright. Afterward, they will have no memory of what happened.
Absence seizures can occur multiple times a day. Due to their short duration and subtle presentation, people nearby might not even notice the seizure.
Atypical absence seizures tend to be longer, come on slower, and have more symptoms. An atypical absence seizure may last 20 seconds or more. These seizures may also feature facial spasms, eyelid fluttering, or lip-smacking.
Atonic Seizures
Atonic seizures, sometimes called drop attacks, cause a sudden loss of muscle tone. A person experiencing an atonic seizure will go limp, causing them to suddenly fall down if standing or drop their head. The person experiencing the atonic seizure will remain unresponsive until the seizure is over. Atonic seizures are also associated with a rare type of epilepsy, Lennox-Gastaut syndrome, that develops between the ages of 3 and 5.
What Causes Generalized Seizures?
Generalized seizures can occur in people with and without epilepsy. Someone who experiences two or more generalized seizures that are not the result of a fever may be diagnosed with generalized epilepsy.
Generalized epilepsy can be caused by a number of factors, such as damage to the brain or genetics. A person with epilepsy can also develop the condition over time as the result of a brain tumor, stroke, or infectious diseases like meningitis or encephalitis.
Risk factors for generalized epilepsy include:
- A family history of seizures
- A head injury
- Age — a person is more likely to develop epilepsy under the age of 20 or over 65
- A history of having seizures as a child
Read more about causes of epileptic seizures.
Treatment Options for Generalized Seizures
There is no treatment that is effective for all types of generalized seizures. However, many treatments are available for generalized seizures. These include medications, specialized diets, and surgery. Treatments are matched to the type of seizure, where in the brain the seizure originates, and the seizure’s root cause.
Antiepileptic Drugs
Many people can control their symptoms with antiepileptic drugs (AEDs). These medications are thought to work by reducing the electrical activity in the brain that causes epileptic seizures. Depending on the type of seizure, a doctor may prescribe a broad- or narrow-spectrum AED. Broad-spectrum AEDs are effective against more than one seizure type, while narrow-spectrum AEDs are used to treat specific types. For example, absence seizures are frequently treated with a narrow-spectrum AED.
In addition to AEDs, other medications can be used to treat seizures. Sedatives like barbiturates or benzodiazepines are sometimes prescribed. Lennox-Gastaut syndrome is often treated with the benzodiazepine clonazepam (Klonopin).
Diet Changes
Although the majority of those who experience generalized seizures can control their symptoms with medication, some epilepsy may be resistant to traditional treatments. If generalized seizures cannot be controlled with medication, a doctor may prescribe diet modifications.
The ketogenic diet is used to treat children with treatment-resistant epilepsy. This high-fat, low-carbohydrate diet increases ketones in the blood, which helps reduce seizures for some children. A similar, less extreme version of this diet may be prescribed to adults with treatment-resistant epilepsy.
Surgery
In extreme cases where neither medication nor diet has improved seizure activity — or in cases where a person experiences severe, frequent seizures that are life-threatening — a doctor may recommend epilepsy surgery. Surgery for treatment-resistant epilepsy removes the part of the brain where seizures originate. In some cases, this may be a brain lesion or tumor. Depending on the type of seizure, a frontal or temporal lobe resection may be appropriate.
For people with drug-resistant generalized seizures, the most common surgical intervention is a corpus callosotomy. This procedure removes the part of the brain that joins the two hemispheres. This treatment works best in people with atonic, atypical absence, tonic, and tonic-clonic seizures.
Read more about treatments for epileptic seizures.
Talk With Others Who Understand
MyEpilepsyTeam is the social network for people with epilepsy and their loved ones. On MyEpilepsyTeam, more than 105,000 members come together to ask questions, give advice, and share their stories with others who understand life with epilepsy.
Are you living with generalized onset seizures? Share your experience in the comments below, or start a conversation by posting on your Activities page.
[ARTICLE] Clinical Effectiveness of Non-Immersive Virtual Reality Tasks for Post-Stroke Neuro-Rehabilitation of Distal Upper-Extremities: A Case Report – Full Text
Posted by Kostas Pantremenos in Paretic Hand, Virtual reality rehabilitation on December 29, 2022
Abstract
A library of non-immersive Virtual Reality (VR) tasks were developed for post-stroke rehabilitation of distal upper extremities. The objective was to evaluate the rehabilitation impact of the developed VR-tasks on a patient with chronic stroke. The study involved a 50-year-old male patient with chronic (13 month) stroke. Twenty VR therapy sessions of 45 min each were given. Clinical scales, cortical-excitability measures, functional MRI (fMRI), and diffusion tensor imaging (DTI) data were acquired pre-and post-therapy to evaluate the motor recovery. Increase in Fugl-Meyer Assessment (wrist/hand) by 2 units, Barthel Index by 5 units, Brunnstrom Stage by 1 unit, Addenbrooke’s Cognitive Examination by 3 units, Wrist Active Range of Motion by 5° and decrease in Modified Ashworth Scale by 1 unit were observed. Ipsilesional Motor Evoked Potential (MEP) amplitude (obtained using Transcranial Magnetic Stimulation) was increased by 60.9µV with a decrease in Resting Motor Threshold (RMT) by 7%, and contralesional MEP amplitude was increased by 56.2µV with a decrease in RMT by 7%. The fMRI-derived Laterality Index of Sensorimotor Cortex increased in precentral-gyrus (from 0.28 to 0.33) and in postcentral-gyrus (from 0.07 to 0.3). The DTI-derived FA-asymmetry decreased in precentral-gyrus (from 0.029 to 0.024) and in postcentral-gyrus (from 0.027 to 0.017). Relative reduction in task-specific performance metrics, i.e., time taken to complete the task (31.6%), smoothness of trajectory (76.7%), and relative percentage error (80.7%), were observed from day 1 to day 20 of the VR therapy. VR therapy resulted in improvement in clinical outcomes in a patient with chronic stroke. The research also gives insights to further improve the overall system of rehabilitation.
1. Introduction
Residual upper-arm disabilities are common morbidities in the chronic phase of recovery, affecting more than 66% of patients with stroke [1]. The literature suggests the requirement of intensive practice to facilitate functional recovery in the chronic phase [2]. However, factors such as lack of objective assessment, associated clinical burden and boredom highly limit the effectiveness of traditional rehabilitation [3]. In recent years, Virtual Reality (VR)-assisted rehabilitation has emerged as a supplementary approach to address some of the limitations associated with traditional physiotherapy [4,5]. Post-stroke rehabilitation of distal upper extremities is comparatively slower and requires intensive targeted practice to conduct Activities of Daily Living (ADL) [6]. However, limited literature exists to support targeted VR-based rehabilitation of distal upper extremities [7]. Furthermore, the exact neurophysiological aspects showing enhanced post-stroke recovery at the neuronal level are still unclear [8]. In our previous study, a library of VR tasks specific to distal-joint rehabilitation was developed, and task-specific outcome metrics were validated with forty healthy subjects and two patients with stroke [9]. In this study, we present the case of a 50-year-old male patient with 13-month chronic stroke who participated in VR therapy and the associated functional and neuronal changes observed in response to the therapy. The primary objectives of this study were to evaluate the efficacy of the developed VR tasks and to investigate the neurophysiological behavior supporting post-stroke motor recovery in response to the VR therapy during the chronic phase.
2. Case Description
The study was approved by the Institutional Review Board (IRB) at All India Institute of Medical Science (AIIMS), New Delhi, India, under protocol-number IEC-229/11.4.2020. The patient provided written informed consent before enrollment in this study.
2.1. Subject
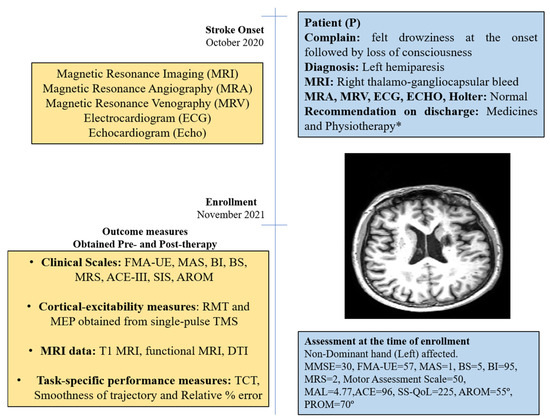
The patient was a 50-year-old right-handed male (henceforth, referred as “P”); he was well educated and was a lawyer by profession. He had an incidence of right thalamo-gangliocapsular-bleed in October 2020 (Supplement Figure S1). Additional clinical-presentation details are provided in the Supplementary Materials (Section S1). He had no history of substance abuse, such as consuming tobacco or alcohol, but experienced hypertension in the past 10 years and diabetes for past 1 year. After onset of stroke, he was admitted to a local hospital and discharged after 14 days for rehabilitation management at home. He underwent supervised home-based physiotherapy after 3 months after stroke-onset (see Supplementary Materials). Assessment scores at enrollment are given in Figure 1.
[BLOG POST] Practice mindfulness to optimize well-being after stroke or brain injury
Posted by Kostas Pantremenos in Cognitive Rehabilitation on December 29, 2022

Practice mindfulness to optimize well-being after stroke or brain injury
by Kate Ying
Mindfulness is a valuable skill that has the ability to enhance your emotional and physical well-being by lowering stress levels and improving cognitive function. These benefits are especially valuable following such a life-changing and challenging event as a stroke or traumatic brain injury.
This post discusses what mindfulness is, how it is beneficial for mental health and cognition, and how to incorporate it into your recovery journey.
What is mindfulness?
Mindfulness has become something of a buzzword recently, but the term actually describes a simple concept. Mindfulness is the state of being fully present and calmly aware of the thoughts, emotions, and sensations you experience from one moment to the next. The goal is to do this curiously and without judgment or attachment to any particular feelings or outcomes.
We all have the potential to be mindful, but certain techniques can help us intentionally activate our inner mindful selves.
Top 4 reasons to practice mindfulness
Studies have shown that becoming more mindful is a simple but powerful way to improve your sense of well-being and sharpen your cognitive abilities. Some specific benefits include:
- Lowered anxiety: Dedicated mindfulness practices can help significantly decrease feelings of anxiety, leading to improved psychological and overall health (Carmody & Baer, 2007).
- Reduced stress: Even a brief mindfulness practice can similarly be an effective intervention to lower psychological stress, which in turn can improve general health. This is especially important if you are recovering from an acute health event, such as a stroke or traumatic brain injury (Creswell et al., 2014).
- Decreased pain and fatigue: Mindfulness practices have been effective in studies at reducing pain and improving mood in survivors of traumatic brain injury (McMillan et al., 2002). Furthermore, survivors of stroke and traumatic brain injury who took a Mindfulness-Based Stress Reduction course reported experiencing decreased mental fatigue (Johansson et al., 2012).
- Improved cognition and communication: Mindfulness practice has also been linked to a longer attention span, which can enhance your ability to perform demanding cognitive tasks and to communicate clearly (Jha et al., 2007). Studies have even shown that consistently meditating might physically alter areas of the brain related to cognitive and sensory processing (Lazar et al., 2005).
How can I practice mindfulness?
One of the best aspects of practicing mindfulness is that it is something anyone can do without special training or equipment. All you need is the desire and willingness to be more fully in touch with the present.
Consider starting here to tap into your inner mindful state:
- Find a quiet moment: Pick a time when you have a few minutes to yourself and will not be rushed or interrupted.
- Commit to practicing for a certain amount of time: It could be a set number of minutes that you track via a timer, or it could simply be for the full duration of a specific activity through to its natural end.
- Start slowly: You might find a mindfulness practice tiring at first, due to the concentration required. It is important to take breaks and go slowly at first, starting with one to two minutes a day and working up.
- Choose your mindfulness exercise: You might try to mindfully taste a sour lemon candy, paying attention to how the wrapper sounds and noting the sensations in your body as the candy melts on your tongue. Or you might decide to mindfully perform a mundane daily activity like washing the dishes, noticing the sound of running water, and the slippery texture of the soap.
Whatever you decide to do, try to do it mindfully. That means that you should try to focus with intention and curiosity on every part of your experience, including what you smell, hear, feel, or think during the practice. Try to avoid fixating on a particular outcome, such as finishing the whole candy or washing all the dishes. Instead, let each moment take you to the next.
- Acknowledge disruptions without judgment or attachment: If you find yourself getting distracted by something external, such as a loud noise, or internal, such as a thought that elicits strong emotion, acknowledge the interruption without judgment of yourself or others. Then, detach yourself from the distraction, gently turning your mind back to the exercise. You might visualize an overwhelming thought or emotion as a leaf floating along a stream, moving toward you and then away again.
- Be patient with yourself: Remember that, as with anything else, the process of becoming more mindful is a gradual one. You might experience impatience, boredom, or frustration as you begin practicing this skill.
Additional supports:
If it feels intimidating to begin a mindfulness practice completely on your own, you might consider the following resources:
- Seek social support: Friends, family, or mental health professionals can be a valuable source of encouragement if you choose to share your mindfulness journey with them. They might remind you to do a daily practice or check-in to ask how you are feeling afterward.
- App-based guided meditations: There are a variety of apps for the iOS and Android operating systems that offer guided mindfulness meditations. Popular apps available for free include Insight Timer, UCLA Mindful, and Smiling Mind.
- Join a local meditation group: Usually, an instructor will lead the group through a live guided meditation. These groups can be a great way to build community into your practice.
- Enroll in a Mindfulness-Based Stress Reduction (MBSR) course: MBSR courses lead students through an intensive, 8-week mindfulness curriculum. They usually involve a substantial time and monetary commitment. Many clinical studies on the benefits of mindfulness have been based on MBSR programs (A.K. and S.K., 2011).
Over time, entering a state of mindfulness will become a more seamless part of your everyday experience. You might continue practicing specific mindfulness techniques or doing daily meditation, or your practice might evolve to integrate more fully with your daily activities. Either way, hopefully, it will not take long before you start to notice the benefits of mindfulness practice on your mental and physical health as you progress in your recovery from a stroke or traumatic brain injury.
References and Further Resources
Creswell, J. D., Pacilio, L. E., Lindsay, E. K., & Brown, K. W. (2014). Brief mindfulness meditation training alters psychological and neuroendocrine responses to social evaluative stress. Psychoneuroendocrinology, 44, 1–12. https://pubmed.ncbi.nlm.nih.gov/24767614/
Carmody, J., & Baer, R. A. (2007). Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. Journal of Behavioral Medicine, 31(1), 23–33. https://link.springer.com/article/10.1007/s10865-007-9130-7
Jha, A.P., Krompinger, J., & Baime, M.J. (2007). Mindfulness training modifies subsystems of attention. Cognitive, Affective, & Behavioral Neuroscience, 7(2), 109–119. https://link.springer.com/article/10.3758/CABN.7.2.109
Johansson, B., Bjuhr, H., & Rönnbäck, L. (2012). Mindfulness-based stress reduction (MBSR) improves long-term mental fatigue after stroke or traumatic brain injury. Brain Injury, 26(13-14), 1621–1628. https://pubmed.ncbi.nlm.nih.gov/22794665/
Lazar, S. W., Kerr, C. E., Wasserman, R. H., Gray, J. R., Greve, D. N., Treadway, M. T., … Fischl, B. (2005). Meditation experience is associated with increased cortical thickness. NeuroReport, 16(17), 1893–1897. https://pubmed.ncbi.nlm.nih.gov/16272874/
McMillan, T., Robertson, I. H., Brock, D., & Chorlton, L. (2002). Brief mindfulness training for attentional problems after traumatic brain injury: A randomised control treatment trial. Neuropsychological Rehabilitation, 12(2), 117–125. https://www.tandfonline.com/doi/abs/10.1080/09602010143000202
Niazi, A. K., & Niazi, S. K. (2011). Mindfulness-based stress reduction: a non-pharmacological approach for chronic illnesses. North American journal of medical sciences, 3(1), 20–23. https://www.najms.org/article.asp?issn=1947-2714;year=2011;volume=3;issue=1;spage=20;epage=23;aulast=Niazi
Kate Ying is an intern at Constant Therapy Health. She is a student at Columbia University.
[Book Chapter] Hand Gesture Controlled Game for Hand Rehabilitation – Google Books
Posted by Kostas Pantremenos in Books, Paretic Hand, REHABILITATION, Video Games/Exergames on December 28, 2022

Hand Gesture Controlled Game for Hand Rehabilitation
Table of Content
Contents
| PeerReview Statements | 1 |
| Designing User Interface for an ElderlyMuslimFriendly Mobile Application | 3 |
| Comparison of Machine Learning Models for IoT Malware Classification | 15 |
| SafeTravelApplication with Blockchain Technology | 29 |
| Location Profiling for RetailSite Recommendation Using Machine Learning Approach | 48 |
| A Primary Study on the Performances and Techniques | 68 |
| A Case Study Using Machine Learning Techniques for Prediction of House Prices in WP Malaysia | 79 |
| Identifying Demographic Factors Attributed to the Infection Rate of Covid19 in Malaysia | 92 |
| Colourassisted PCB Inspection System with Hardware Support for Realtime Environment | 313 |
| A Residual CNN Model for ICD Assignment | 331 |
| Virtual Reality Game for Physical Rehabilitation | 342 |
| Preliminary Study on Shadow Detection in DroneAcquired Images with UNET | 357 |
| Mediating Schema Ontology for Linked Open Data Cloud Integration Using BottomUp Schema Mapping | 369 |
| QR Steganography for Information Hiding of Patient Record | 392 |
| A TwoStage Classification Chatbot for Suicidal Ideation Detection | 405 |
| Heart Disease Classification | 413 |
| Machine Learning Approaches to Intrusion Detection System Using BOTPE | 104 |
| Email Plugin Suite for kResilient IdentityBased Encryption and Searchable Encryption | 120 |
| Classification of Emotion Stimulation via Iranian Music Using Sparse Representation of EEG Signal | 133 |
| ICABased Sensorimotor Rhythms Detection in ALS Patients for BCI Applications | 145 |
| A Hybrid Unsupervised Mining Approach for Customer Segmentation in B2C eCommerce | 156 |
| A Digital Rights Management System for Media Content Consumption | 171 |
| A Review | 182 |
| CNNBased Traffic Sign Recognition | 195 |
| Hand Gesture Controlled Game for Hand Rehabilitation | 205 |
| A Review on Industrial Revolution 40 IR40 Readiness Among Industry Players | 216 |
| Technology Usage for Sustainable Health and Wellbeing in Ecommerce Throughout the COVID 19 Pandemic | 232 |
| Objectivity and Subjectivity Classification with BERT for Bahasa Melayu | 246 |
| Predictive Modelling of Student Performance in MMU Based on Machine Learning Approach | 258 |
| Face Mask Detection Using Deep Learning | 279 |
| Traffic Light Recognition Assistance for Colour Vision Deficiency Using Deep Learning | 289 |
| Research Framework and Design of Incorporation of Conversational Agent in Mathematics Learning | 301 |
| A Review and Analysis of Tools Used from 2018 till 2022 in Requirements Engineering | 424 |
| Automatic Face Mask Detection and Violation of Social Distancing Application | 439 |
| A Hybrid Automated Essay Scoring Using NLP and Random Forest Regression | 448 |
| Machine Learning Regression Models to Predict Particulate Matter PM25 | 458 |
| A Review | 469 |
| Performance Analysis of OAMBased Advanced Symbol Modulation Schemes for OFDM Over FSO System | 480 |
| Comparison of Word Embeddings for Sentiment Classification with Preconceived Subjectivity | 488 |
| Autoencoders with Reconstruction Error and Dimensionality Reduction for Credit Card Fraud Detection | 503 |
| Lossless ECG Signal Compression Using Nonlinear Predictor and ASCII Character Encoding | 513 |
| Comparison of Plain and Dense Skip Connections on UNet Architecture for Change Detection | 524 |
| Underwater Image Semantic Segmentation with Weighted Average Ensemble | 533 |
| Dynamic Hand Gesture Recognition Based on Deep Learning for Muslim Elderly Care | 544 |
| Comparison of Deep Learning Methods for Underwater Image Enhancement | 558 |
| Integration of Pedagogical Agent in Learning | 572 |
[WEB] Why It’s Not a Sign of Weakness to Ask for Help
Posted by Kostas Pantremenos in REHABILITATION on December 28, 2022
 BETTER LIFE
BETTER LIFE
It’s a common misconception that it’s a sign of weakness to ask for help. However, knowing when you need an assist is a sign of strength. It is one of the hardest things for people to do, showing courage and a willingness to admit vulnerability.
Asking for help doesn’t mean that you are dependent on anyone. Instead, it shows a willingness to grow and learn as you gain knowledge from those who know more about it than you do. There are many benefits to asking for help, proving that it’s not a sign of weakness.
You can’t know everything, and you’re stronger in some areas than other people are. Everyone has different strengths and weaknesses, so utilizing them can improve performance. Not admitting when you need a little support is the true sign of weakness as you won’t deliver the best effort.
Don’t miss out on an opportunity to develop your skills and get help in areas you aren’t an expert in. It’ll save you time, help you learn, and offer many other benefits. Understanding why it’s not a sign of weakness can help give you the courage to speak up next time you need something.
Why It’s Not a Sign of Weakness to Ask for Help
1. It’s a Sign of a High Performer
Research shows that high performers are more likely to ask their colleagues for help. They want to improve and know that asking for advice can boost personal performance. You can’t learn something new if you never ask someone to show you, so it’s not a sign of weakness.
On the other hand, people who don’t ask for help tend to be low performers. They assume they already know everything and that their performance levels are high, although that might not be accurate.
2. It Helps You Develop a Growth Mindset
When you receive help from others, it can help you develop a growth mindset. It proves that making an effort and looking for a solution allows you to learn new information. When you continually gather information, it helps you think long-term with a growth mindset.
https://imasdk.googleapis.com/js/core/bridge3.549.0_en.html#goog_1747596763
3. It Improves Your Mental Health
Asking for help can connect you to others, allowing you to learn new things. Feeling connected to others and learning new things both improve your mental health. You’ll feel better knowing that you have people who support you and that you can continue learning.
Additionally, asking for help improves your mental health because it allows you to make time for yourself. When you have help with tasks, you’ll have more time to care for your needs and do things you enjoy.
4. It Strengthens Bonds
When you ask for help, it encourages bonds with the person who helps you. It forces you to put your trust in others, allowing them to trust you, too. Expressing the need for support encourages ongoing collaboration or mentorship, enabling you to grow.
It helps if you ask someone for help that you can help in return if the need arises. Plus, studies show that asking someone for assistance indicates that you like them, promoting a relationship and healthy support system.
5. It Allows You to Reassess Your Priorities
You’ll experience a time when you must reassess your priorities in life, which isn’t always an easy thing to do. However, reassessing gives you the chance to focus on what matters most to you in life. By asking for help, you can decide which tasks to delegate and which to keep.
Asking for help allows you to improve your life. When you feel better and happier, you’ll perform better in all areas. It will make you stronger and let you experience optimism and excitement.
6. It Encourages Others to Ask for Help
Sometimes people don’t ask for help because no one else has asked yet. They often wait until someone else asks first, and you can be the leader who paves the way. It shows that you are open to asking for and receiving a hand up from others, creating an environment for growth.
7. You Learn About Other People’s Passions and Strengths
Asking for help allows you to get to know people better. You’ll see their strengths and talents, allowing other people to shine. If your strengths lie in other areas, you can produce better work by accepting help from someone.
When you know what someone’s strengths are, you’ll know who to turn to for collaboration. Producing the best work is always more important than controlling every detail, so don’t hesitate to reach out.
8. It Improves Resilience
When you ask for help, it makes you feel good as you learn and develop in that particular area. It also shows that you have supportive people in your life, making you feel even better. When you feel good, you’ll experience hope and optimism, helping you become more resilient.
9. It Encourages Teamwork
Working as a team improves an individual’s work ethic, promoting enhanced effort. Even if the other person helps you with something unrelated to what you’re doing, it improves overall performance. By asking for help, you not only have less work, but you also work more effectively on your other tasks.
10. It Allows Others to Relate to You
Asking for help doesn’t show that you are weak but allows others to relate to you. It shows that you are imperfect like everyone else around you. When you aren’t afraid to hide when you need help, the people around you will feel at ease.
11. You Give the Gift of Happiness
When you ask someone for a hand, it will likely make them happy because they’re able to give you something. While the person might not physically give anything, helping you out will still trigger their body to release oxytocin. Oxytocin is a hormone that promotes happiness and encourages bonding, too.
12. It Changes Your Mindset
Asking for help allows you to change your mindset and stop assuming you have to do everything yourself. You are worthy of receiving assistance from others, and acknowledging the fact will help you open up time in your life. It gives you the time and opportunity to do things that empower you to grow.
You can ask for help with things at home, work, or anywhere else. It allows you to stay sane as you go through your daily tasks. You don’t have to put everything on yourself, and requesting some support will make you recognize that you’re not alone.
13. It Helps You Maintain Energy and Focus
By asking for help, you allow yourself to stay focused and energetic. When you share a task with others or have someone working alongside you, it makes the experience more fun. You might not do anything differently, but you’ll enjoy the situation more when you aren’t alone. The more relaxed you are, the more you can maintain energy and focus.
14. It’s a Good Character Trait
The good people in your life will respect you for asking for an assist. It’s a good character trait because it shows courage and a willingness to learn. When you express vulnerability by asking for help, it allows others to see you positively.
If anyone in your life thinks you’re weak for asking for help, they likely aren’t someone you want around anyway. The people who matter will like that you want to improve yourself and will be more than willing to give you a boost.
15. It Decreases Procrastination
Asking for help can encourage you to stop procrastinating. You won’t put things off when someone is there to help because you don’t want to waste their time. The task will also seem more manageable when you have someone to work alongside you or teach you something new.
Three Easy Tips For Asking for Help
Now that you know why it’s not a sign of weakness to ask for help, it’s time to start asking. Don’t miss an opportunity to get help when it’s available by using the following tips:
1. Change Your Expectations
Don’t beat yourself up by believing that you should do everything alone. You don’t have to do it on your own if someone is willing to give you a hand. Change your expectations and remember that it’s okay to ask for help and not know everything.
2. Don’t Make It Hard to Help
Before you ask for help, think about who you’re asking. You’ll want to ask the right person to help you, so consider their strengths ahead of time. Make sure you ask someone who can do the task and won’t make you feel bad about asking.
3. Ask Directly
Don’t drop hints or wait around hoping for someone to offer their assistance. Instead, be direct and clearly say what you need help with. Tell them what you need, how you want it done, and when you need it right from the start.

Final Thoughts on Reasons Why It’s Not a Sign of Weakness to Ask for Help
Many people falsely believe that asking for help is a sign of weakness. However, asking for a hand-up indicates a strong and courageous person willing to learn from their peers and superiors. It increases resiliency and promotes bonding, too.
Once you start requesting assistance, your mindset will shift, and you can re-prioritize your life. You’ll find meaning in your tasks and experience improved job performance while bonding with those around you.
While asking for help isn’t always easy, you’ll get better at it the more often you do it. You’ll quickly see the benefits of getting support from those around you, and your life will improve.
[Abstract] A Review on Soft Hand Rehabilitation Robot
Posted by Kostas Pantremenos in Paretic Hand, Rehabilitation robotics on December 24, 2022
Abstract
Background: In China, there are more than 2 million patients with hand function impairment caused by trauma and stroke each year. Since the hand is an important sensory and motor organ of the human body, the loss of hand function seriously affects people’s daily activities and work. The current hand function rehabilitation robots are mainly rigid. The rigid robot has the problems of fixed rehabilitation track, high rigidity, and poor comfort. To solve this series of problems, soft hand function rehabilitation robots have been vigorously developed.
Objective: To introduce the classification, advantages and disadvantages, and development trend of existing soft hand rehabilitation robots. To provide for other researchers to understand its development status and future development trends.
Methods: The various products and patents of soft hand rehabilitation robots are summarized, and the structural features, merits, and demerits of typical soft hand rehabilitation robots are introduced.
Results: By analyzing a variety of soft hand function rehabilitation robots, the characteristics and the current problems of soft hand function rehabilitation robots are determined, the development trend of soft hand function rehabilitation robots has been prospected, the current research status of soft hand function rehabilitation robots are discussed and the prospects are carried out.
Conclusion: Because the rate of increase in patients with hand function loss is much greater than that of rehabilitation physicians, many patients cannot receive timely and effective treatment. Therefore, hand function rehabilitation robots have received people’s attention. Compared with rigid rehabilitation robots, soft hand function rehabilitation robots have diverse rehabilitation trajectories, high comfort, and low rigidity, so it is very necessary to develop soft hand function rehabilitation robots. In the future, soft hand function rehabilitation robots will inevitably develop towards simplification of structure, more comfortable wearing, economical, diversified functions, better curative effect, and safer development.
[Abstract] Effect of Virtual Reality Combined with Modified Constraint-Induced Movement Therapy on Chronic Stroke Survivors
Posted by Kostas Pantremenos in Constraint induced movement therapy CIMT, Paretic Hand, Virtual reality rehabilitation on December 22, 2022
Research Objectives
To evaluate the effect of virtual reality combined with modified constraint-induced movement therapy-based upper limb training on chronic stroke survivors.
Design
Intervention. Randomized control trial, baseline two and four-week intervention.
Setting
In the Hospital setting outpatients.
Participants
Twenty-six patients both males and females with chronic stroke for more than 6 months and dysfunction in the upper limb were included in the study. The age range between 20 to 45 years was included. Convenient sampling is used for the selection procedure.
Interventions
Virtual reality Group: Treatment for 20 min 3 sessions per week for 4 weeks along with the conventional therapy. The VR protocol included using a VR headset and the games. In the Rally ball game, balls approaching the player from multiple angles are hit from a chair. The Reflex Ridge game involves hitting, and grasping obstacles while sitting in a chair. The patient played each game for 10-mins per session. Conventional therapy includes passive stretching, repetitive task-specific activities, passive, active-assisted and active ROM exercises.
Virtual reality combined with m-CIMT Group: Treatment for 20 min 3 sessions per week for 4 weeks along with the conventional therapy. The unaffected hand of the participant was restrained and then the same VR treatment (as above) was given to the participants.
Main Outcome Measures
Wolf motor function test, DASH Questionnaire, Modified Ashworth Scale, and Box & Block test.
Results
The treatment group significantly improved from the control group. Repeated measure ANOVA showed significant improvement for all the outcome measures (p< 0.005) within the 2 groups. The Independent t-test shows a significant difference in Gross motor function, patient self-report disability, and manual dexterity of upper limb (p< 0.005) and no significant difference in spasticity for MAS (p>0.005) between the groups.
Conclusions
Both treatment approaches in the control and Treatment groups are effective in managing motor functional status, spasticity level of the upper extremity, disability level, and manual proficiency of the upper extremity. Except for spasticity, both treatment approaches were found equally effective.
[WEB] Active vs Passive Exercises During Rehabilitation
Posted by Kostas Pantremenos in REHABILITATION, Spasticity on December 22, 2022
Medically reviewed by Barbara Brewer, COTA — written by Flint Rehab.

Knowing the difference between active and passive exercise can help you understand what your rehabilitation process will encompass.
In this article, you’ll learn the difference between active and passive exercise, who should use them, and how they can benefit your rehabilitation program. Use the links below to jump straight to any section:
- What Are Passive Exercises?
- Who Can Benefit from Passive Exercises?
- What Are Active Exercises?
- Who Can Benefit from Active Exercises?
- Exercises to Get You Started
What Are Passive Exercises?

Passive exercises are also known as passive range of motion (ROM) exercises; and your range of motion includes how far you can move your joints in different directions. These exercises are considered passive because you don’t exert any effort. Instead, someone helps you move your muscles and joints through their full range of motion for you.
Who Can Benefit from Passive Exercises?
Passive range of motion exercises are great for patients with hemiplegia (paralysis on one side of the body) or spasticity (stiff, tight muscles after neurological injury).
When you cannot move your limbs on your own, passive exercise allows a therapist or caregiver to move your body for you. Although passive exercise does not require effort on your behalf, the movement still carries many benefits.
For instance, movement improves blood flow in the affected areas and provides sensory stimulation to the limb. Passive stretching also helps prevent spasticity from worsening.
Passive exercises provide the most effective benefits when they are used consistently over a long period of time. Consistent repetition of therapeutic movements helps spark neuroplasticity: the mechanism the brain uses to rewire itself.
However, in order for passive exercise to induce neuroplasticity, attention must be paid to the movement. Passive exercise won’t be helpful if done while distracted or disengaged in the activity. Patients must focus on the passive movements in order to benefit from it.
What Are Active Exercises?

Active exercises involve your physical effort exerted into muscular activity.
These exercises can include active range of motion, like self-stretching, or general stroke rehabilitation exercises where you move your muscles through therapeutic movements.
When you’re doing the exercises yourself, it’s active exercise.
Movement difficulties occur after neurological injury because the brain cannot send the correct signals to the affected muscles. Rehabilitation exercise encourages the brain to rewire itself through neuroplasticity, which improves its ability to send signals to your muscles.
Neuroplasticity occurs with both passive and active exercise, but more with active exercise. Active exercise also helps with muscle strengthening. This is particularly beneficial if muscle atrophy has occurred from less daily movement.
Want 25 pages of stroke recovery exercises in PDF form? Click here to download our free Stroke Rehab Exercise ebook now (link opens a pop up for uninterrupted reading)
Who Can Benefit from Active Exercises?
Patients that struggle with hemiparesis (weakness on one side of the body) can benefit from active exercise. As long as the person has some movement of their muscles (even if the control is not substantial), they can benefit from active exercises.
When mobility is limited and restricted by conditions like spasticity, passive exercises can be done before active exercise. This helps warm up the muscles and prepare them for active use.
Patients who have some movement of their affected side, and working towards regaining more mobility, can begin with active exercises. However, ask your physical therapist what’s right for you. Some range-of-motion exercises are recommended regardless of mobility level.
Just like passive exercise, active exercise benefits patients by stimulating neuroplasticity. Frequently practicing active rehab exercises will provide the brain with the stimulation it needs to rewire itself.
Exercises to Get You Started

Now that you know the difference between active and passive exercise, do you feel like your rehabilitation regimen is properly adapted to your ability level?
If yes, that’s great! If not, then talk with your therapist. Ask her to adjust your current exercises or recommend new ones. Many therapists are eager for patients to exercise at home, because healing involves the patient taking charge of their exercises and that’s when the best results are achieved.
To help with this, at-home rehab exercise devices like FitMi home therapy help motivate patients to exercise at home. This device is therapist-approved because it adapts to your ability level, and patients can practice both passive or active exercises.
Rehab devices have higher compliance rates than written sheets of exercise, which means that patients see better results with interesting equipment. However, some patients prefer written sheets.
To help you get started, here are some free exercise guides from our rehabilitation blog:
Passive Exercise Guides:
- Paralysis Recovery Exercises for Stroke Patients
- Passive Range of Motion Exercises for Stroke Patients
Active Exercise Guides:
Select exercises and practice them consistently in order to see the best results. If you’re unsure of selecting the right exercises for you, ask your therapist for recommendations.
We hope this article helps you on the road to recovery.

