Posts Tagged gait training
[ARTICLE] Noninvasive spinal stimulation improves walking in chronic stroke survivors: a proof-of-concept case series – Full Text
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop on April 8, 2024
Abstract
Background
After stroke, restoring safe, independent, and efficient walking is a top rehabilitation priority. However, in nearly 70% of stroke survivors asymmetrical walking patterns and reduced walking speed persist. This case series study aims to investigate the effectiveness of transcutaneous spinal cord stimulation (tSCS) in enhancing walking ability of persons with chronic stroke.
Methods
Eight participants with hemiparesis after a single, chronic stroke were enrolled. Each participant was assigned to either the Stim group (N = 4, gait training + tSCS) or Control group (N = 4, gait training alone). Each participant in the Stim group was matched to a participant in the Control group based on age, time since stroke, and self-selected gait speed. For the Stim group, tSCS was delivered during gait training via electrodes placed on the skin between the spinous processes of C5–C6, T11–T12, and L1–L2. Both groups received 24 sessions of gait training over 8 weeks with a physical therapist providing verbal cueing for improved gait symmetry. Gait speed (measured from 10 m walk test), endurance (measured from 6 min walk test), spatiotemporal gait symmetries (step length and swing time), as well as the neurophysiological outcomes (muscle synergy, resting motor thresholds via spinal motor evoked responses) were collected without tSCS at baseline, completion, and 3 month follow-up.
Results
All four Stim participants sustained spatiotemporal symmetry improvements at the 3 month follow-up (step length: 17.7%, swing time: 10.1%) compared to the Control group (step length: 1.1%, swing time 3.6%). Additionally, 3 of 4 Stim participants showed increased number of muscle synergies and/or lowered resting motor thresholds compared to the Control group.
Conclusions
This study provides promising preliminary evidence that using tSCS as a therapeutic catalyst to gait training may increase the efficacy of gait rehabilitation in individuals with chronic stroke.
Trial registration NCT03714282 (clinicaltrials.gov), registration date: 2018-10-18.
Background
Stroke is the leading cause of adult-onset disability [1]. Despite many advances in gait research in the last decade, about 35% of stroke survivors fail to regain independence in performing activities of daily living due to the impaired function of their affected leg, and about 70% have gait deficits, including reduced walking speeds, asymmetrical walking patterns, and motor coordination issues [2,3,4].
Walking deficits after stroke mostly derive from a disruption of the corticospinal pathways that play an important role in transmitting sensory–motor commands [5, 6]. To address this, most interventions using non-invasive electrical pulses focus on stimulation of the motor cortex to activate dormant or new pathways [2, 7, 8]. However, while supra-spinal regions can facilitate fine locomotor control, spinal networks ultimately generate the basic locomotor pattern [9, 10]. More interestingly, a recent study using functional MRI showed increased blood-oxygen-level dependent activities in motor cortex following transcutaneous spinal cord stimulation (tSCS) in individuals with stroke [11]. Therefore, we hypothesized that tSCS would facilitate an improvement of gait after stroke. Our previous work, in collaboration with additional researchers, established anatomical and physiological changes in the spinal cord after stroke [12, 13], offering a theoretical basis for testing our hypothesis of targeting the spinal circuits for post-stroke recovery.
Recently, Moshonkina et al. reported functional improvements in post-stroke individuals after 2 weeks of tSCS with standard physical therapy, achieving the minimum clinical important differences (MCID) in the 6 min walk test and comfortable walking speed [14]. The same investigators reported immediate improvements in walking kinematics after a single tSCS session [15, 16]. Notably, however, none of the studies mentioned above investigated the effects of more than 4 weeks of training nor tried to explore the potential neurophysiological differences accompanied with gait outcomes. Consequently, it remains unclear whether tSCS can exert a lasting impact on restoration of function following a stroke.
We investigated whether tSCS combined with symmetry-focused gait training has a sustained effect on gait recovery after chronic stroke. We hypothesized that longer-term gait training (24 sessions) with tSCS would lead to greater sustained improvements in walking function compared to control treatment focused solely on gait training. Specifically, we focused on gait symmetry since such improvements can have lasting effects on balance and overall mobility of stroke survivors [6]. We also expected that gait improvements would be associated with physiological changes in muscle coordination measured from electromyography (EMG) of the paretic side, and spinal excitability determined by the spinal motor evoked responses (sMERs). […]
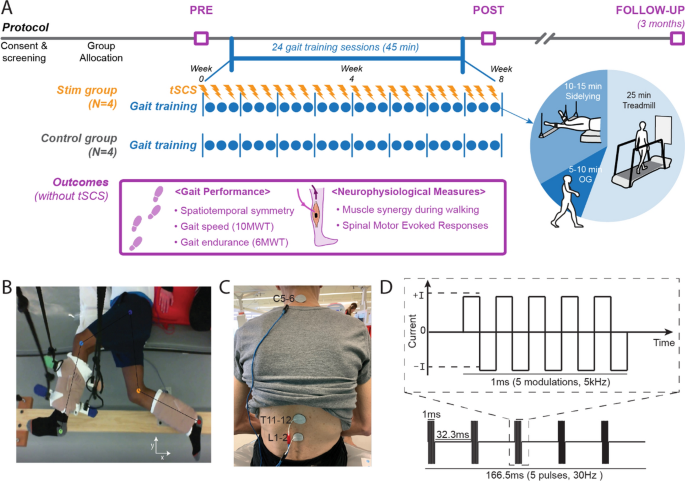
Study protocol and stimulation setup. A Overall experimental protocol. B Top–down view of position of the legs extended beyond the edge of the table and supported with vertically cables during the side-lying training of a participant (Stim 2). C tSCS delivered using surface electrodes on the skin between the C5–6, T11–12, and L1–2 spinous processes (cathode) and a surface electrode on each anterior crest (anode, not shown). D Schematic representation of biphasic pulse sequence used for tSCS. tSCS transcutaneous spinal cord stimulation, OG overground walking, 10MWT 10-m walk test, 6MWT 6-min walk test
[ARTICLE] Spatiotemporal, kinematic and kinetic assessment of the effects of a foot drop stimulator for home-based rehabilitation of patients with chronic stroke: a randomized clinical trial – Full Text
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, Tele/Home Rehabilitation on June 15, 2022
Abstract
Background
Gait disability affects the daily lives of patients with stroke in both home and community settings. An abnormal foot–ankle position can cause instability on the supporting surface and negatively affect gait. Our research team explored the ability of a portable peroneal nerve-targeting electrical stimulator to improve gait ability by adjusting the foot–ankle position during walking in patients with chronic stroke undergoing home-based rehabilitation.
Methods
This was a double-blinded, parallel-group randomized controlled trial. Thirty-one patients with chronic stroke and ankle–foot motor impairment were randomized to receive 3 weeks of gait training, which involved using the transcutaneous peroneal nerve stimulator while walking (tPNS group; n = 16, mean age: 52.25 years), or conventional home and/or community gait training therapy (CT group; n = 15, mean age: 54.8 years). Functional assessments were performed before and after the 3-week intervention. The outcome measures included spatiotemporal gait parameters, three-dimensional kinematic and kinetic data on the ankle–foot joint, and a clinical motor and balance function assessment based on the Fugl–Meyer Assessment of Lower Extremity (FMA-LE) and Berg Balance scales (BBS). Additionally, 16 age-matched healthy adults served as a baseline control of three-dimensional gait data for both trial groups.
Results
The FMA-LE and BBS scores improved in both the tPNS groups (p = 0.004 and 0.001, respectively) and CT groups (p = 0.034 and 0.028, respectively) from before to after training. Participants in the tPNS group exhibited significant differences in spatiotemporal gait parameters, including double feet support, stride length, and walking speed of affected side, and the unaffected foot off within a gait cycle after training (p = 0.043, 0.017, 0.001 and 0.010, respectively). Additionally, the tPNS group exhibited significant differences in kinematic parameters, such as the ankle angle at the transverse plane (p = 0.021) and foot progression angle at the frontal plane (p = 0.009) upon initial contact, and the peak ankle joint angle at the transverse plane (p = 0.023) and foot progression angle (FPA) at the frontal and transverse planes (p = 0.032 and 0.046, respectively) during gait cycles after 3 weeks of training.
Conclusions
Use of a portable tPNS device during walking tasks appeared to improve spatiotemporal gait parameters and ankle and foot angles more effectively than conventional home rehabilitation in patients with chronic stroke. Although guidelines for home-based rehabilitation training services and an increasing variety of market devices are available, no evidence for improvement of motor function and balance was superior to conventional rehabilitation.
Background
Stroke is one of the five leading causes of disability-adjusted life-years worldwide [1]. In China, the increasing incidence of stroke and decrease in related mortality have led to a rapid increase in the burden of society [2]. Gait dysfunction is common among stroke survivors and represents a major burden, while the community commonly might provide no more than 1-year’s rehabilitation service due to lack of therapists [3, 4]. After stroke, most patients experience abnormal lower extremity movement and a plantarflexion or inversion pattern of hemiplegia in the ankle and foot during the swing phase of gait [5]. Estimates suggest that 20–30% of stroke survivors experience ankle and foot drop and/or inversion, which causes abnormal gait [4]. Ankle–foot drop and inversion are caused by abnormal activation of the musculature in the distal lower limb and result in inefficient foot clearance and foot tremor during the swing phase of gait and a less stable stance. Consequently, stroke patients tend to exhibit a compensatory gait pattern involving the affected side, such as steppage gait, hip hiking, toe walking, and forefoot walking. These pathological deviations reduce the walking speed and increase the risk of fall, thus impeding an individual’s ability to walk efficiently both indoors and outdoors and restricting their participation in many activities of daily life and the community. Therefore, studies on stroke motor recovery have frequently identified inadequate ankle–foot control and stability during walking as a key factor to address when attempting to improve gait dysfunction [6,7,8,9].
Approaches such as ankle–foot orthosis (AFO), electrical stimulation (ES), and neuroprosthetic implants are used to treat drop foot in stroke survivors [10,11,12], and a meta-analysis revealed that these approaches yielded similar results [12]. AFO is a traditional treatment for ankle joint immobilization in the neutral position and can be used to support ankle dorsiflexion during the swing phase to improve gait stability. However, as a mechanical device, an static AFO only restricts ankle movement when it is worn, leading to no improvement of muscle activety,, reduced muscle activity and a restricted ankle range-of-motion higher possibility of falling over the long term [13, 14]. ES, an alternative approach, is widely used to achieve more physiological positioning of the ankle and foot and to improve ankle–foot function, for example neuromuscular electrical stimulation (NMES), functional electrical stimulation (FES) multichannel and neuroprosthetic implants with the development of electronic engineering technology [8, 15,16,17], but multichannel and implanted devices are not used widely in the clinical settings, which limits their translational use in community and home settings.
Studies conducted in the last 10 years have focused on volitional muscle activation combined with lower motor neuron stimulation, which contributes to several possible mechanisms of neuromuscular plasticity, including repeated muscle contractions leading to increased oxidative capacity; increased numbers of microcapillaries and changes in fiber type at the muscular level; and the convergence of orthodromic or antidromic impulses at the anterior horn, leading to the strengthening of synapses at the spinal level and changes in the cortex [17,18,19]. These effects of therapy culminate in increased volitional muscle activity in the weak dorsiflexors and evertors of the ankle. Such changes are thought to positively influence other biomechanical features and help restore the associated functions. Several studies have observed sustained improvements in volitional muscles after removal of therapeutic devices, particularly in terms of improved gait capacity during the chronic post-stroke stage [19,20,21]. One type of FES treatment, the transcutaneous peroneal nerve stimulator (tPNS), involves the placement of electrodes on the skin surface above the peroneal nerve, and based on the mechanisms of effects on volitional muscle activity combined with lower motor neurone stimulation during walking to acquire a more physiological positioning of ankle and foot. This clinically accepted rehabilitation intervention has been demonstrated to be more efficient than AFO, especially in terms of improving walking speed [22, 23]. However, a multicenter prospective randomized study found that the use of peroneal nerve FES was equivalent to device-free gait training in terms of the clinical outcomes of improvements in walking speed, the Fugl–Meyer Assessment of Lower Extremity (FMA-LE) score, ankle muscle strength and dorsiflexion performance [24].
Above studies in different views of the tPNS suggest that this therapeutic device is an appropriate alternative therapeutic device using at chronic stroke survivors for gait training. Other studies have focused on the physiological and biomechanical effects of tPNS on the kinematics and kinetics of the hip, knee, and ankle joints [16, 22, 25]. However, excessive pronation and supination of the foot and hyper-planta/dorsiflexion of the ankle joint directly result in an abnormal and unstable stance and toe clearance during walking, leading to a tilted posture and increasing the fall risk. The evidence so far for improvement of foot activity is still limited, especially its biomechanical analysis. This study focused on quantitative analysis of both kinematics and kinetics of the ankle joint and foot progression angles (FPA) and spatiotemporal gait and clinical assessment parameters. We aimed to determine the efficacy of tPNS among chronic stroke population and its feasibility for use as a rehabilitation training tool in home and community settings. This is important because most discharged stroke patients in China receive inadequate rehabilitation training at home due to a shortage of rehabilitation therapists.
Therefore, in our study, some chronic stroke patients discharged were recruited to randomized into two groups, including the home-based or community-based gait training was arranged via tPNS or self-training without tPNS with therapist’s guidance lasted for 2 h each day during 3 weeks. The results of gait parameters and clinical assessment outcomes were compared between groups before and after interventions.[…]

[Abstract] The use of rhythmic auditory stimulation for functional gait disorder: A case report
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, Music/Music therapy on February 26, 2022
Abstract
Background: Functional gait disorders (FGD) are a common and disabling condition. Consensus-based rehabilitation techniques for treating FGD and other functional neurological disorder presentations at large utilize a variety of therapeutic strategies, including distraction, novel approaches to movement, entrainment, stress/hypervigilance modulation, and psychotherapy.
Case report: Here we present a case of a 24-year-old woman with a complex history of anxiety, depression, left frontal astrocytoma, postural orthostatic tachycardia syndrome (POTS) and FGD. During a multidisciplinary inpatient rehabilitation stay for FGD, the patient underwent rhythmic auditory stimulation (RAS) delivered by a neurologic music therapist in conjunction with physical therapy, occupational therapy, and psychotherapy.
Results: The RAS intervention appeared to play a significant role in symptom resolution for this patient. Improvement in the patient’s truncal displacement, foot dragging, and well as overall gait speed occurred following serial RAS trials performed over a single treatment session. Benefits persisted immediately following the intervention and upon subsequent reassessment. Although at four-year follow-up the patient’s FGD symptoms remained resolved, fatigue continued to limit her ambulatory capacity and overall endurance.
Conclusion: RAS represents a unique therapeutic approach for treating FGD, complementary to existing consensus-based rehabilitation recommendations, and may warrant further consideration by the field.
[ARTICLE] Gait Improvement in Chronic Stroke Survivors by Using an Innovative Gait Training Machine: A Randomized Controlled Trial – Full Text
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop on January 3, 2022
Abstract
Chronic stroke leads to the impairment of lower limb function and gait performance. After in-hospital rehabilitation, most individuals lack continuous gait training because of the limited number of physical therapists. This study aimed to evaluate the effects of a newly invented gait training machine (I-Walk) on lower limb function and gait performance in chronic stroke individuals. Thirty community-dwelling chronic stroke individuals were allocated to the I-Walk machine group (n = 15) or the overground gait training (control) group (n = 15). Both groups received 30 min of upper limb and hand movement and sit-to-stand training. After that, the I-Walk group received 30 min of I-Walk training, while the control followed a 30-minute overground training program. All the individuals were trained 3 days/week for 8 weeks. The primary outcome of the motor recovery of lower limb impairment was measured using the Fugl–Meyer Assessment (FMA). The secondary outcomes for gait performance were the 6-minute walk test (6 MWT), the 10-meter walk test (10 MWT), and the Timed Up and Go (TUG). The two-way mixed-model ANOVA with the Bonferroni test was used to compare means within and between groups. The post-intervention motor and sensory subscales of the FMA significantly increased compared to the baseline in both groups. Moreover, the 6 MWT and 10 MWT values also improved in both groups. In addition, the mean difference of TUG in the I-Walk was higher than the control. The efficiency of I-Walk training was comparable to overground training and might be applied for chronic stroke gait training in the community.
1. Introduction
Stroke is a major cause of death and global disability [1]. Thirty percent of stroke survivors are incapable of walking independently [2]. Gait training by physical therapists is mainly available only in the poststroke acute phase for a short period [3]. Gait speed is an important indicator of community ambulation associated with walking competency. Greater gait speed suggests good functioning and better quality of life [4,5]. Ng et al. found that stroke patients with a gait impairment appeared to walk at a slower pace in the 10-meter walk test and a shorter length in the 6-minute walk test than healthy people [6]. As a result of the chronic phase of stroke (≥6 months), 50% of community-dwelling persons with hemiparesis fail to complete a 6-minute walk test (6 MWT), and they are only able to walk half the distance of their predicted values [7]. Gait training methods can be classified into conventional overground gait training, staircase gait training, and device-assisted gait training. Overground gait training is one of the most common interventions for poststroke individuals. It can be defined as a physical therapist-guided gait pattern together with related exercises with no high-technology assistive devices [8]. Meanwhile, staircase gait training is used to enhance cardiovascular endurance and is suitable for patients with good dynamic balance. On the other hand, patients with poor stability need assistive devices, such as partial weight support belts.Previous studies have reported the benefits of overground, treadmill, staircase, and device-assisted gait training on motor and sensory lower limb function, walking endurance, and walking speed in stroke survivors [9,10]. Gama et al. reported that the effects of overground training on motor function were superior to treadmill training in chronic stroke individuals [10]. Park and colleagues showed that step climbing and staircase walking exercise improved walking speed in chronic stroke patients, reducing the Timed Up and Go (TUG) test [11]. Moreover, Donath et al. reported that the staircase walking exercise enhanced cardiovascular endurance in healthy older individuals, indicated by a reduced resting heart rate [12]. Bizovičar et al. found that a motorized gait assistive device improved motor recovery measured by the Fugl-Meyer Assessment (FMA) in acute-chronic stroke patients after three weeks [9]. Pansuksawat et al. suggested that the I-Walk machine improved gait speed, motor impairment, the lower extremity joint angle, and the gait kinematic variables in chronic stroke [13].Neuroplasticity training in hemiparesis after a stroke consists of five principles—specificity, repetition, intensity, time, and salience [14]. Therefore, optimal training procedures should have these properties. Indeed, other tools or models of therapy may need to be considered rather than the traditional one-on-one interaction. Group or robot-assisted therapies are areas currently under investigation that support the goal of an increased number of repetitions [15]. This study aimed to examine the effects of an innovative gait training machine (I-Walk) on motor control and gait performance in community-dwelling persons with hemiparesis after a stroke.
[…]

[RESEARCH] Spatiotemporal, Kinematic and Kinetic Assessment of the Effects of a Foot Drop Stimulator for Home-Based Rehabilitation of Patients with Chronic Stroke — A Three-Dimensional Motion Analysis – Full Text
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, Tele/Home Rehabilitation on November 7, 2021
Abstract
Background: Gait disability affects the daily lives of patients with stroke in both home and community settings. An abnormal foot–ankle position can cause instability on the supporting surface and negatively affect gait. Our research team explored the ability of a portable peroneal nerve-targeting electrical stimulator to improve gait ability by adjusting the foot–ankle position during walking in patients with chronic stroke undergoing home-based rehabilitation.
Methods: This was a double-blinded, parallel-group randomized controlled trial. Thirty-one patients with chronic stroke and ankle–foot motor impairment were randomized to receive 3 weeks of gait training, which involved using the transcutaneous peroneal nerve stimulator while walking (tPNS group; n = 16, mean age: 52.25 years), or conventional home and/or community gait training therapy (CT group; n = 15, mean age: 54.8 years). Functional assessments were performed before and after the 3-week intervention. The outcome measures included spatiotemporal gait parameters, three-dimensional kinematic and kinetic data on the ankle-foot joint, and a clinical motor and balance function assessment based on the Fugl–Meyer Assessment of Lower Extremity (FMA-LE) and Berg Balance scales (BBS). Additionally, 16 age-matched healthy adults served as a baseline control of three-dimensional gait data for both trial groups.
Results: The FMA-LE and BBS scores improved in both the tPNS groups (p = .004 and .001, respectively) and CT groups (p = .034 and .028, respectively) from before to after training. Participants in the tPNS group exhibited significant differences in spatiotemporal gait parameters, including opposite foot off, double support, stride length, and walking speed, after training (p = .010, .042, .017 and .001, respectively). Additionally, the tPNS group exhibited significant differences in kinematic parameters, such as the ankle angle at the transverse plane (p = .021) and foot progression angle at the frontal plane (p = .009) upon initial contact, and the peak ankle joint angle at the transverse plane (p = .023) and foot progression angle at the frontal and transverse planes (p = .032 and .046, respectively) during gait cycles after 3 weeks of training.
Conclusions: Use of a portable tPNS device during walking tasks appeared to improve spatiotemporal gait parameters and ankle and foot angles more effectively than conventional home rehabilitation in patients with chronic stroke. Although guidelines for home-based rehabilitation training services and an increasing variety of market devices are available, no evidence for improvement of motor function and balance was superior to conventional rehabilitation.
Background
Stroke is one of the five leading causes of disability-adjusted life-years worldwide [1]. In China, the increasing incidence of stroke and decrease in related mortality have led to a rapid increase in the burden of decrease associated with this condition [2]. Gait dysfunction is common among stroke survivors and represents a major burden [3, 4]. After stroke, most patients experience abnormal lower extremity movement and a plantarflexion or inversion pattern of hemiplegia in the ankle and foot during the swing phase of gait [5]. Estimates suggest that 20–30% of stroke survivors experience ankle and foot drop and/or inversion, which causes abnormal gait [4]. Ankle–foot drop and inversion are caused by abnormal activation of the musculature in the distal lower limb and result in inefficient foot clearance and foot tremor during the swing phase of gait and a less stable stance. Consequently, stroke patients tend to exhibit a compensatory gait pattern involving the affected side, such as steppage gait, hip hiking, toe walking, and forefoot walking. These pathological deviations reduce the walking speed and increase the risk of fall, thus impeding an individual’s ability to walk efficiently both indoors and outdoors and restricting their participation in many activities of daily life and the community. Therefore, studies on stroke motor recovery have frequently identified inadequate ankle–foot control and stability during walking as a key factor to address when attempting to improve gait dysfunction [6-9].
Approaches such as ankle–foot orthosis (AFO), electrical stimulation (ES), and neuroprosthetic implants are used to treat drop foot in stroke survivors [10-12], and a meta-analysis revealed that these approaches yielded similar results [12]. AFO is a traditional treatment for ankle joint immobilization in the neutral position and can be used to support ankle dorsiflexion during the swing phase to improve gait stability. However, as a mechanical device, an AFO only restricts ankle movement when it is worn, leading to weakened muscles, reduced muscle activity and a restricted ankle range-of-motion over the long term [13, 14]. ES, an alternative approach, is widely used to achieve more physiological positioning of the ankle and foot and to improve ankle–foot function, for example neuromuscular electrical stimulation (NMES), functional electrical stimulation (FES) multichannel and neuroprosthetic implants with the development of electronic engineering technology[8, 15-17], but multichannel and implanted devices are not used widely in the clinical settings, which limits their translational use in community and home settings.
Studies conducted in the last 10 years have focused on volitional muscle activation combined with lower motor neuron stimulation, which contributes to several possible mechanisms of neuromuscular plasticity, including repeated muscle contractions leading to increased oxidative capacity; increased numbers of microcapillaries and changes in fiber type at the muscular level; and the convergence of orthodromic or antidromic impulses at the anterior horn, leading to the strengthening of synapses at the spinal level and changes in the cortex [17-19]. These effects of therapy culminate in increased volitional muscle activity in the weak dorsiflexors and evertors of the ankle. Such changes are thought to positively influence other biomechanical features and help restore the associated functions. Several studies have observed sustained improvements in volitional muscles after removal of therapeutic devices, particularly in terms of improved gait capacity during the chronic post-stroke stage [19-21] . One type of FES treatment, the transcutaneous peroneal nerve stimulator (tPNS), involves the placement of electrodes on the skin surface above the peroneal nerve, and based on the mechanisms of effects on volitional muscle activity combined with lower motor neurone stimulation during walking to acquire a more physiological positioning of ankle and foot. This clinically accepted rehabilitation intervention has been demonstrated to be more efficient than AFO, especially in terms of improving walking speed [22, 23]. However, a multicenter prospective randomized study found that the use of peroneal nerve FES was equivalent to device-free gait training in terms of the clinical outcomes of improvements in walking speed, the Fugl–Meyer Assessment of Lower Extremity (FMA-LE) score, ankle muscle strength and dorsiflexion performance [24].
Above studies in different views of the tPNS suggest that this therapeutic device is an appropriate alternative therapeutic device using at chronic stroke survivors for gait training. Other studies have focused on the physiological and biomechanical effects of tPNS on the kinematics and kinetics of the hip, knee, and ankle joints [16, 22, 25]. However, excessive pronation and supination of the foot and hyper-planta/dorsiflexion of the ankle joint directly result in an abnormal and unstable stance and toe clearance during walking, leading to a tilted posture and increasing the fall risk. This study focused on quantitative analysis of kinematics and kinetics of the ankle joint and foot progression angles and spatiotemporal gait and clinical assessment parameters. We aimed to determine the efficacy of tPNS and its feasibility for use as a rehabilitation training tool in home and community settings. This is important because most discharged stroke patients in China receive inadequate rehabilitation training at home due to a shortage of rehabilitation therapists. […]

[WEB PAGE] How Gait Training Via Exoskeleton Helps Boost Stroke Recovery
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, REHABILITATION, Rehabilitation robotics on February 28, 2021

Gait training using a robotic exoskeleton has the potential to help spur along the recovery of motor function after a stroke, a study published in Frontiers in Neurorobotics suggests.
In the study, researchers from Kessler Foundation used an Ekso GT robotic exoskeleton from Ekso Bionics Inc to demonstrate the potential to of high-dose therapy gait training to aid early rehabilitation after acute stroke.
Gait Training vs Standard of Care
Participants included 44 individuals (ages 18 to 82 years) admitted to Kessler Institute for Rehabilitation for acute stroke. Half received conventional standard of care (SOC), and half received SOC with an option for overground gait training in the Ekso GT (RE+SOC). Both groups received the same amount of overall therapy time.
Overground gait training in the exoskeleton was supervised by a licensed physical therapist who adjusted the variable bilateral assistance of the Ekso GT according to each individual’s progress. Outcome measures were total distance walked during inpatient rehabilitation and functional independence measure (FIM) score. The RE-SOC group trained in the Ekso GT at least three times during their stay.
“We found that gait training in the exoskeleton allowed us to increase the dose of gait training without increasing the duration of inpatient rehabilitation. Because overground walking in the exoskeleton requires active effort on the part of the participant, early intervention with this type of gait training promotes brain plasticity that may lead to greater functional improvements and more lasting effects when combined with conventional training.”
— Karen Nolan, PhD, assistant director of the Center for Mobility and Rehabilitation Engineering Research at Kessler Foundation
[Source(s): Kessler Foundation, EurekAlert]
[Abstract] The effects of virtual reality augmented robot-assisted gait training on dual-task performance and functional measures in chronic stroke: a randomized controlled single-blind trial
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, Rehabilitation robotics, Virtual reality rehabilitation on February 11, 2021
Abstract
Background
Many studies have demonstrated positive effects of virtual reality (VR) and robot-assisted gait training (RAGT) on balance, gait skills, functional capacity, active participation, and motivation in stroke patients, previously. However the effects of VR augmented RAGT on dual-task performance which requires simultaneous use of motor and cognitive parameters has not been investigated.
Aim
To primarily investigate the effects of virtual reality (VR) augmented robot-assisted gait training (RAGT) on dual-task performance and secondarily, functional measurements in chronic stroke patients.
Design
A randomized, single-blind trial.
Setting
Inpatient rehabilitation center.
Population
The study included 30 chronic stroke patients aged between 40-65 with the level of ≥ 3 from Functional Ambulation Classification and ≥ 24 from the Standardized Mini Mental State Examination.
Methods
Fifteen patients in the study group received VR augmented RAGT and 15 patients in the control group received only RAGT during 12 sessions (six weeks). All patients received neurodevelopmental therapy in addition to their treatments, simultaneously. To evaluate dualtask performance, motor and cognitive tasks were given in addition to the 10 Meter Walk (first motor task), and durations were recorded in seconds. Functional measures such as Functional Gait Assessment, Rivermead Mobility Index, Berg Balance Scale, Fall Activity Scale International, and the Functional Independence Measure for gait, mobility, balance, fear of falling, and independence in daily living activities were also applied, consecutively.
Results
The mean age of the study population was 57.93±5.91. After the treatment, single and dual-task gait speeds and cognitive dual-task performance increased in the study group (p <0.05), while no change was observed in the control group (p> 0.05). No significant difference was detected between the groups in terms of all assessments after the treatment (p>0.05).
Conclusions
This study demonstrated that VR augmented RAGT improved dual-task gait speeds and dual-task performance of chronic stroke patients however there were no difference between the two groups after the treatment. Although functional improvements were determined with VR combined RAGT approach, it was not superior to RAGT only treatment.
Clinical rehabilitation impact
The results of current study suggest the simultaneous use of VR as an adjunct therapy method to the functional training to obtain functional gains in ambulant patients with chronic stroke.
[WEB PAGE] Robotic exoskeleton training expands options for stroke rehabilitation
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, REHABILITATION, Rehabilitation robotics on January 30, 2021
by Kessler Foundation

A team of New Jersey researchers has demonstrated that high-dose therapy gait training using robotic exoskeletons may aid early rehabilitation for acute stroke. The article, “Robotic exoskeleton gait training during acute stroke inpatient rehabilitation,” was published October 30, 2020 in Frontiers in Neurorobotics.
The authors are Karen Nolan, Ph.D., Kiran Karunakaran, Ph.D., and Kathleen Chervin, of Kessler Foundation, Michael Monfett, MD, of Children’s Specialized Hospital, Radhika Bapineedu, MD, and Neil N. Jasey Jr, MD, of Kessler Institute for Rehabilitation, and Mooyeon Oh-Park, MD, of Burke Rehabilitation Hospital, formerly with Kessler. Drs. Nolan and Karunakaran are also affiliated with Children’s Specialized Hospital. Kessler scientists and clinicians have faculty appointments at Rutgers New Jersey Medical School.
The need for stroke rehabilitation is tremendous, given the large numbers of stroke survivors with deficits in mobility, balance and coordination that limit their activities of daily living. Advances in robotics and biomedical engineering are expanding the options for rehabilitative care. Researchers are applying new technologies to gait training that may offer advantages over traditional labor intensive physical therapy. This inpatient study of a robotic exoskeleton (Ekso GT, Ekso Bionics, Inc,) demonstrated the potential to improve gait training after acute stroke toward the goal of earlier recovery of motor function.
Participants included 44 individuals (ages 18 to 82 years) admitted to Kessler Institute for Rehabilitation for acute stroke. Half received conventional standard of care (SOC), and half received SOC with an option for overground gait training in the Ekso GT (RE+SOC). Both groups received the same amount of overall therapy time. Overground gait training in the exoskeleton was supervised by a licensed physical therapist who adjusted the variable bilateral assistance of the Ekso GT according to each individual’s progress. Outcome measures were total distance walked during inpatient rehabilitation and functional independence measure (FIM) score. The RE-SOC group trained in the Ekso GT at least three times during their stay.
“We found that gait training in the exoskeleton allowed us to increase the dose of gait training without increasing the duration of inpatient rehabilitation,” said Dr. Nolan, assistant director of the Center for Mobility and Rehabilitation Engineering Research at Kessler Foundation. “Because overground walking in the exoskeleton requires active effort on the part of the participant,” she added, “early intervention with this type of gait training promotes brain plasticity that may lead to greater functional improvements and more lasting effects when combined with conventional training.”
Explore further Robotic exoskeleton training improves walking in adolescents with acquired brain injury
More information: Karen J. Nolan et al, Robotic Exoskeleton Gait Training During Acute Stroke Inpatient Rehabilitation, Frontiers in Neurorobotics (2020). DOI: 10.3389/fnbot.2020.581815
Provided by Kessler Foundation
[Abstract] Lessons learned from robotic gait training during rehabilitation: Therapeutic and medical severity considerations over 3 years
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, REHABILITATION, Rehabilitation robotics on September 21, 2020
Abstract
BACKGROUND: Robotic exoskeletons are increasingly available to inpatient rehabilitation facilities though programmatic implementation evidence is limited.
OBJECTIVE: To describe therapists’ clinical practice experiences with robotic gait training (RGT) over 3 years during inpatient rehabilitation.
METHODS: Therapists participated in a survey and semi-structured focus group to discuss their RGT experiences. Interviews were recorded, transcribed, and analyzed using a theoretical analysis-driven thematic approach.
RESULTS: Therapists averaged 7.6 years of neurologic rehabilitation experience and 1.85 years with RGT. Eight of 10 therapists had completed ⩾ 50 RGT sessions, with frequency of 1–5 sessions/week, including on-label (spinal cord injury, stroke) and off-label (e.g., traumatic brain injury) experiences. Three adverse events occurred over 716 RGT sessions with 186 patients. Qualitative analysis identified three major themes and corresponding subthemes: 1-Comparison with traditional gait training approaches (6 sub-themes), 2-Clinical decision-making considerations (3), and 3-On-label and off-label utilization (4). Stated RGT benefits included decreased therapists’ physical burden and increased patient motivation. Clinical concerns with RGT included tonicity, continence, and patient communication (e.g., aphasia). Off-label RGT was used to overcome barriers in traditional gait therapy and achieve early mobility.
CONCLUSIONS: Therapists’ level of training and clinical knowledge furthered RGT implementation and allowed for safe utilization with on-label and off-label patients.
Source: https://content.iospress.com/articles/technology-and-disability/tad190248
[WEB SITE] Gait Training & Ceiling Mounted Physical Therapy System – Gorbel Rehabilitation
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, REHABILITATION on September 4, 2020

Gorbel Rehabilitation
“We Improve People’s Lives” is the cornerstone in Gorbel’s Mission. Improving the safety, efficiency and quality of gait training and balance therapy is our fundamental purpose with each device we design, develop and manufacture. Our best opportunity to meet this objective has always been by working directly with the people we aim to serve; rehabilitation therapists. Whether it is a body weight support system, a rehabilitation harness, or a fall protection mobility trainer, the contributions of therapists are evident in every product in the SafeGait Solutions for rehabilitation.
Dynamic Gait and Mobility Products

SAFEGAIT 360

SAFEGAIT ACTIVE

ACCESSORIES

STEPRIGHT STABILITY TRAINER
For more visit site —–> https://www.gorbelrehabilitation.com/
