Reviewed by Lily Ramsey, LLM Jul 24 2023
Statistics indicate that globally 1 in 4 adults over the age of 25 will have a stroke in their lifetime. One of the most serious consequences of this disease is disability. The joint study by Rytis Maskeliūnas, a researcher at Kaunas University of Technology, Faculty of Informatics (KTU IF), and Lithuanian researchers is focused on creating an artificial intelligence (AI)-based system that aims to facilitate the rehabilitation process.
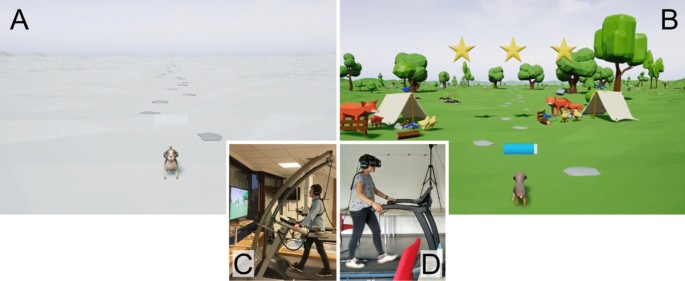
More recently, a team of researchers presented BiomacVR, an innovation that aims to help stroke victims get back on their feet as quickly as possible. Shortly afterwards, a third component of this technology was developed: BiomacEMG.
According to Maskeliūnas, the new system is a part of the Biomac project’s solutions, for monitoring the arm. This system will be useful for those patients who need to monitor the movements of the hand or the whole arm during rehabilitation exercises.
The KTU researcher believes that the integration of motion recognition technology into physical therapy is an innovation that will allow patients to focus on the task at hand and perform it correctly. The software enables the patient to study and adjust the exercises, which ensures an efficient healing and rehabilitation process.
Motion is measured by a bracelet
According to the researcher, the new system essentially measures muscle movements: “Our study evaluated the technical feasibility of measuring and recognizing the arm movements of the participants in the experiment, and thus monitoring the rehabilitation or other medical process”.
At this stage, in order to check the accuracy, it was chosen to measure not only the movements of the whole arm or another large part of the body but also more precise scenarios, i.e. to investigate the movements made by the fingers.
The wearable equipment, more specifically, a bracelet measuring the state of the nerves, muscles and the nerve cells that control them, is placed on the forearm and used to measure different types of muscle groups in real-time. According to Maskeliūnas, the process is simple – you put the bracelet on your arm and try to make the gestures shown in the picture. The system (or a doctor online) informs you whether you are doing the exercises correctly or incorrectly.
Our team was responsible for the system, and the colleagues from other Lithuanian universities developed the biomechanics model (a model of the muscles and their movements) and carried out the testing.”
Rytis Maskeliūnas, Researcher, Kaunas University of Technology
The system benefits not only the patient but also the professional
“Our new methodology with electromyography (EMG) elements is particularly important for proper exercise design during a rehabilitation programme. With this new technology, you can see exactly which muscle is working and at what capacity, how it reacts to the load and how quickly it recovers. This information allows the specialist to work with the patient not blindly, but knowing exactly which muscles are working well, which are overworked, or which are not even tired,” says Aušra Adomavičienė, a researcher at the Faculty of Medicine at Vilnius University (VU MF).
In her opinion, such technology is not only a great help to the rehabilitation specialist, but it is equally essential for the patient, who, with such technology, can continue the exercises at home, see the progress, and feel safe and secure, without doubts about whether they are doing it right, or whether they are harming themselves, etc.
AI In Healthcare eBook Compilation of the top interviews, articles, and news in the last year. Download the latest edition
“This system is important for patients with musculoskeletal disorders or diseases that require the restoration of lost movement and mobility function, which is directly caused by reduced or lost muscle function. These are the patients who have suffered a cerebral infarction, various traumas, fractures, soft tissue or nerve damage, systemic diseases such as Multiple Sclerosis or Parkinson’s Disease,” says Adomavičienė.
The researcher points out that this innovative technology can also be used for wellness purposes. For example, people who, due to irregular, poor working posture, or repetitive movements at work that strain one segment of the body, have muscular imbalances in their bodies, and often experience chronic pain (back, shoulder or wrist) or fatigue. According to Adomavičienė, the simple, user-friendly and easy-to-use technology is suitable for people of any age, whether child or adult.
These technologies are our future
“I think that after 20 years, patients and professionals involved in rehabilitation will not even be able to imagine that during functional assessment, testing and program execution, they were guided by the subjective, hand-held instruments that we now use on a daily basis,” says Adomavičienė.
According to her, computerized and intelligent systems based on artificial intelligence strategies will not only be able to identify in detail the problems experienced by the patient, but after the assessment, they will be able to analyze, systematize and provide feedback, i.e. to provide information and recommendations during the live sessions on how to adjust the rehabilitation programme individually according to the patient’s situation to increase tolerance to physical load, activate recovery mechanisms and the healing process.
KTU researcher Maskeliūnas agrees with his colleague: “Future research should also look at the development of individualised treatment plans and the adaptation of the algorithm to respond to a wider range of possible actions, taking into account the individual needs of the patient.”
Although the study evaluated the accuracy of the system in measuring hand movement patterns, the long-term impact on functional recovery in stroke patients needs to be further investigated, including the integration of this approach with other therapies such as occupational and physical therapy, according to Maskeliūnas.
Source: Kaunas University of Technology (KTU)