Archive for category Rehabilitation robotics
Soft robotic nerve cuffs could revolutionize treatment of neurological conditions
Posted by Kostas Pantremenos in REHABILITATION, Rehabilitation robotics on May 4, 2024
Soft robotic nerve cuffs could revolutionize treatment of neurological conditions
Source: Soft robotic nerve cuffs could revolutionize treatment of neurological conditions
[Abstract] Hybrid Brain-Computer Interface Controlled Soft Robotic Glove for Stroke Rehabilitation
Posted by Kostas Pantremenos in Paretic Hand, Rehabilitation robotics on April 26, 2024
Abstract:
Soft robotic glove controlled by a brain-computer interface (BCI) have demonstrated effectiveness in hand rehabilitation for stroke patients. Current systems mostly rely on static visual representations for patients to perform motor imagination (MI) tasks, resulting in lower BCI performance. Therefore, this study innovatively used MI and high-frequency steady-state visual evoked potential (SSVEP) to construct a friendly and natural hybrid BCI paradigm. Specifically, the stimulation interface sequentially presented decomposed action pictures of the left and right hands gripping a ball, with the pictures flashing at specific stimulation frequencies (left: 34 Hz, right: 35 Hz). Integrating soft robotic glove as feedback, we established a comprehensive “peripheral – central – peripheral” hand rehabilitation system to facilitate the hand rehabilitation of patients. Filter bank common spatial pattern (FBCSP) and filter bank canonical correlation analysis (FBCCA) algorithms were used to identify MI and SSVEP signals, respectively. Additionally, to fuse the features of these two signals, we proposed a novel fusion algorithm for improving the recognition accuracy of the system. The feasibility of the proposed system was validated through online experiments involving 12 healthy subjects and 9 stroke patients, achieving accuracy rates of 95.83 ± 6.83% and 63.33 ± 10.38%, respectively. The accuracy of MI and SSVEP in 12 healthy subjects reached 81.67 ± 15.63% and 95.14 ± 7.47%, both lower than the accuracy after fusion, these results confirmed the effectiveness of the proposed algorithm. The accuracy rate was more than 50% in both healthy subjects and patients, confirming the effectiveness of the proposed system.
[Abstract + References] The usefulness of assistive soft robotics in the rehabilitation of patients with hand impairment: A systematic review
Posted by Kostas Pantremenos in Paretic Hand, REHABILITATION, Rehabilitation robotics on March 26, 2024
Abstract
Introduction
Loss of hand function causes severe limitations in activity in daily living. The hand-soft robot is one of the methods that has recently been growing to increase the patient’s independence. The purpose of the present systematic review was to provide a classification, a comparison, and a design overview of mechanisms and the efficacy of the soft hand robots to help researchers approach this field.
Methods
The literature research regarding such tools was conducted in PubMed, Google Scholar, Science Direct, and Cochrane Central Register for Controlled Trials. We included peer-reviewed studies that considered a soft robot glove as an assistive device to provide function. The two investigators screened the titles and abstracts, then independently reviewed the full-text articles. Disagreements about inclusion were resolved by consensus or a third reviewer.
Results
A total of 15 articles were identified, describing 210 participants (23 healthy subjects). The tools were in three categories according to their actuation type (pneumatic system, cable-driven, another design). The most critical outcomes in studies included functional tasks (fourteen studies), grip strength (four studies), range of motion (ROM) (five studies), and user satisfaction (five studies).
Discussion
Function and grip parameters are the most common critical parameters for tests of hand robots. Cable-driven transmission and soft pneumatic actuators are the most common choices for the actuation unit. Radder et al. study had the highest grade from other studies. That was the only RCT among studies.
Conclusion
Although few soft robotic gloves can be considered ready to reach the market, it seems these tools have the potential to be practical for people with a disability. But, we lack consistent evidence of comparing two or more soft robot gloves on the hand functions. Future research needs to assess the effect of soft robotic gloves on people with hand disorders with more populations.
Introduction
Over sixty million people suffer from hand disabilities globally (Lawrence et al., 2001; Organization and Society, 2013). Hand function recovery is crucial for the independence of people with disability (Almenara et al., 2017). Hand robots are one of the methods that are growing recently because of increasing the patient’s independence (Gopura et al., 2011). Soft robots and exoskeletons are two available benches for rehabilitation robots. High weight, bulky, complex, and limited interaction with an environment are some of the limitations of the exoskeletons (Gopura et al., 2016; Jiryaei et al., 2021). The exoskeletons are expensive and non-portable, which restricts the rehabilitation process at home. Hence, they need to develop lightweight and wearable robots (Cappello et al., 2018; Trivedi et al., 2008).
Soft robots are one of the newest and most innovative technological devices. These tools allow interaction between the execution of motions and the intentions of the tool and the users (Kazerooni, 2005; Pons et al., 2008). Clinical studies showed that users who used soft robotics during rehabilitation programs significantly improved hand motor functionality compared to patients without soft robots (Ueki et al., 2010).
Recently, many research groups have begun to develop and evaluate robotic gloves with soft and flexible materials (e.g., cable-driven, fluidic soft actuators, and soft pneumatic actuators) (Bardi et al., 2022; Trivedi et al., 2008). Soft robots provide more degrees of freedom, more safety, less weight, and less complexity than exoskeletons. In addition, the soft robots are suitable for delicate and sensitive movements and improve activities of daily living (ADL) with the hand (Diftler et al., 2014; Heo et al., 2012; Kadowaki et al., 2011; Polygerinos et al., 2015; Trivedi et al., 2008).
Using soft materials enables a structure without joints, which resolves the problem of aligning human finger joints with a rigid exoskeleton (Sarakoglou et al., 2016). This concept of a wearable soft-robotic glove allows low-performance users to employ their hands in ADL. It may even reduce the need for healthcare professionals and is thought to improve hand-function users’ independence in performing ADL (Radder et al., 2019).
In a systematic review, Bardi et al., assessed sixty-nine soft robots for the upper limb (105 articles) (Bardi et al., 2022). Although this review included a wide of soft robots for upper limbs, the researchers reviewed the studies related to technical points and did not consider clinical tests. In a narrative review, the clinical outcomes of the soft robots were reviewed, but only papers with SCI participants were selected (Cardoso et al., 2022). To the best of our knowledge, a comprehensive review of the topic with a clinical view needs to be included. Thus, this systematic review provides a classification, a comparison, and a design overview of mechanisms and the efficacy of the soft glove robots to help researchers approach this field. We reviewed these outcomes outcome measures functional tasks, grip and pinch strength, ROM, and user satisfaction, in the present study.
Section snippets
Search strategy
This systematic review was conducted according to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement (Mark Vrabel, 2015) and registered with the PROSPERO database. The search strategy was based on the Population Intervention Comparison Outcome (PICO) method and included all relevant articles published from January 2005 to April 2022. Do studies of hand robots could be benefit for researchers and clinicians? To answer this question a
Description of the studies
The present study restricted the research to papers written in English and published from January 2005 to April 2022 (see Fig. 1). The search strategy yielded 874 articles. After a full review of the articles, 15 met the inclusion criteria. This review summarizes the results of studies that evaluated soft robotic gloves on patients with hand impairment. The researchers modified the Downs and Black scale to 15 items. Four papers received a maximum score (a score of 12), and the six papers
Discussion
The present study demonstrates soft robots will have a very high potential in the near future. However, this area needs more strong evidence and clinical tests. This review’s results amplify the effect of clinical tests of soft robot gloves. The main applications for which these tools have been developed are related to the assistance of disabled people. Function and grip parameters are the most common critical parameters for tests of hand robots. From a technical view, cable-driven transmission
Conclusion
In conclusion, this study confirms that soft robots might show very high potential, but they have yet to reach the market. This review could infer no reports with long effects of using soft devices on ADL and the quality of life of disabled people. Thus, clinical trials are needed to assess the effectiveness of soft hand robots and identify the needs of disabled people who can benefit the most from these types of tools. Overall, soft robots can be a window of hope for them. Hopefully, soon
Clinical relevance
- •Soft robots may improve grip, reduce limitations and increase function.
- •Soft robots may benefit by increasing the quality of life for people with disability in hand.
References (39)
- R. Gopura et al.Developments in hardware systems of active upper-limb exoskeleton robots: a reviewRobot. Autonom. Syst.(2016)
- Z. Jiryaei et al.Development and feasibility of a soft pneumatic-robotic glove to assist impaired hand function in quadriplegia patients: a pilot studyJ. Bodyw. Mov. Ther.(2021)
- M. Almenara et al.Usability test of a hand exoskeleton for activities of daily living: an example of user-centered designDisabil. Rehabil. Assist. Technol.(2017)
- E. Bardi et al.Upper limb soft robotic wearable devices: a systematic reviewJ. NeuroEng. Rehabil.(2022)
- L. Cappello et al.Assisting hand function after spinal cord injury with a fabric-based soft robotic gloveJ. NeuroEng. Rehabil.(2018)
- L.R. Cardoso et al.Soft robotics and functional electrical stimulation advances for restoring hand function in people with SCI: a narrative review, clinical guidelines and future directionsJ. NeuroEng. Rehabil.(2022)
- M. Diftler et al.RoboGlove-A robonaut derived multipurpose assistive device
- S.H. Downs et al.The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventionsJ. Epidemiol. Community(1998)
- H.C. Fischer et al.Use of a portable assistive glove to facilitate rehabilitation in stroke survivors with severe hand impairmentIEEE Trans. Neural Syst. Rehabil. Eng.(2015)
- L. Ge et al.Design, modeling, and evaluation of fabric-based pneumatic actuators for soft wearable assistive glovesSoft Robot.(2020)
View more references
[Review] Soft Hand Exoskeletons for Rehabilitation: Approaches to Design, Manufacturing Methods, and Future Prospects
Posted by Kostas Pantremenos in Paretic Hand, Rehabilitation robotics on March 24, 2024
Abstract
Stroke, the third leading cause of global disability, poses significant challenges to healthcare systems worldwide. Addressing the restoration of impaired hand functions is crucial, especially amid healthcare workforce shortages. While robotic-assisted therapy shows promise, cost and healthcare community concerns hinder the adoption of hand exoskeletons. However, recent advancements in soft robotics and digital fabrication, particularly 3D printing, have sparked renewed interest in this area. This review article offers a thorough exploration of the current landscape of soft hand exoskeletons, emphasizing recent advancements and alternative designs. It surveys previous reviews in the field and examines relevant aspects of hand anatomy pertinent to wearable rehabilitation devices. Furthermore, the article investigates the design requirements for soft hand exoskeletons and provides a detailed review of various soft exoskeleton gloves, categorized based on their design principles. The discussion encompasses simulation-supported methods, affordability considerations, and future research directions. This review aims to benefit researchers, clinicians, and stakeholders by disseminating the latest advances in soft hand exoskeleton technology, ultimately enhancing stroke rehabilitation outcomes and patient care.
1. Introduction
Strokes are the second leading cause of death worldwide [1,2,3]. These events, which consist of the sudden death of some brain cells due to lack of oxygen when blood flow is lost due to blockage or rupture of an artery [4,5], are also the third cause of permanent disability and one of the main causes of dementia and depression [6,7]. The occurrence of strokes is subject to different risk factors [8,9]. Diseases such as hypertension and diabetes, along with habits such as smoking, are considered modifiable risk factors, that is, factors susceptible to prevention. Other risk factors are not preventable, such as atrial fibrillation and transient ischemic attacks, which are presumed to be of genetic origin [10].
Globally, 70% of strokes and 87% of deaths related to these events occur in low- and middle-income countries [11]. Over the past four decades, the incidence of stroke in low- and middle-income countries has increased by more than 100%. During these decades, its incidence has decreased by 42% in high-income countries. On average, this event occurs 15 years earlier and causes more deaths for people living in low- and middle-income countries when compared to those in high-income countries. Strokes mainly affect people at the peak of their productive lives [12], and despite its enormous impact on the socio-economic development of countries, this growing crisis has received very little attention to date.
Recent neurological research indicates that impaired motor skills of stroke patients can be improved and possibly restored through repetitive, task-oriented training [13,14,15,16,17]. This is due to a property of the human brain known as neuroplasticity or the ability of the brain to reorganize itself by establishing new neural connections [18,19]. On this basis, the use of automatic devices has been implemented to help therapists increase the intensity of treatments, produce multisensory stimulation, and reduce costs during their work [20,21,22,23,24,25]. This new concept dates to the early 1990s with a new family of robotic machines called “haptic interfaces”. These mechanical devices were designed to interact with the human being, guiding the upper limb towards passive and active assisted mobilization, assisting in some movement tasks through biofeedback systems, and measuring kinematic changes and dynamics in motion. However, there is no consensus on the metrics or devices used to treat motor function deficiencies through neuroplasticity [26,27]. Additionally, recovery success relies heavily on a patient’s ability to attend therapy, which can be deterred by the frequency, duration, or cost of the therapy [28]. In this way, robotic therapy could represent a standard and successful complement to rehabilitation programs, improve patient access, and increase compliance and subsequent outcomes of rehabilitation efforts.
Despite the multiple designs reviewed in the last decade [29], there is no clinical evidence of the superiority of robotic training over traditional therapy. However, this procedure can complement traditional therapy processes [30]. In contrast, soft robots have the potential to overcome the limitations that are present in rigid robots. This design paradigm, inspired by the behavior and structure of living things, seems to be more compatible with rehabilitation activities due to increased versatility and compliance [31,32].
In addition, the solutions proposed, under the appropriate portability parameters, would have the potential to support the patient in the execution of activities of daily living, increasing their level of independence, mental health, and the well-being of their family nucleus.
The purpose of this work is to present a comparative review of the most recent rehabilitation hand exoskeletons based on soft actuators. This comparison is based on two main criteria: (i) the complexity of the manufacturing process and (ii) the resulting adaptability to the patient’s anatomy in rehabilitation environments.
This review also wants to motivate future designers to work in interdisciplinary solutions, taking into consideration multiple initiatives related to the implementation of makerspaces within the facilities of healthcare institutions, enabling the high reception and adoption of digital fabrication methods in society, and specifically, in healthcare [33,34,35,36,37,38]. […]

[Abstract] A Review on Soft Exoskeletons for Hand Rehabilitation
Posted by Kostas Pantremenos in Paretic Hand, Rehabilitation robotics on February 24, 2024
Background: How to enhance the quality of life for the elderly has emerged as a key issue in many nations due to the ageing population. Stroke is the most prevalent disease among the elderly; specifically, the hand dysfunction caused by stroke is also a powerful obstacle to the daily life of the elderly. Soft Exoskeletons for Hand Rehabilitation (SEHRs) have become a major trend for the future due to the increasing demand for hand rehabilitation.
Objective: To provide a reference for readers in this field by introducing the most recent research developments in the field of SEHR, including their classification and properties.
Methods: By reviewing different types of hand rehabilitation exoskeleton research papers and patents, the advantages and disadvantages, differences, and applications of various SEHRs were summarized.
Results: According to the driving mode and realizing the function of SEHRs, the structure characteristics of SEHRs are analyzed and compared. The key problems and future development trends of SEHRs were expounded.
Conclusion: According to the driving method, the research shows that SEHRs can be divided into Air-Driven Soft Exoskeletons for Hand Rehabilitation (ADSEHRs), Motor-Driven Soft Exoskeletons for Hand Rehabilitation (MDSEHRs), and Hybrid-Driven Soft Exoskeletons for Hand Rehabilitation (HDSEHRs). Future research is required to further optimize the flexibility and adaptability of soft exoskeletons, improve their accuracy and sensitivity, and enhance human-machine interaction with the human hand.
[Abstract + References] Research progress and development trend of flexible hand rehabilitation gloves
Posted by Kostas Pantremenos in Paretic Hand, REHABILITATION, Rehabilitation robotics on February 20, 2024
Abstract
The flexible hand rehabilitation glove is proposed to solve the problems of long rehabilitation training time for patients and high workload for doctors, and to make the treatment more effective. With the advances in robotics, robotic-assisted therapy has developed rapidly and has become an essential complement to conventional treatment. To understand flexible hand rehabilitation glove devices, with the different construction types of actuators and drive methods as the mainline, the corresponding study of these structures as the auxiliary lines. The characteristics and the current state of research have been discussed. A brief introduction to manufacturing actuators and rehabilitation systems is also given. Through the analysis of hand rehabilitation gloves, some current advantages and disadvantages are summarized, and future directions and functional diversification are envisaged. Certain feasible research suggestions have been proposed for future development regarding structure, functional diversity, and a combination of driving methods. These include that there will be more combinations of pneumatic and motor driven, combining the advantages of both methods to overcome the disadvantages of each. The structural design will be more in line with anatomy and ergonomics, make it more esthetically pleasing. More innovative controls methods will be adopted to achieve more complex rehabilitation functions.
References
1. Taylor CL, Schwarz RJ. The anatomy and mechanics of the human hand. Artif Limbs 1955; 2(2): 22–35.
2. Chim H. Hand and wrist anatomy and biomechanics: a comprehensive guide. Plast Reconstr Surg 2017; 140(4): 865–865.
3. Nas K, Yazmalar L, Şah V, et al. Rehabilitation of spinal cord injuries. World J Orthop 2015; 6(1): 8–16.
4. Silva NA, Sousa N, Reis RL, et al. From basics to clinical: a comprehensive review on spinal cord injury. Prog Neurobiol 2014; 114: 25–57.
5. Davis A. Medical, psychosocial and vocational aspects of disability, 4th edition.J Rehabil 2015; 81(3): 58–59.
6. Gassert R, Dietz V. Rehabilitation robots for the treatment of sensorimotor deficits: a neurophysiological perspective. J Neuroeng Rehabil 2018; 15(1): 46.
7. Mlinac ME, Feng MC. Assessment of activities of daily living, self-care, and independence. Arch Clin Neuropsychol 2016; 31(6): 506–516.
8. Rudd AG, Bowen A, Yang GR. The latest national clinical guideline for stroke. Clin Med 2017; 17(4): 382–383.
9. O’Driscoll SW, Giori NJ. Continuous passive motion (CPM): theory and principles of clinical application. J Rehabil Res Dev 2000; 37(2): 179–188.
10. Bütefisch C, Hummelsheim H, Denzler P, et al. Repetitive training of isolated movements improves the outcome of motor rehabilitation of the centrally paretic hand. J Neurol Sci 1995; 130(1): 59–68.
11. Iqbal J, Baizid K. Stroke rehabilitation using exoskeleton-based robotic exercisers: mini review. Biomed Res 2014; 26(26): 197–201.
12. Rotella M, Reuther K, Hofmann C, et al. An orthotic hand-assistive exoskeleton for actuated pinch and grasp. In: 2009 IEEE 35th annual northeast bioengineering conference, Cambridge, MA, 3–5 April 2009, pp.338–339. New York: IEEE.
13. Li G, Cheng L, Gao Z, et al. Development of an untethered adaptive thumb exoskeleton for delicate rehabilitation assistance. IEEE Trans Robot 2022; 38(6): 3514–3529.
14. Kang B, In H, Cho K. Modeling of tendon driven soft wearable robot for the finger. In: 2013 10th international conference on ubiquitous robots and ambient intelligence (URAI), Jeju, South Korea, 30 October–2 November 2013, pp.459–460. New York: IEEE.
15. Yap HK, Lim JH, Goh JCH, et al. Design of a soft robotic glove for hand rehabilitation of stroke patients with clenched fist deformity using inflatable plastic actuators. J Med Device 2016; 10(4): 044504.
16. Yap HK, Lim JH, Nasrallah F, et al. Characterisation and evaluation of soft elastomeric actuators for hand assistive and rehabilitation applications. J Mar Eng Technol 2016; 40(4): 199–209.
17. Shahid T, Gouwanda D, Nurzaman SG, et al. Moving toward soft robotics: a decade review of the design of hand exoskeletons. Biomimetics 2018; 3(3): 17.
18. Ahmed Y, Ai-Neami, Lateef S. Robotic glove for rehabilitation purpose: review. In: The 3rd scientific conference of electrical and electronic engineering researches (SCEEER), Basrah, Iraq, 15–16 June 2020, pp.15–16. New York: IEEE.
19. du Plessis T, Djouani K, Oosthuizen C. A review of active hand exoskeletons for rehabilitation and assistance. Robotics 2021; 10(1): 40.
20. Tran P, Jeong S, Herrin KR, et al. Review: hand exoskeleton systems, clinical rehabilitation practices, and future prospects. IEEE Trans Med Robot Bionics 2021; 3(3): 606–622.
21. Pérez Vidal AF, Rumbo Morales JY, Ortiz Torres G, et al. Soft exoskeletons: development, requirements, and challenges of the last decade. Actuators 2021; 10(7): 166.
22. Tiboni M, Amici C. Soft gloves: a review on recent developments in actuation, sensing, control and applications. Actuators 2022; 11(8): 232.
23. Heo P, Gu GM, Lee SJ, et al. Current hand exoskeleton technologies for rehabilitation and assistive engineering. Int J Precis Eng Manuf 2012; 13(5): 807–824.
24. Balasubramanian S, Klein J, Burdet E. Robot-assisted rehabilitation of hand function. Curr Opin Neurol 2010; 23(6): 661–670.
25. Fonseca MCR, Elui VMC, Lalone E, et al. Functional, motor, and sensory assessment instruments upon nerve repair in adult hands: systematic review of psychometric properties. Syst Rev 2018; 7(1): 175.
26. Pataky TC, Latash ML, Zatsiorsky VM. Multifinger Ab- and adduction strength and coordination. J Hand Ther 2008; 21(4): 377–385.
27. Hunter S, Crome P. Hand function and stroke. Rev Clin Gerontol 2002; 12(1): 68–81.
28. Boser QA, Dawson MR, Schofield JS, et al. Defining the design requirements for an assistive powered hand exoskeleton: a pilot explorative interview study and case series. Prosthet Orthot Int 2021; 45(2): 161–169.
29. Aubin PM, Sallum H, Walsh C, et al. A pediatric robotic thumb exoskeleton for at-home rehabilitation: the isolated orthosis for thumb actuation (IOTA). Int J Intell Comput Cybern 2014; 7(3): 233–252.
30. Hines AE, Crago PE, Billian C. Hand opening by electrical stimulation in patients with spastic hemiplegia. IEEE Trans Rehabil Eng 1995; 3(2): 193–205.
31. Ilievski F, Mazzeo AD, Shepherd RF, et al. Soft robotics for chemists. Angew Chem 2011; 50(8): 1890–1935.
32. Polygerinos P, Lyne S, Wang Z, et al. Towards a soft pneumatic glove for hand rehabilitation. In: 2013 IEEE/RSJ international workshop on intelligent robots and systems (IROS), Tokyo, Japan, 3–7 November 2013, pp.1512–1517. New York: IEEE.
33. Tiboni M, Loda D. Monolithic PneuNets soft actuators for robotic rehabilitation: methodologies for design, production and characterization. Actuators 2023; 12(7): 299.
34. Yang Y, Chen Y, Li Y, et al. Bioinspired robotic fingers based on pneumatic actuator and 3D printing of smart material. Soft Robot 2017; 4(2): 147–162.
35. Yap H, Lim J, Nasrallah F, et al. A soft exoskeleton for hand assistive and rehabilitation application using pneumatic actuators with variable stiffness. In: 2015 IEEE international conference on robotics and automation (ICRA), Seattle, WA, 26–30 May 2015, pp.4967–4972. New York: IEEE.
36. Wang J, Fei Y, Pang W. Design, modeling, and testing of a soft pneumatic glove with segmented pneunets bending actuators. IEEE/ASME Trans Mechatron 2019; 24(3): 990–1001.
37. Guo S, Zhao F, Wei W, et al. Soft actuator for hand rehabilitation. In: 2015 IEEE international conference on mechatronics and automation (ICMA), Beijing, China, 2–5 August 2015. New York: IEEE.
38. Mosadegh B, Polygerinos P, Keplinger C, et al. Pneumatic networks for soft robotics that actuate rapidly. Adv Funct Mater 2014; 24(15): 2163–2170.
39. Lalegani Dezaki M, Bodaghi M, Serjouei A, et al. Soft pneumatic actuators with controllable stiffness by bio-inspired lattice chambers and fused deposition modeling 3D printing. Adv Eng Mater 2023; 25(6): 2200797.
40. Li X, Lin Y, Jia J. Design and implementation of a hand rehabilitation device for stroke. Mech Eng Technol 2021; 50(3): 104–105.
41. Jiang Y, Chen D, Liu P, et al. Fishbone-inspired soft robotic glove for hand rehabilitation with multi-degrees-of-freedom. In: 2018 IEEE international conference on soft robotics (RoboSoft), Livorno, Italy, 24–28 April 2018, pp.394–399. New York: IEEE.
42. Meng F, Liu C, Li Y, et al. Personalized and safe soft glove for rehabilitation training. Electronics 2023; 12(11): 2531.
43. Zhang J, Hu D, Hong J, et al. A user-defined passive pneumatic soft body manipulator. CN Patent 110 236 880. September17, 2019.
44. Haghshenas-Jaryani M, Patterson RM, Bugnariu N, et al. A pilot study on the design and validation of a hybrid exoskeleton robotic device for hand rehabilitation. J Hand Ther 2020; 33(2): 198–208.
45. Fan S, Jin M, Li B, et al. Rigid-flexible coupled extensible articulated soft exoskeleton glove and method. CN Patent 111 150 602, 15 May 2020.
46. Yang K, Mao Z, Yamamoto K. Finger joint rehabilitation device. US Patent 10 751 244, 25 August 2020.
47. Yang R, Shi H, Yuan L, et al. A wearable soft hand functional rehabilitation glove. CN Patent 111 821 140, 27 October 2020.
48. Liu D, Wang M, Bi C, et al. A wearable finger rehabilitation device with a combination of rigid and soft activation and its manufacturing method. CN Patent 110 772 402, 11 February 2020.
49. Hu D, Zhang J, Yang Y, et al. A novel soft robotic glove with positive-negative pneumatic actuator for hand rehabilitation. In: 2020 IEEE/ASME international conference on advanced intelligent mechatronics (AIM), Boston, MA, 6–9 July 2020. New York: IEEE.
50. Yun SS, Kang BB, Cho KJ. Exo-Glove PM: an easily customizable modularized pneumatic assistive glove. IEEE Robot Autom Lett 2017; 2(3): 1725–1732.
51. Heung KHL, Tong RKY, Lau ATH, et al. Robotic glove with soft-elastic composite actuators for assisting activities of daily living. Soft Robot 2019; 6(2): 289–304.
52. Heung K, Tong Z, Ho L, et al. Design of a 3D printed soft robotic hand for stroke rehabilitation and daily activities assistance. In: 2019 IEEE 16th international conference on rehabilitation robotics (ICORR), Toronto, ON, 24–28 June 2019, pp.65–70. New York: IEEE.
53. Connolly F, Polygerinos P, Walsh CJ, et al. Mechanical programming of soft actuators by varying fiber angle. Soft Robot 2015; 2(1): 26–32.
54. Polygerinos P, Wang Z, Overvelde JTB, et al. Modeling of soft fiber-reinforced bending actuators. IEEE Trans Robot 2015; 31(3): 778–789.
55. Wang B, McDaid A, Aw K, et al. Design and development of a skinny bidirectional soft glove for post-stroke hand rehabilitation. In: 2017 intelligent systems conference (IntelliSys), London, 7–8 September 2017, pp.979–987. New York: IEEE.
56. Ramos O, Múnera M, Moazen M, et al. Assessment of soft actuators for hand exoskeletons: pleated textile actuators and fiber-reinforced silicone actuators. Front Bioeng Biotechnol 2022; 10: 924888.
57. Lin M, Paul R, Abd M, et al. Feeling the beat: a smart hand exoskeleton for learning to play musical instruments. Front Rob AI 2023; 10: 1212768.
58. Wang Y, Kokubu S, Zhou Z, et al. Designing soft pneumatic actuators for thumb movements. IEEE Robot Autom Lett 2021; 6(4): 8450–8457.
59. Tarvainen T, Fernandez-Vargas J, Yu W. New layouts of fiber reinforcements to enable full finger motion assist with pneumatic multi-chamber elastomer actuators. Actuators 2018; 7(2): 31.
60. Meng M. A hand-assisted rehabilitation drive. CN Patent 110 840 706, 28 February 2020.
61. Cao X, Ma K, Jiang Z, et al. A soft robotic glove for hand rehabilitation using pneumatic actuators with jamming structure. In: 2021 40th Chinese control conference (CCC), Shanghai, China, 26-28 July 2021. New York: IEEE.
62. Zhang H, Kumar AS, Chen F, et al. Topology optimized multimaterial soft fingers for applications on grippers, rehabilitation, and artificial hands. IEEE/ASME Trans Mechatron 2019; 24(1): 120–131.
63. Meng M. Structural design of a soft hand functional rehabilitation robot glove. CN Patent 112 999 014, 22 June 2021.
64. Kladovasilakis N, Kostavelis I, Sideridis P, et al. A novel soft robotic exoskeleton system for hand rehabilitation and assistance purposes. Appl Sci 2022; 13(1): 553.
65. Meng N, Kun W, Mingxin L, et al. Design, analysis and experiment of finger soft actuator with nested structure for rehabilitation training. Adv Mech Eng 2020; 12(11): 1–15.
66. Sun ZS, Guo ZH, Tang W. Design of wearable hand rehabilitation glove with soft hoop-reinforced pneumatic actuator. J Central South Univ 2019; 26: 106–119.
67. Polygerinos P, Wang Z, Galloway KC, et al. Soft robotic glove for combined assistance and at-home rehabilitation. Robot Auton Syst 2015; 73: 135–143.
68. Li Z, Lv H, Li Q. An articulated soft body rehabilitation robot glove. CN Patent 113 332 104, 3 September 2021.
69. Gaylord R. Fluid actuated motor system and stroking device. US Patent 2 844 126, 22 July 1958.
70. Daerden F, Lefeber D. Pneumatic artificial muscles: actuators for robotics and automation. Eur J Mech Env Eng 2002; 47: 11–21.
71. Baldwin HA. Realizable models of muscle function. In Biomechanics: Proceedings of the first rock island arsenal biomechanics symposium april 5–6, 1967. Springer, New York, 1969, pp.139–147.
72. Andrikopoulos G, Nikolakopoulos G, Manesis S. Pneumatic artificial muscles: a switching model predictive control approach. Control Eng Pract 2013; 21(12): 1653–1664.
73. Andrikopoulos G, Nikolakopoulos G, Manesis S. Design and development of an exoskeletal wrist prototype via pneumatic artificial muscles. Meccanica 2015; 50(11): 2709–2730.
74. Takosoglu JE, Laski PA, Blasiak S, et al. Determining the static characteristics of pneumatic muscles. Meas Control 2016; 49(2): 62–71.
75. Al-Fahaam H, Davis S, Nefti-Meziani S. The design and mathematical modelling of novel extensor bending pneumatic artificial muscles (EBPAMs) for soft exoskeletons. Robot Auton Syst 2018; 99: 63–74.
76. Peng G, Fan X, Liu X, et al. Design and control of flexible wearable rehabilitation gloves. Med Biomech 2019; 34(6): 637–643.
77. Takahashi N, Furuya S, Koike H. Soft exoskeleton glove with human anatomical architecture: production of dexterous finger movements and skillful piano performance. IEEE Trans Haptics 2020; 13(4): 679–690.
78. Wang J, Liu Z, Fei Y. Design and testing of a soft rehabilitation glove integrating finger and wrist function. J Mech Robot 2019; 11(1): 011015.
79. Maldonado-Mejía JC, Múnera M, Diaz CAR, et al. A fabric-based soft hand exoskeleton for assistance: the exhand exoskeleton. Front Neurorobot 2023; 17: 1091827.
80. Elmoughni HM, Yilmaz AF, Ozlem K, et al. Machine-knitted seamless pneumatic actuators for soft robotics: design, fabrication, and characterization. Actuators 2021; 10(5): 94.
81. Yap HK, Khin PM, Koh TH, et al. A fully fabric-based bidirectional soft robotic glove for assistance and rehabilitation of hand impaired patients. IEEE Robot Autom Lett 2017; 2(3): 1383–1390.
82. Feng M, Yang D, Gu G. High-force fabric-based pneumatic actuators with asymmetric chambers and interference-reinforced structure for soft wearable assistive gloves. IEEE Robot Autom Lett 2021; 6(2): 3105–3111.
83. Ge L, Chen F, Wang D, et al. Design, modeling, and evaluation of fabric-based pneumatic actuators for soft wearable assistive gloves. Soft Robot 2020; 7(5): 583–596.
84. Jeong U, In HK, Cho KJ. Implementation of various control algorithms for hand rehabilitation exercise using wearable robotic hand. Intell Serv Robot 2013; 6(4): 181–189.
85. Aoun A, Lliovits A, Kassem A, et al. Arthro-Glove a hybrid bionic glove for patients diagnosed with arthritis, als and/or dysmorphia. In: 2018 9th Cairo international biomedical engineering conference (CIBEC), Cairo, Egypt, 20–22 December 2018, pp.106–109. New York: IEEE.
86. Xu D, Wu Q, Zhu Y. Development of a soft cable-driven hand exoskeleton for assisted rehabilitation training. Ind Rob 2021; 48(2): 189–198.
87. Alnajjar F, Umari H, Ahmed WK, et al. CHAD: compact hand-assistive device for enhancement of function in hand impairments. Robot Auton Syst 2021; 142: 103784.
88. Biggar S, Yao W. Design and evaluation of a soft and wearable robotic glove for hand rehabilitation. IEEE Trans Neural Syst Rehabil Eng 2016; 24(10): 1071–1080.
89. Serrano D, Copaci D, Arias J, et al. SMA-based soft exo-glove. IEEE Robot Autom Lett 2023; 8(9): 5448–5455.
90. Abdelhafiz MH, Andreasen Struijk LNS, Dosen S, et al. Biomimetic tendon-based mechanism for finger flexion and extension in a soft hand exoskeleton: design and experimental assessment. Sensors 2023; 23(4): 2272.
91. Chen W, Li G, Li N, et al. Soft exoskeleton with fully actuated thumb movements for grasping assistance. IEEE Trans Robot 2022; 38(4): 2194–2207.
92. Tran P, Jeong S, Lyu F, et al. FLEXotendon Glove-iii: voice-controlled soft robotic hand exoskeleton with novel fabrication method and admittance grasping control. IEEE/ASME Trans Mechatron 2022; 27(5): 3920–3931.
93. Kang B, Lee H, In H, et al. Development of a polymer-based tendon-driven wearable robotic hand. In: 2016 IEEE International Conference on Robotics and Automation (ICRA), Stockholm, 16–21 May 2016, pp.3750–3755. New York: IEEE.
94. Kin D, Heo S, Park H. Biomimetic finger extension mechanism for soft wearable hand rehabilitation devices. In: 2017 international conference on rehabilitation robotics (ICORR), London, 17–20 July 2017, pp.1326–1330. New York: IEEE.
95. Setiawan JD, Ariyanto M, Nugroho S, et al. Fuzzy logic control for a soft exoskeleton glove using a motor-tendon actuator. Ing Invest 2021; 41(1): e81531.
96. Tang D, Lv X, Qi L, et al. A tendon wire driven exoskeleton for functional hand rehabilitation. CN Patent 115 284 261, 4 November 2022.
97. Mohammadi A, Lavranos J, Choong P, et al. Flexo-glove: a 3D printed soft exoskeleton robotic glove for impaired hand rehabilitation and assistance. In: 2018 40th annual international conference of the IEEE engineering in medicine and biology society (EMBC), Honolulu, HI, 18–21 July 2018, pp.2120–2123. New York: IEEE.
98. Liu A, Qiu J, Wang F, et al. An adaptive and jointless hand exoskeleton system design. In: 2018 15th international conference on control, automation, robotics and vision (ICARCV), Singapore, 18–21 November 2018, pp.579–584. New York: IEEE.
99. Arata J, Ohmoto K, Gassert R, et al. A new hand exoskeleton device for rehabilitation using a three-layered sliding spring mechanism. In: 2013 IEEE international conference on robotics and automation, Karlsruhe, Germany, 6–10 May 2013, pp.3902–3907. New York: IEEE.
100. Nazari V, Pouladian M, Zheng YP, et al. A compact and lightweight rehabilitative exoskeleton to restore grasping functions for people with hand paralysis. Sensors 2021; 21(20): 6900.
101. Lin L, Zhang F, Yang L, et al. Design and modeling of a hybrid soft-rigid hand exoskeleton for poststroke rehabilitation. Int J Mech Sci 2021; 212: 106831.
102. Bützer T, Lambercy O, Arata J, et al. Fully wearable actuated soft exoskeleton for grasping assistance in everyday activities. Soft Robot 2021; 8(2): 128–143.
103. Gerez L, Gao G, Dwivedi A, et al. A hybrid, wearable exoskeleton glove equipped with variable stiffness joints, abduction capabilities, and a telescopic thumb. IEEE Access 2020; 8: 173345–173358.
104. Stilli A, Cremoni A, Bianchi M, et al. Airexglove – a novel pneumatic exoskeleton glove for adaptive hand rehabilitation in post-stroke patients. In: 2018 IEEE international conference on soft robotics (RoboSoft), Livorno, Italy, 24–28 April 2018, pp.579–584. New York: IEEE.
105. Tang D, Qi L, Shen C, et al. A flexible hand rehabilitation exoskeleton and its control method. CN Patent 116 650 285, 29 August 2023.
106. Cho KJ, Koh JS, Kim S, et al. Review of manufacturing processes for soft biomimetic robots. Int J Precis Eng Manuf 2009; 10: 171–181.
107. Yap H, Goh J, Yeow R. Design and characterization of soft actuator for hand rehabilitation application. In: 6th European conference of the international federation for medical and biological engineering, Dubrovnik, Croatia, 7–11 September 2014, vol. 45, pp.367–370.
108. Yirmibesoglu O, Menguc Y. Hybrid soft sensor with embedded imus to measure motion. In: 2016 IEEE international conference on automation science and engineering (CASE), Fort Worth, TX, 21–25 August 2016, pp.798–804. New York: IEEE.
109. Sun Y, Song S, Liang X, et al. A miniature soft robotic manipulator based on novel fabrication methods. IEEE Robot Autom Lett 2016; 1(2): 617–623.
110. Gong Z, Xie Z, Yang X, et al. Design, fabrication and kinematic modeling of a 3D-motion soft robotic arm. In: 2016 IEEE international conference on robotics and biomimetics (ROBIO), Qingdao, China, 3–7 December 2016, pp.509–514. New York IEEE.
111. Wallin TJ, Pikul J, Shepherd RF. 3D printing of soft robotic systems. Nat Rev Mater 2018; 3: 84–100.
112. Hinton TJ, Jallerat Q, Palchesko RN, et al. Three-dimensional printing of complex biological structures by freeform reversible embedding of suspended hydrogels. Sci Adv 2015; 1(9): e1500758.
113. Nyberg EL, Farris AL, Hung BP, et al. 3D-printing technologies for craniofacial rehabilitation, reconstruction, and regeneration. Ann Biomed Eng 2017; 45(1): 45–57.
114. Wolf SL, Blanton S, Baer H, et al. Repetitive task practice: a critical review of constraint-induced movement therapy in stroke. Neurologist 2002; 8(6): 325–338.
115. Altschuler EL, Wisdom SB, Stone L, et al. Rehabilitation of hemiparesis after stroke with a mirror. Lancet 1999; 353(9169): 2035–2036.
116. Boos A, Qiu Q, Fluet G, et al. Haptically facilitated bimanual training combined with augmented visual feedback in moderate to severe hemiplegia. In: 2011 annual international conference of the IEEE engineering in medicine and biology society, Boston, MA, 30 August–3 September 2011, pp.3111–3114. New York: IEEE.
117. Kim SY, Kim YY. Mirror therapy for phantom limb pain. Korean J Pain 2012; 25(4): 272–274.
118. Chen X, Gong L, Wei L, et al. A wearable hand rehabilitation system with soft gloves. IEEE Trans Ind Inform 2021; 17(2): 943–952.
119. Li M, Wang T, Zhou Y, et al. A soft robotic glove for hand rehabilitation training controlled by movements of the healthy hand. In: 2020 17th International Conference on Ubiquitous Robots (UR), Kyoto, Japan, 22–26 June 2020. New York: IEEE.
120. Moraru E, Onose G. Current issues and considerations about the central role of rehabilitation therapies in the functional recovery of neurological impairments after stroke in adults. J Med Life 2014; 7(3): 368–372.
121. Harvey RL. Improving poststroke recovery: neuroplasticity and task-oriented training. Curr Treat Options Cardiovasc Med 2009; 11(3): 251–259.
122. Hoang CL, Salle JY, Mandigout S, et al. Physical factors associated with fatigue after stroke: an exploratory study. Top Stroke Rehabil 2012; 19(5): 369–376.
123. Bates B, Choi JY, Duncan PW, et al.; US Department of Defense and Department of Veterans Affairs. Veterans affairs/department of defense clinical practice guideline for the management of adult stroke rehabilitation care: executive summary. Stroke 2005; 36(9): 2049–2056.
124. Merians AS, Jack D, Boian R, et al. Virtual reality–augmented rehabilitation for patients following stroke. Phys Ther Rehabil 2002; 82(9): 898–915.
125. Holden MK. Virtual environments for motor rehabilitation: review. Cyberpsychol Behav 2005; 8(3): 187–211.
126. Connelly L, Jia Y, Toro ML, et al. A pneumatic glove and immersive virtual reality environment for hand rehabilitative training after stroke. IEEE Trans Neural Syst Rehabil Eng 2010; 18(5): 551–559.
127. Merians AS, Fluet GG, Qiu Q, et al. Robotically facilitated virtual rehabilitation of arm transport integrated with finger movement in persons with hemiparesis. J Neuroeng Rehabil 2011; 8(1): 27–10.
128. Mitsopoulos K, Fiska V, Tagaras K, et al. Neurosuitup: system architecture and validation of a motor rehabilitation wearable robotics and serious game platform. Sensors 2023; 23(6): 3281.
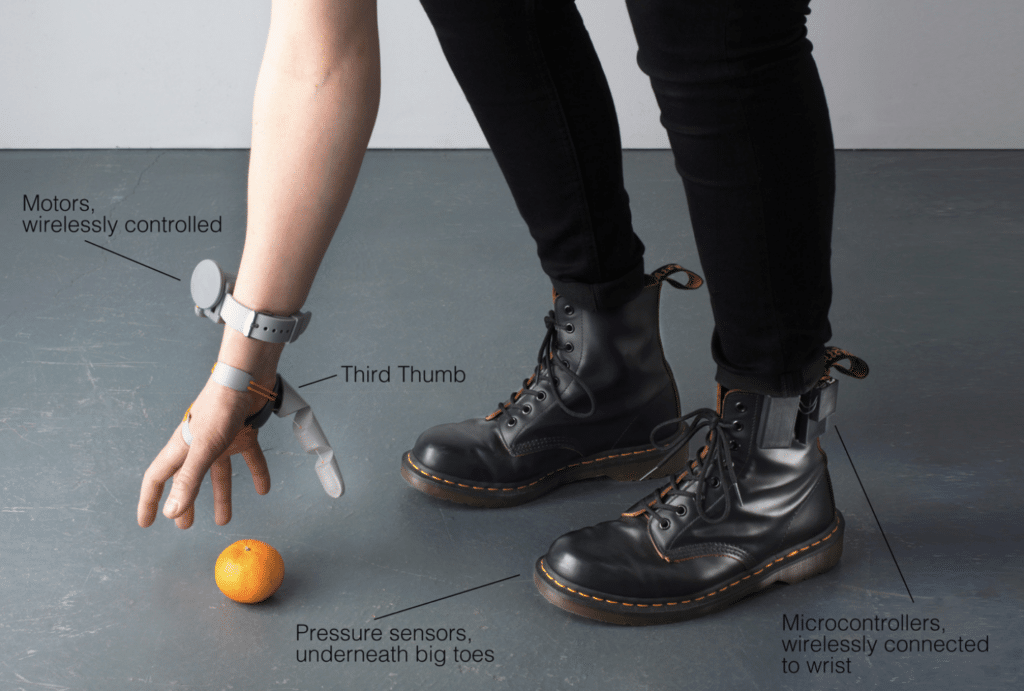
[WEB] This woman just created a robotic third thumb and it’s a total gamechanger
Posted by Kostas Pantremenos in Assistive Technology, Rehabilitation robotics on February 11, 2024

If you could have an extra body part, what would it be?
An augmentation designer has chosen a third thumb.
Sounds mad – and it looks it too – but it turns out an extra thumb would be pretty useful.
READ MORE! ‘World’s most advanced humanoid robot’ reveals what life will look like in 100 years
Designer Dani Clode developed a device called the ‘Third Thumb’ as part of a project at the Royal College of Art.
Clode wears the 3D-printed device on the side of the hand opposite her actual thumb near the pinky finger.
She then controls it with pressure sensors attached to her feet on the underside of the big toes.
Connected wirelessly, both toe sensors control different movements of the Third Thumb by immediately responding to subtle changes of pressure from the wearer.
To test the Third Thumb’s capability, a team from University College London were trained to use the device.
https://imasdk.googleapis.com/js/core/bridge3.619.0_en.html#goog_1293646367
417.3K
Water Firing Hypercar with NASA Technology | Hyperion
This involved focusing on tasks that helped increase the cooperation between their hand and the Third Thumb, such as picking up multiple balls or wine glasses with one hand.
They learned the basics of using the device very quickly, while the training enabled them to successfully improve their motor control, dexterity and hand-thumb coordination.
Participants were even able to use the device when distracted – building a wooden block tower while solving math problems – or while blindfolded.
So, it felt natural super quickly.


The project challenges the conventional idea of prosthetics by considering them as extensions rather than mere replacements.
A video posted to TikTok of the Third Thumb in action shows not everyone’s convinced, though.
“If we were meant to have six fingers, we would’ve been born with six fingers,” one user said.
“We’ve been fine without one for centuries. Why now?” another asked.
“People today don’t even know how to use their brain. What will they do with an extra finger?” another posted.
Some social media users suggested other body parts that would be more useful, like another pair or arms of even a tail.
Perhaps they’re projects for Clode to consider next.
[ARTICLE] Utilizing the intelligence edge framework for robotic upper limb rehabilitation in home – Full Text
Posted by Kostas Pantremenos in Paretic Hand, Rehabilitation robotics, Tele/Home Rehabilitation on February 4, 2024
Abstract
Robotic devices are gaining popularity for the physical rehabilitation of stroke survivors. Transition of these robotic systems from research labs to the clinical setting has been successful, however, providing robot-assisted rehabilitation in home settings remains to be achieved. In addition to ensure safety to the users, other important issues that need to be addressed are the real time monitoring of the installed instruments, remote supervision by a therapist, optimal data transmission and processing. The goal of this paper is to advance the current state of robot-assisted in-home rehabilitation. A state-of-the-art approach to implement a novel paradigm for home-based training of stroke survivors in the context of an upper limb rehabilitation robot system is presented in this paper. First, a cost effective and easy-to-wear upper limb robotic orthosis for home settings is introduced. Then, a framework of the internet of robotics things (IoRT) is discussed together with its implementation. Experimental results are included from a proof-of-concept study demonstrating that the means of absolute errors in predicting wrist, elbow and shoulder angles are 0.89180,2.67530 and 8.02580, respectively. These experimental results demonstrate the feasibility of a safe home-based training paradigm for stroke survivors. The proposed framework will help overcome the technological barriers, being relevant for IT experts in health-related domains and pave the way to setting up a telerehabilitation system increasing implementation of home-based robotic rehabilitation. The proposed novel framework includes:
- •A low-cost and easy to wear upper limb robotic orthosis which is suitable for use at home.
- •A paradigm of IoRT which is used in conjunction with the robotic orthosis for home-based rehabilitation.
- •A machine learning-based protocol which combines and analyse the data from robot sensors for efficient and quick decision making.
Graphical abstract


[WEB] Soft robo-glove can help stroke patients relearn to play music
Posted by Kostas Pantremenos in Music/Music therapy, Rehabilitation robotics on January 25, 2024
By Mischa Dijkstra, Frontiers science writer

Researchers have developed the prototype of a comfortable and flexible ‘soft smart hand exoskeleton’ or robo-glove, which gives feedback to wearers who need to relearn tasks that require manual dexterity and coordination, for example after suffering a stroke. The present study focused on patients who need to relearn to play the piano as a proof-of-principle, but the glove can easily be adapted to help relearn other daily tasks.
Stroke is the most important cause of disability for adults in the EU, which affects approximately 1.1 million inhabitants each year. After a stroke, patients commonly need rehabilitation to relearn to walk, talk, or perform daily tasks. Research has shown that besides physical and occupational therapy, music therapy can help stroke patients to recover language and motor function. But for people trained in music and who suffered a stroke, playing music may itself be a skill that needs to be relearned. Now, a study in Frontiers in Robotics and AI has shown how novel soft robotics can help recovering patients to relearn playing music and other skills that require dexterity and coordination.
“Here we show that our smart exoskeleton glove, with its integrated tactile sensors, soft actuators, and artificial intelligence, can effectively aid in the relearning of manual tasks after neurotrauma,” said lead author Dr Maohua Lin, an adjunct professor at the Department of Ocean & Mechanical Engineering of Florida Atlantic University.
Credit: Dr Maohua Lin et al
Whom the glove fits: custom-made ‘smart hand’
Lin and colleagues designed and tested a ‘smart hand exoskeleton’ in the shape of a multi-layered, flexible 3D-printed robo-glove, which weighs only 191g. The entire palm and wrist area of the glove are designed to be soft and flexible, and the shape of the glove can be custom-made to fit each wearer’s anatomy.
Soft pneumatic actuators in its fingertips generate motion and exert force, thus mimicking natural, fine-tuned hand movements. Each fingertip also contains an array of 16 flexible sensors or ‘taxels’, which give tactile sensations to the wearer’s hand upon interaction with objects or surfaces. Production of the glove is straightforward, as all actuators and sensors are put in place through a single molding process.
“While wearing the glove, human users have control over the movement of each finger to a significant extent,” said senior author Dr Erik Engeberg, a professor at Florida Atlantic University’s Department of Ocean & Mechanical Engineering.
“The glove is designed to assist and enhance their natural hand movements, allowing them to control the flexion and extension of their fingers. The glove supplies hand guidance, providing support and amplifying dexterity.”
The authors foresee that patients might ultimately wear a pair of these gloves, to help both hands independently to regain dexterity, motor skills, and a sense of coordination.
AI trained the glove to be a music teacher
The authors used machine learning to successfully teach the glove to ‘feel’ the difference between playing a correct versus incorrect versions of a beginner’s song on the piano. Here, the glove operated autonomously without human input, with preprogrammed movements. The song was ‘Mary had a little lamb’, which requires four fingers to play.
“We found that the glove can learn to distinguish between correct and incorrect piano play. This means it could be a valuable tool for personalized rehabilitation of people who wish to relearn to play music,” said Engeberg.
Now that the proof-of-principle has been shown, the glove can be programmed to give feedback to the wearer about what went right or wrong in their play, either through haptic feedback, visual cues, or sound. These would enable her or him to understand their performance and make improvements.
Picking up the gauntlet for remaining challenges
Lin added: “Adapting the present design to other rehabilitation tasks beyond playing music, for example object manipulation, would require customization to individual needs. This can be facilitated through 3D scanning technology or CT scans to ensure a personalized fit and functionality for each user.”
“But several challenges in this field need to be overcome. These include improving the accuracy and reliability of tactile sensing, enhancing the adaptability and dexterity of the exoskeleton design, and refining the machine learning algorithms to better interpret and respond to user input.”
REPUBLISHING GUIDELINES: Open access and sharing research is part of Frontiers’ mission. Unless otherwise noted, you can republish articles posted in the Frontiers news site — as long as you include a link back to the original research. Selling the articles is not allowed.
[Abstract + References] Effects of robotic-assisted gait training on physical capacity, and quality of life among chronic stroke patients: A randomized controlled study
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, Rehabilitation robotics on January 24, 2024
Abstract
Background
Even though robotic therapy is becoming more commonly used in research protocols for lower limb stroke rehabilitation, there still is a significant gap between research evidence and its use in clinical practice. Therefore, the present study was designed assuming that the wearable mobile gait device training for chronic stroke patients might have different effects on functional independence when compared to training with a stationary gait device. The present study aims to examine the effects of gait training with ExoAthlet exoskeleton and Lokomat Free-D on functional independence, functional capacity, and quality of life in chronic stroke patients.
Methods
The present study included 32 chronic stroke patients. Participants were randomly divided into two groups. Functional independence of patients was evaluated by using Functional Independence Measure (FIM), physical function was assessed by using the 30-second chair stand test (30-CST), functional capacity was measured by using the 6-Minute Walk Test (6MWT), and quality of life was assessed by using Short Form 36 (SF36). All participants underwent a conventional physiotherapy program for eight weeks, three sessions per week, and each session lasted 60 min. After the physiotherapy program, one group received gait training by using ExoAthlet exoskeleton (ExoAtlet 1 model/2019, Russia), while the other group received training by using Lokomat Free-D (Hocoma, Lokomat Pro Free-D model/2015, Switzerland). Participants were assessed at baseline and post-intervention.
Results
Results achieved in this study revealed that there was a statistically significant difference between FIM, 30-CST, 6MWT, and SF36 scores before and after the treatment in both groups (p < 0.05).There was no difference in FIM, 30-CST, and 6MWT results between Exoskeleton ExoAthlet and Lokomat Free-D groups (p > 0.05). However, there was a statistically significant difference between Exoskeleton ExoAthlet and Lokomat Free-D groups in terms of SF-36 sub-parameters “vitality”, “mental health”, “bodily pain”, and “general health perception” (p < 0.05).
Conclusions
This study demonstrated that the use of ExoAthlet exoskeleton and Lokomat Free-D in addition to conventional physiotherapy, was effective in improving functional independence, physical function, functional capacity, and quality of life among chronic stroke patients. Incorporation of robotic gait aids into rehabilitation for chronic stroke patients might offer significant advantages.
Introduction
Stroke is defined as a condition that develops due to a disturbance in brain functions, either in a specific location or in the whole brain, rapidly manifests symptoms, and these symptoms persist for one day or longer, or result in death [1]. Motor functions are affected in 65 % of chronic stroke patients, and the majority of these patients experience a reduced level of functional independence [2]. It is believed that the most prominent challenges faced by chronic stroke patients are the distance walked in 6 min and the decrease in functional capacity [3]. In addition, cohort studies also reported that 22 % of chronic stroke patients did not regain any walking function [4].
A significant portion of chronic stroke patients suffer not only from physical disability but also from cognitive and emotional disorders [5]. General predictors of the poor quality of life after a stroke were reported to include medical comorbidities, loss of physical function, social role difficulties, emotional involvement, and depression [6], [7], [8].
In recent years, robotic technology has exhibited notable advancement thanks to faster and more powerful computers, innovative computational methodologies, and a broader range of electromechanical components. This technological advancement also made robotics suitable for rehabilitation interventions, and robotic rehabilitation is a promising method for treating patients with motor disorders. Its significance lies in its the potential to increase and carefully control the dosage of therapy [9], [10]. However, robotic rehabilitation does not solely focus on augmenting the quantity and intensity of treatment.
Robotic systems not only generate simple and repetitive stereotypical movement patterns but can also be utilized in order to provide patients with more intricate and controlled multisensory stimuli [11]. It can be seen that the effect of rehabilitation technology on functional outcomes can be optimized by affording the nervous system greater opportunities to experience genuine activity-related sensorimotor input [12]. Nevertheless, there are ongoing studies examining the therapeutic effectiveness of robotic rehabilitation. In clinical rehabilitation practices addressing chronic stroke patients, robotic technologies are employed for gait training, providing opportunities to move freely on a stationary or mobile basis. Robotic devices are utilized as assistive, rehabilitative, and augmentative instruments in lower extremity rehabilitation for neurological conditions [13]. Considering the lower extremity rehabilitation, the Lokomat, utilized as a stationary device, was demonstrated to be effective in improving walking quality, speed, and balance in conditions such as Multiple Sclerosis, Cerebral Palsy, Parkinson’s disease, Brown-Sequard syndrome, and vascular dementia [14]. Moreover, Lokomat was also reported to be an effective approach used in the rehabilitation of chronic stroke patients. In the literature, a retrospective case-control study examined the efficacy of Lokomat Free-D on functional independence, functional capacity, and balance in chronic stroke patients [15]. It was also reported that Lokomat Free-D is effective in chronic stroke individuals, not only affecting motor functions such as walking, balance, muscle strength, walking ability, and speed but also cognitive and emotional status. [14]. However, to the best of our knowledge, there is no study examining the effectiveness of Lokomat on the quality of life in chronic stroke individuals could be found. Another method utilized for lower extremity rehabilitation is the use of mobile gait devices. Devices such as MIRAD, XoR, and ExoAthlet exoskeleton are some of them [13]. The ExoAthlet exoskeleton was found to increase gait speed and stability, as well as reducing body sway, in conditions such as Multiple Sclerosis and spinal cord injuries [16], [17]. In a randomized controlled study comparing ExoAthlet exoskeleton and traditional physiotherapy in chronic stroke patients, the ExoAthlet exoskeleton group exhibited significant improvements when compared to the traditional physiotherapy group. The ExoAthlet exoskeleton group had a decrease in hemiparesis severity, an increase in paretic limb muscle strength, improvement in balance, and notable enhancements in the walking process and speed [18]. However, there is no study available that examines the effectiveness of the ExoAthlet exoskeleton on quality of life in chronic stroke patients. In both literature and clinical practice, there are gaps concerning the effectiveness of Lokomat Free-D and ExoAthlet exoskeleton on different parameters. There is no study available that has comparing these two different methods among chronic stroke patients. Finally, this study aims to examine the effects of gait training with the ExoAthlet exoskeleton and Lokomat Free-D on functional independence, functional capacity, and quality of life in chronic stroke patients, as well as to investigate whether there are any different effects.
Section snippets
Study design and ethics
Study design: Randomized Controlled Study.
Ethics: The study protocol was approved by from the institutional ethics board of Üsküdar University’s Non-Interventional Ethics Committee (Approval no = 61351342/February 2021-66/26.02.2021). The present study was carried out in accordance with the principles outlined in the Declaration of Helsinki. Participants, who voluntarily agreed to participate in this study, signed a written consent form. The paper is registered with ClinicalTrials.gov, and the
Results
Initially, 40 chronic stroke patients were involved in the study, and 8 individuals did not meet the inclusion criteria. Thus, the study was completed with a total of 32 individuals. The flow chart of the study is presented in Fig. 3.
The sociodemographic characteristics of the chronic stroke patients included in the study are shown in Table 1.
The results of this study showed that there was a statistically significant difference between functional independence, functional capacity, and quality
Discussion
Significant advancements have been achieved in robotic technology, especially in the last ten years, and the use of robotic technology in healthcare has increased. The use of robotic technology increased in post-stroke rehabilitation due to its advantages such as performing movements very similar to normal activity, providing continuous stimulation of the central nervous system, and creating treatment options with appropriate intensity and dosage for the patient during the rehabilitation
Limitations and future directions
The study has some limitations. The long-term effects of robotic-assisted gait training were not evaluated in this study. Additionally, different psychometric properties that would affect the quality of life were ignored. Future studies taking these parameters into consideration may provide different perspectives on the interpretation of results.
Conclusion
In conclusion, the results achieved in this study showed that gait training with Exoskeleton ExoAthlete and gait training with Lokomat Free-D for eight weeks administered in addition to conventional physiotherapy have positive effects on functional independence, functional capacity, and quality of life parameters in post-stroke patients. Training with Exoskeleton ExoAthlet had a more positive effect on the quality-of-life sub-parameters, such as vitality, mental health, bodily pain, and general
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References (45)
- S. Wist et al.Muscle strengthening for hemiparesis after stroke: A meta-analysisAnn Phys Rehabil Med(2016)
- H.S. Jørgensen et al.Recovery of walking function in stroke patients: the Copenhagen Stroke StudyArch Phys Med Rehabil(1995)
- R.J. NudoFunctional and structural plasticity in motor cortex: implications for stroke recoveryPhysical Medicine and Rehabilitation Clinics(2003)
- I. Schwartz et al.The effectiveness of locomotor therapy using robotic-assisted gait training in subacute stroke patients: a randomized controlled trialPMR(2009)
- GBD. Stroke collaborators. global, regional, and national burden of stroke, 1990-2016: a systematic analysis for the…
- Clara Selves, Gaëtan Stoquart, Thierry Lejeune. Gait rehabilitation after stroke: review of the evidence of predictors,…
- J.P.L. Slenders et al.Early cognitive and emotional outcome after stroke is independent of discharge destinationJ Neurol(2020)
- G.O. Vincent-Onabajo et al.Consistent determinants of health-related quality of life in the first 12 months after stroke: a prospective study in NigeriaTop Stroke Rehabil(2015)
- A.C. Jonsson et al.Determinants of quality of life in stroke survivors andtheir informal caregiversStroke(2005)
- Samsa GP, Matchar DB. How strong is the relationshipbetween functional status and quality of life among personswith…
- A. Esquenazi et al.Robotic-assisted gait training and restorationAm J Phys Med Rehabil(2012)
- L. PignoloRobotics in neuro-rehabilitationJ Rehabil Med(2009)
- A.B. KeelingUnderstanding Stroke Rehabilitation Progression in a Robotic Rehabilitation TrialCumming School of Medicine(2020)
- H. Lee et al.Lower limb exoskeleton systems—overviewWearable Robotics(2020)
- R.S. Calabrò et al.Robotic gait rehabilitation and substitution devices in neurological disorders: where are we now?Neurol Sci(2016)
- A. Manuli et al.Calabrò RS.J Is intensive gait training feasible and effective at old age? A retrospective case-control study on the use of Lokomat Free-D in patients with chronic strokeClin Neurosci(2021 Oct)
- S.V. Kotov et al.The efficacy of the exoskeleton ExoAtlet to restore walking in patients with multiple sclerosis. Zhurnal nevrologii i psikhiatrii imeni SSKorsakova(2017)
- E.Y. Shapkova et al.Exoskeleton walk training in paralyzed individuals benefits from transcutaneous lumbar cord tonic electrical stimulationFront Neurosci(2020)
- S.V. Kotov et al.Efficiency of leg exoskeleton use in rehabilitation of cerebral stroke patientsSerbian journal of experimental and clinical research(2021)
- R. Mustafaoglu et al.Does robot-assisted gait training improve mobility, activities of daily living and quality of life in stroke? A single-blinded, randomized controlled trialActa Neurol Belg(2020)
- A.A. Küçükdeveci et al.Adaptation of the Functional Independence Measure for use in TurkeyClin Rehabil(2001)
- Mcleod JC, Ward SJ, Hicks AL. Evaluation of the Keeogo™ Dermoskeleton. Disabil Rehabil Assist Technol. 2019…
There are more references available in the full text version of this article.
