Posts Tagged biomechanics
[Abstract] Preliminary Design and Finite Element Analysis of A Low-Cost Wrist Rehabilitation Robot
Posted by Kostas Pantremenos in Paretic Hand, Rehabilitation robotics, Tele/Home Rehabilitation on February 6, 2023
Abstract:
Wrist rehabilitation robots are fundamental for helping patients with stroke or wrist injuries and also decrease the workload of physiotherapists. Though wrist rehabilitation robots are essential, recent wrist rehabilitation robots have shortcomings such as heavy weight, immobility, costliness, etc. To remedy these shortcomings, in this study, we developed and produced a low-cost and mobile robotic device for these patients with partial paralysis. The device is designed to assist the patient to perform wrist exercises comfortably in the home environment without being dependent on rehabilitation centers and/or physiotherapists. Therefore, we offer the device driven by a 3D-printed mechanism in two degrees of freedom. In addition, we analyzed and simulate the robot via finite element analysis and Solidworks respectively. The results indicate the robot provides enough force, torque, and range of motion. For these reasons, the robot can be used as a compact and lighter robot in hardware and a cheaper robot in cost. So it is feasible and affordable for real-time application in wrist rehabilitation.
[Abstract] EEG-EMG hybrid real-time classification of hand grasp and release movements intention in chronic stroke patients
Posted by Kostas Pantremenos in Paretic Hand, Rehabilitation robotics on October 31, 2022
Abstract
Rehabilitation of the hand motor function is essential for stroke patients to resume activities of daily living. Recent studies have shown that wearable robot systems, like a multi degree-of-freedom soft glove, have the potential to improve hand motor impairment. The rehabilitation system, which is intuitively controlled according to the user’s intention, is expected to induce active participation of the user and further promote brain plasticity. However, due to the patient-specific nature of stroke patients, extracting the intention from stroke patients is still challenging. In this study, we implemented a classifier that combines EEG and EMG to detect chronic stroke patients’ four types of intention: rest, grasp, hold, and release. Three chronic stroke patients participated in the experiment and performed rest, grasp, hold, and release actions. The rest vs. grasp binary classifier and release vs. hold binary classifier showed 76.9% and 86.6% classification accuracy in real-time, respectively. In addition, patient-specific accuracy comparisons showed that the hybrid approach was robust to upper limb impairment level compared to other approaches. We believe that these results could pave the way for the development of BCI-based robotic hand rehabilitation therapy.
[ARTICLE] ARMIA: A Sensorized Arm Wearable for Motor Rehabilitation – Full Text
Posted by Kostas Pantremenos in Paretic Hand, Virtual reality rehabilitation on July 4, 2022
Abstract
In this paper, we present ARMIA: a sensorized arm wearable that includes a combination of inertial and sEMG sensors to interact with serious games in telerehabilitation setups. This device reduces the cost of robotic assistance technologies to be affordable for end-users at home and at rehabilitation centers. Hardware and acquisition software specifications are described together with potential applications of ARMIA in real-life rehabilitation scenarios. A detailed comparison with similar medical technologies is provided, with a specific focus on wearable devices and virtual and augmented reality approaches. The potential advantages of the proposed device are also described showing that ARMIA could provide similar, if not better, the effectivity of physical therapy as well as giving the possibility of home-based rehabilitation.
1. Introduction
The number of people with motor disabilities has importantly increased in the last few years due to global aging and the general improvement of clinical care and health technology. For this reason, public and private health care systems are investing more in rehabilitation technologies. Recent events, such as the COVID-19 pandemic have stressed the importance of telerehabilitation both at home and at clinical facilities [1,2]. The use of telerehabilitation systems could avoid unnecessary physical contact between patients and therapists as well as enhance the rehabilitation process by increasing repeatability and intensity.
Upper limb motor impairment is one of the most limiting conditions for activities of daily living (ADLs), so an efficient rehabilitation is critical to recovering quality of life. This impairment can be caused by a variety of neuromuscular conditions such as stroke, spinal cord injury, neurodegenerative diseases, mistakes during surgery or aging. In the last few decades, a variety of robot-assisted technologies have been developed to outperform the efficacy of conventional manual therapies [3,4]. End-effector systems are the most typical devices to provide the patient with repetitive and continuous tasks. Examples of those are MIT-Manus [5], GENTLE [6] or, more recently, reachMAN2 [7]. Anthropomorphic devices such as upper limb exoskeletons are also common even though they are biomechanically more complex [8]. However, all these technologies are expensive and not affordable for particulars and for most rehabilitation centers.
Another key factor in upper limb motor rehabilitation is patient motivation. Studies on this behalf have been explored for many years to conclude that any motivational input increases the involvement of the patient in the requested motor tasks. For this purpose, a very common approach is the use of serious games, which are therapeutic leisure virtual activities to promote engagement. There are many applications of serious games to upper limb rehabilitation [9]. These applications can complement the use of assistive technologies. For instance, ArmAssist is a robotic device to improve arm mobility by using serious games [10], and VirtualRehab provides different interfaces for motor disabled individuals [11].
In addition to robot assistance, a good method to interact with these virtual environments is the sensorization of the patient. In the first stage, a common and simple way of performing this was using accelerometers to measure arm kinematics at the sagittal plane [12], but this did not allow inferring tridimensional information. With the development of modern inertial sensors (inertial measurement units, IMUs), it is now possible to characterize the whole arm kinematics with high precision. Moreover, kinematic metrics have a good correlation with conventional clinical scales, which provides an additional way of enhancing motor therapy [13]. Recent studies also show how ADLs can benefit from the application of this technology in rehabilitation [14,15]. Upper-limb motor rehabilitation can also benefit from the assessment of neuromuscular behavior. Surface electromyography (sEMG) allows for measuring electrical activity from the muscle contractions. This technique has been widely used to evaluate factors such as muscle fatigue [16] or movement coordination [17]. sEMG can also be used as input control for virtual environments by processing the activity of muscle contractions [18]. sEMG provides several advantages compared to other electrophysiological measurements, including non-invasiveness, real-time monitoring and on-site application with relatively affordable equipment.
In this paper, we present ARMIA: a sensorized arm wearable that includes a combination of inertial and sEMG sensors to interact with serious games in telerehabilitation setups. This device reduces the cost of robotic assistance technologies to be affordable for end-users at home and at rehabilitation centers. Hardware and acquisition software specifications are described together with potential applications of ARMIA in real-life rehabilitation scenarios. Similar wearable devices have already been applied in the telerehabilitation of specific body parts such as fingers [19] or the elbow [20]. In this case, ARMIA will provide rehabilitation to the whole arm by tracking upper-limb kinematics through inertial sensors. It also includes the real-time assessment of neuromuscular function by extracting meaningful biomarkers of motor control such as muscular fatigue. ARMIA is meant to be combined with virtual activities defined to track the whole rehabilitation process and optimize it based on the recorded physiological data.
2. Hardware
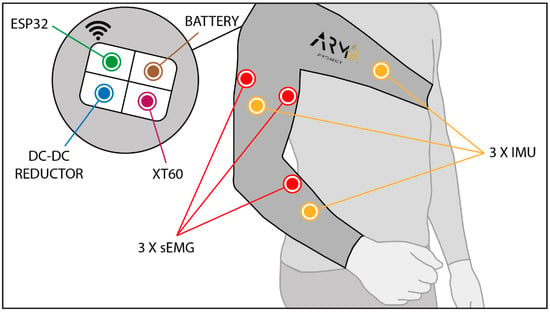
ARMIA is a sensorized sleeve that allows measuring kinematics and muscular activity during upper limb movements (Figure 1). In order to determine arm kinematics, three inertial sensors are placed on the kinematic chain: one on the thorax (reference), one on the arm and one on the forearm. These last two sensors provide arm link orientation and elbow and shoulder joint angles. ARMIA does not provide wrist orientation, but it is possible to obtain cartesian coordinates of the arm end effector (hand).
[Abstract] Fatigue analysis of upper limb rehabilitation based on surface electromyography signal and motion capture
Posted by Kostas Pantremenos in Fatigue, Paretic Hand, REHABILITATION on March 15, 2022
Abstract
At present, fatigue state monitoring of upper limb movement generally relies solely on surface electromyographic signal (sEMG) to identify and classify fatigue, resulting in unstable results and certain limitations. This paper introduces the sEMG signal recognition and motion capture technology into the fatigue state monitoring process and proposes a fatigue analysis method combining an improved EMG fatigue threshold algorithm and biomechanical analysis. In this study, the right upper limb load elbow flexion test was used to simultaneously collect the biceps brachii sEMG signal and upper limb motion capture data, and at the same time the Borg Fatigue Subjective and Self-awareness Scale were used to record the fatigue feelings of the subjects. Then, the fatigue analysis method combining the EMG fatigue threshold algorithm and the biomechanical analysis was combined with four single types: mean power frequency (MPF), spectral moments ratio (SMR), fuzzy approximate entropy (fApEn) and Lempel-Ziv complexity (LZC). The test results of the evaluation index fatigue evaluation method were compared. The test results show that the method in this paper has a recognition rate of 98.6% for the overall fatigue state and 97%, 100%, and 99% for the three states of ease, transition and fatigue, which are more advantageous than other methods. The research results of this paper prove that the method in this paper can effectively prevent secondary injury caused by overtraining during upper limb exercises, and is of great significance for fatigue monitoring.
[Abstract] Design of Lower Limb Exoskeleton for Stroke Patients Gait Rehabilitation – Conference Publication
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, Rehabilitation robotics on January 21, 2022
Abstract
The possible gap as the number of stroke patients outgrows the number of therapists encourages the development of the exoskeleton as a multiplier for the therapists. The objective of this study is to design a lower limb exoskeleton for stroke patients’ gait therapy. The design method was started with assessing previous studies, to search for design references and issues of the technology. The previous studies provide information on the brief history of the exoskeleton for gait rehabilitation as well as the various structural, mechanical, and control designs of exoskeletons. Based on the references, we design a simple lower limb exoskeleton and formulate the prototyping and testing plan, from CAD modeling, followed by 3D printing of the model, mockup testing, until prototyping and the clinical test of the prototype. This article describes the preliminary stage of exoskeleton design especially the design process and the results in the form of exoskeleton conceptual design and scale model 1:2. The scale model improves the efficacy of the design study.
Published in: 2021 International Conference on Radar, Antenna, Microwave, Electronics, and Telecommunications (ICRAMET)
[WEB PAGE] An Orthopedic Approach to the Hemiparetic Upper Limb: Understanding the Biomechanics and Pathoanatomy of the Shoulder.
Posted by Kostas Pantremenos in Paretic Hand on December 23, 2020
By Henry Hoffman
Before I co-founded Saebo, I was a practicing occupational therapist specializing in non-operative orthopedic medicine and manual therapy of the upper quadrant. While working at Burke Rehabilitation Hospital in White Plains, NY, part of my caseload was dedicated to orthopedic rehabilitation including the treatment of overhead athletes. Through the International Academy of Orthopedic Medicine (IAOM), I received my post-professional education training on diagnosis specific musculoskeletal management.
In addition to treating clients with orthopedic injuries, I had the blessed opportunity to periodically work with stroke survivors in the outpatient setting at Burke (which became the beginning of Saebo, but I will save that story for another time). While treating neurologically impaired clients, I found myself applying key orthopedic principles I developed during my training with the Academy. I believed (and still do) having an orthopedic background, coupled with a good understanding of evidenced based treatment for the neurologically impaired population, enhanced my therapeutic outcomes. Whether it was identifying a patient’s source of pain, performing joint specific mobiIization techniques, or providing appropriate strength training drills, my comprehensive ortho/neuro hybrid treatment approach was more successful with clinical outcomes than using traditional “neuro” based strategies alone.
Whether we are treating a young overhead athlete that reports pain and clicking during the cocking phase of throwing or a middle-aged stroke survivor who is unable to touch the back of his head due to a capsular pattern, licensed occupational and physical therapists must be knowledgeable in understanding the biomechanics and pathomechanics of the shoulder complex in order to properly examine and treat these conditions. Regardless of the diagnosis, subacromial pathologies are the same. Yes, the causal factors may be different, but mechanics are mechanics and lesion sites are lesion sites despite the pathogensis.
The purpose of today’s blog is to offer an introductory review of the bio- and pathomechanics of the glenohumeral joint and scapulothoracic articulation. By developing a better understanding of the shoulder, we as clinicians will be more suited to resolve the functional limitations of our clients and offer them an improved quality of life.
Biomechanics of Arm Elevation:
Arm elevation is the most important function of the shoulder. There are 3 types of arm elevation – flexion, abduction, and scaption (plane of the scapula). In order to perform full arm elevation, the glenohumeral, scapulothoracic (articulation), sternoclavicular, acromioclavicular joints along with the cervico-thoracic junction have to participate in a coordinated, concomitant, and smooth pattern.
Scapulohumeral Rhythm
Normal maximum shoulder elevation is 180 degrees. Traditional theorists feel the overall glenohumeral-scapulothoracic rhythm is a 2:1 ratio. Recent literature now suggests that the 2:1 ratio is not consistent across an entire arc of shoulder elevation. The first 30-60 degrees of elevation has been termed the setting phase. The scapula is seeking a position of stability in relation to the humerus during this phase. As the arm elevates, the scapula has the tendency to tip secondary to the weight. To prevent this, the trapezius and serratus anterior contract to stabilize the scapula. In addition, these 2 muscles combine to form a force couple that upwardly rotates the scapula. In this early phase, motion occurs primarily at the GHJ.
Note: Poppen and Walker report a 4:1 glenohumeral to scapulothroacic ratio during the first 25 degrees, thereafter, an almost equal 5:4 ratio occurs. Doody showed a 7:1 ratio during the first 30 degrees, thereafter, a 1:1 ration from 90-150.
In the middle 60 degrees, elevation phase, glenohumeral motion is about equal to scapulothoracic motion. The last 60 degrees, glenohumeral motion is again more than scapulothoracic motion (5:1). The final scapular motion is the result of clavicular rotation and elevation of the acromioclavicular joint.
Scapulothoracic Motion
Movement at the scapulothoracic articulation is important for normal biomechanics of the shoulder joint. Scapulothoracic rhythm is important because it (1) sets the most functional position of the GHJ, (2) prevents active insufficiency of the scapulohumeral muscles, and (3) allows for sufficient ROM between the humeral head and the subacromial space.
Arthokinematics
The glenoid fossa and the humeral head are incongruent surfaces. Rotation of the joint cannot take place as a pure spin, but requires that the motions of the humerus be accompanied by a combined rolling and gliding of the humeral head on the glenoid fossa in a direction opposite of the movement of the shaft of the humerus. The humeral head slides posteriorly and inferiorly in flexion, anteriorly and superiorly in extension, and inferiorly in abduction, and superiorly in adduction. In external rotation, the humeral head slides anteriorly and in internal rotation it slides posteriorly.
Muscles Contributing to Arm Elevation
Deltoid Muscle
The largest and most important glenohumeral muscle. As the humerus elevates, the translatory component of the deltoid as a whole increases joint compression. When the humerus is in the plane of the scapula, the anterior and middle deltoid are optimally aligned to produce elevation of the humerus. In this motion, the posterior deltoid primarily serves as a joint compressor.
Supraspinatus Muscle
The primary function of this muscle is abduction with the secondary motion being external rotation. It exerts maximum effort at approximately 30 degrees of abduction. The secondary functions of the supraspinatus are to compress the GHJ and to provide stability at the humerus during elevation.
Infraspinatus, Teres Minor, Subscapularis Muscles
The function of these muscles are to depress the humeral head and prevent superior impaction of the humeral head into the acromion. In addition, they provide muscular balance and help stabilize the joint capsule.
Latissmus Dorsi, Pectoralis Major, and Teres Major
Latest EMG studies are showing that during arm elevation, the above muscles are acting as humeral head depressors. In addition, the muscles function as stabilizers for the anterior capsule.
Upper and Lower Trapezius and Serratus Anterior Muscles
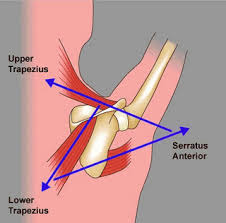
These muscles form a force couple that drives the scapula into upward rotation. In elevation, the force of the trapezius is more critical to the movement of upward rotation than the force of the serratus anterior. However, in order to perform full elevation both of these muscles must be firing.
Pathomechanics of Arm Elevation:
Prior to and following an orthopedic injury to the shoulder, pathologic changes take place. Because of this, normal mechanical behavior of the shoulder is substituted with asynchronous and faulty mechanics. Following a neurological injury (UMN lesion) damage to the sensory and motor areas of the cerebral cortex and brain stem may lead to primary impairments such as weakness, motor control, sensation, and tone. These clients often suffer from paralysis or abnormal tone in the muscles controlling their glenohumeral joint and scapula resulting in poor biomechanics which can lead to microtraumatic lesions. Therefore, an orthopedic or neurologic injury can cause the entire upper quadrant elevation chain to be affected.
When poor mechanics or soft tissue lesions are present, it is the clinician’s job to identify the source so proper treatment strategies can be provided. Below are examples of some of the common shoulder pathologies seen by orthopedic and neurologic clients:
Rotator Cuff Injuries
1. Subacromial Impingement – involves painful compression of one of the soft tissue structures located between the head of the humerus and the acromion, coracoacromial ligament, coracoid process, or AC joint. Impingement may occur due to structural narrowing (primary) or from underlying instability of the glenohumeral joint (secondary). Biomechanical changes after a neurological injury place affected clients at greater risk for impingement.
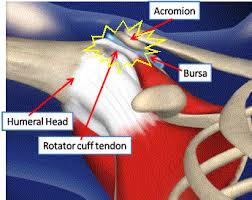
Note: Soft tissue structures that can be impinged:
- Supraspinatus
- Infraspinatus
- Subscapularis
- Teres minor
- Subacromial-subdeltoid bursa
- Joint capsule
- Long Head of Biceps tendon
2. Tensile Failure – repetitive eccentric overload of the rotator cuff muscles.
3. Internal Impingement – impingement of the soft tissues of the rotator cuff and joint capsule on the glenoid or between the glenoid and the humerus (i.e., overhead athlete).
Capsuloligamentous Injuries: result in partial separation of the humerus from the glenoid fossa. The rotator cuff is the primary stabilizing factor during mid range motions. At end range motions, the capsular ligaments become the stabilizing force. It is common for clients that performed repetitive overhead tasks to develop instability due to challenging the integrity of the ligaments. In addition, paralysis of the shoulder girdle due to a neurological injury may comprise the dynamic stability of the cuff muscles leading to an unstable joint.
3 Main Directions of Instability
- Anterior Instability: humeral head migrates excessively in an anterior direction relative to the glenoid.
- Inferior Instability: excessive inferior movement of the humeral head relative to the glenoid.
- Posterior Instability: excessive movement of the humeral head in a posterior direction relative to the glenoid.
The most common type of instability (subluxation) associated with hemiplegia is in an inferior direction. Inferior subluxations occur when muscle weakness leads to a downward rotation of the scapula in relation to the thorax. The labrum and inferior portion of the glenoid fossa can no longer provide sufficient support to secure the humeral head into the glenoid. In addition to the faulty mechanics at the scapula, the proximal migrators of the shoulder (deltoids) are no longer able to support the weight of the arm. Gravitational forces applied to the weakened arm stretches the inert and non-inert structures to the point that the humeral head migrates distally below the glenoid fossa.

Capsular Pattern (Frozen Shoulder):
Capsular pattern is synonymous with frozen shoulder, immobilization arthritis, and adhesive capsulitis. It consists of greater limitation of external rotation than abduction and a greater limitation of abduction than internal rotation, in a ratio of 3:2:1, respectively. Hemiparetic patients with limited movement often develop a capsular pattern (and pain) due to progressive adaptive changes to the collagen. Loss of motion occurs from thickening and contracture of the coracohumeral ligaments and rotator interval which prevents external rotation. As the pathology progresses, abduction and internal rotation are eventually affected as well.
It is not uncommon for neurological clients to report a painful shoulder while in therapy. For moderate to severely impaired clients who are unable to raise their arm mid range or higher, pain may result from spasticity and contractures. For mildly impaired clients that exhibit overhead active motion, pain may be due to compressive forces – primary or secondary impingement. This can come from mild weakness of the scapular or rotator cuff muscles or instability due to a previous subluxation event that resolved itself.
Although the above clinical pathologies are not inclusive, it does reflect some of the more commonly seen concerns in the clinic. Understanding the biomechanics and pathomechanics of the shoulder is paramount for proper musculoskeletal management. Clients suffering from an upper motor neuron lesion, with passive or active movement limitations will have some degree of pathomechanical issues. Therefore, clinicians must understand how the entire kinetic chain operates as a complete unit in order to improve upper limb function.
If you are a clinician who mainly treats neurologically impaired clients, seek out orthopedic based continuing education courses to enhance your clinical assessment and treatment skills. The added value of having a good understanding of the musculoskeletal system can be extremely significant when treating neurological clients suffering from joint pathology.
Henry graduated from D’Youville College in Buffalo, NY in 1997 with a Masters degree in Occupational Therapy. He has worked in a variety of clinical settings including home health, acute, sub-acute, and outpatient rehab. Prior to leaving Burke Rehabilitation Hospital in New York in 2002, he worked as a clinical specialist in orthopedic medicine and manual therapy of the Upper Quadrant. After leaving Burke, Henry co-founded Saebo with the goal of creating innovative and life changing solutions for the physically impaired population. He currently holds over 15 patents with products that have helped over 30,000 clients regain function. Saebo’s name is an acronym for Henry’s grandmother “Sarah Eileen Booth”. Her entire life was dedicated to providing a hand to others in need. Saebo’s mission is to match her spirit, dedication, and desire to help others.
[Abstract] Immediate kinematic and muscle activity changes after a single robotic exoskeleton walking session post-stroke
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, Rehabilitation robotics on November 28, 2020
ABSTRACT
Background: Robotic Exoskeletons (EKSO) are novel technology for retraining common gait dysfunction in people post-stroke. EKSO’s capability to influence gait characteristics post-stroke is unknown.
Objectives: To compare temporospatial, kinematic, and muscle activity gait characteristics before and after a single EKSO session and examine kinematic symmetry between involved and uninvolved limbs.
Methods: Participants post-stroke walked under two conditions: pre-EKSO, and immediately post-EKSO. A 10-camera motion capture system synchronized with 6 force plates was used to obtain temporospatial and kinematic gait characteristics from 5 walking trials of 9 meters at a self-selected speed. Surface EMG activity was obtained from bilateral gluteus medius, rectus femoris, medial hamstrings, tibialis anterior, and soleus muscles. Wilcoxon Signed Rank tests were used to analyze differences pre- and post-EKSO. Single EKSO session consisted of 22.3±6.8 minutes total time (walk time=7.2±1.5 minutes) with 250±40 steps.
Results: Six ambulatory (Functional Ambulation Category, range=4-5) adults (3 female; 44.7±14.6 years) with chronic stroke (4.5±1.9 years post-stroke) participated. No significant differences were observed for temporospatial gait characteristics. Muscle activity was significantly less post-EKSO in the involved leg rectus femoris during swing phase (p=0.028). Ankle dorsiflexion range of motion on the involved leg post-EKSO was significantly less during stance phase (p=0.046). Differences between involved and uninvolved joint range of motion symmetry were found pre-EKSO but not post-EKSO in swing phase hip flexion and stance phase knee flexion and knee extension.
Conclusions: EKSO training appears capable of altering gait in people with chronic stroke and a viable intervention to reduce gait dysfunction post-stroke.
[WEB PAGE] Starting with gait retraining: an analysis of changes in impact over time
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, REHABILITATION on July 17, 2020
By the Biomechanics of Human Movement research group of Ghent University

Figure 1. A subject running indoors at 11.5 km/h while wearing an interactive biofeedback system. The music-based biofeedback was played through a headphone.
The repetitive impact that is experienced upon collision with the ground may be related to running injuries but is modifiable. Lower-impact running can be achieved by receiving biofeedback in response to the peak tibial acceleration, but when are runners adapting to lower-impact running? Ten runners with high impact, herein defined as the peak tibial acceleration, ran 25 minutes on an athletic track in the Flanders Sports Arena. They were equipped with a wearable biofeedback system that accurately measures, monitors, and sonifies the impact in real-time. The system consists of 2 lightweight accelerometers, which attach to each leg of the runner, and an application hidden in a backpack for the provision of perceivable music-based biofeedback.
A change-point analysis was used to detect any change in impact (see Figure 2). No changes occurred whilst running without the biofeedback. The impact changed in the biofeedback condition. The major change was a reduction in impact, which occurred after almost 700 strides or after about 8 minutes. However, the time needed to achieve the major reduction varied considerably between the runners.
The simple analysis tool can aid physicians seeking to determine the timing effects of gait retraining by means of biofeedback on impact loading. Because of the rather quick response to the gait retraining due to a strong sensorimotor coupling, Pieter Van den Berghe PhD and colleagues want to highlight the potential of an autonomous biofeedback system that provides real-time and auditory feedback for lower-impact running.
The Biomechanics of Human Movement research group focuses on understanding the neuromechanical interaction of the moving body and the environment to answer questions related to the optimization of learning processes, sports performance, and musculoskeletal loading. A research project focusing on overground running retraining by means of auditory biofeedback was initiated together with the institute for systematic musicology IPEM.
Source: Van den Berghe P, Gosseries M, Gerlo J, Lenoir M, Leman M, De Clercq D. Change-point detection of peak tibial acceleration in overground running retraining. Sensors. 2020;20(6):1720.

Figure 2. The temporal evolution in axial peak tibial acceleration of a participant. More details are given in the article published in Sensors’ special issue, Sensors for Biomechanics Application.
[Abstract] Improving Walking Ability in People With Neurologic Conditions: A Theoretical Framework for Biomechanics-Driven Exercise Prescription.
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, REHABILITATION on December 19, 2019
Abstract
The purpose of this paper is to discuss how knowledge of the biomechanics of walking can be used to inform the prescription of resistance exercises for people with mobility limitations. Muscle weakness is a key physical impairment that limits walking in commonly occurring neurologic conditions such as cerebral palsy, traumatic brain injury, and stroke. Few randomized trials to date have shown conclusively that strength training improves walking in people living with these conditions. This appears to be because
(1) the most important muscle groups for forward propulsion when walking have not been targeted for strengthening, and
(2) strength training protocols have focused on slow and heavy resistance exercises, which do not improve the fast muscle contractions required for walking.
We propose a theoretical framework to improve exercise prescription by integrating the biomechanics of walking with the principles of strength training outlined by the American College of Sports Medicine to prescribe exercises that are specific to improving the task of walking. The high angular velocities that occur in the lower limb joints during walking indicate that resistance exercises targeting power generation would be most appropriate. Therefore, we propose the prescription of plyometric and ballistic resistance exercise, applied using the American College of Sports Medicine guidelines for task specificity, once people with neurologic conditions are ambulating, to improve walking outcomes. This new theoretical framework for resistance training ensures that exercise prescription matches how the muscles work during walking.
[Abstract] DESIGN AND DEVELOPMENT OF A NEW APPROACH TO WRIST REHABILITATION
Posted by Kostas Pantremenos in Paretic Hand on September 28, 2019
Abstract
Wrist injuries are a very common type of pathology that can compromise most daily
tasks. Conventional therapy is dependent on the availability of physiotherapists as well as devices
designed for this purpose. Conventional devices do not accompany the patient throughout their
rehabilitation process, requiring their constant replacement. Vibratory therapies emerged in recent
years and have demonstrated several benefits in this area. However, there are few vibratory
devices designed for wrist rehabilitation. In this paper, we propose two different portable and
active models for wrist rehabilitation based on vibratory therapy for wrist rehabilitation. The first
model has a cylindrical shape and the second model has a dumbbell shape. The results obtained
showed that vibratory therapy can assist the wrist rehabilitation because it promoted
improvements in joint amplitude gain in all wrist movements. Furthermore, the second device
demonstrated higher joint gains than the first device. In addition, the results obtained from the
measurement of accelerations demonstrate that the natural frequencies of both devices are
adequate for wrist and forearm rehabilitation as well as the mode of vibration. There are
differences between what the simulations predicted and what was obtained in practice in terms of
natural frequency values.

