Posts Tagged Shoulder
[Abstract] Design and Development of an Advanced Upper Limb Rehabilitation Robot for Post-Stroke Rehabilitation
Posted by Kostas Pantremenos in Paretic Hand, REHABILITATION, Rehabilitation robotics on January 17, 2024
Abstract
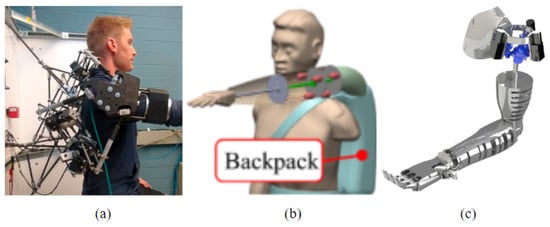
This research focuses on the design and development of an Upper Limb Rehabilitator (ULR) prototype, which aims to enhance stroke recovery. The study begins with a comprehensive review of existing upper limb rehabilitation robots such as the MIT-MANUS, ARMin, and the Robotic Rehabilitation Device (RRD). By analyzing ULR features and control systems, the research constructs a Product Design Specification (PDS) to guide the development of the ULR concept. To ensure structural integrity, governing equations are employed to calculate maximum stresses and safety factors for critical components. Material selection is based on these constraints, utilizing Ashby’s plots, and validating the choices through finite element analysis (FEA) simulations. Upon fabrication, the ULR prototype underwent performance testing, demonstrating notable improvements over the RRD. It achieves increased shoulder adduction and abduction angles of 14° and 10°, respectively, and enables a broader range of motion, including arm rotation, shoulder flexion, and elbow flexion and extension in three-dimensional planes during ULR prototype testing. The research highlights the significance of the ULR prototype in advancing upper limb rehabilitation robotics. It offers a versatile and effective rehabilitation tool, particularly during the critical recovery window. The findings provide valuable insights into the design and development process of the ULR, and its superior capabilities in rehabilitation motion.
Published in: 2023 6th International Conference on Applied Computational Intelligence in Information Systems (ACIIS)
[REVIEW] A Review of Parallel Robots: Rehabilitation, Assistance, and Humanoid Applications for Neck, Shoulder, Wrist, Hip, and Ankle Joints
Posted by Kostas Pantremenos in REHABILITATION, Rehabilitation robotics on November 7, 2023
Abstract
This review article presents an in-depth examination of research and development in the fields of rehabilitation, assistive technologies, and humanoid robots. It focuses on parallel robots designed for human body joints with three degrees of freedom, specifically the neck, shoulder, wrist, hip, and ankle. A systematic search was conducted across multiple databases, including Scopus, Web of Science, PubMed, IEEE Xplore, ScienceDirect, the Directory of Open Access Journals, and the ASME Journal. This systematic review offers an updated overview of advancements in the field from 2012 to 2023. After applying exclusion criteria, 93 papers were selected for in-depth review. This cohort included 13 articles focusing on the neck joint, 19 on the shoulder joint, 22 on the wrist joint, 9 on the hip joint, and 30 on the ankle joint. The article discusses the timeline and advancements of parallel robots, covering technology readiness levels (TRLs), design, the number of degrees of freedom, kinematics structure, workspace assessment, functional capabilities, performance evaluation methods, and material selection for the development of parallel robotics. It also examines critical technological challenges and future prospects in rehabilitation, assistance, and humanoid robots.
Keywords:
assistance; exoskeletons; parallel robots; prosthetics; rehabilitation
1. Introduction
Rehabilitation and assistance for human body joints play crucial roles in people’s health, well-being, and quality of life. These activities are essential for helping individuals recover or improve their functionality, mobility, and autonomy following injuries, surgeries, or diseases affecting the joints. In recent years, technological advances have opened up new possibilities in the use of parallel robots in the fields of rehabilitation, assistive technologies, and humanoid systems. These robotic systems are specifically designed to facilitate the recovery of motor and functional skills. Featuring a parallel mechanical structure, these robots offer greater precision, stability, and adaptability to meet the individual rehabilitation or assistance needs of patients.
Rehabilitation technologies aid in the recovery or improvement of motor function after an injury or illness. Utilizing parallel robots in rehabilitation enables specialists to help patients regain strength and mobility in affected joints more rapidly and efficiently than traditional therapeutic methods. The scope of these technologies includes rehabilitation devices for patients with head and neck injuries [1,2,3,4]; pediatric rehabilitation devices for the arm [5]; wearable rehabilitation devices for the arm [6]; exoskeletons for the arms of patients with stroke and spinal cord injuries [7]; and devices specifically designed for wrist [8,9,10], ankle [11,12,13,14,15,16], and foot rehabilitation [17].
Parallel robots in assistive devices help individuals carry out activities of daily life, thereby providing greater autonomy and independence. Examples include prostheses designed to offer functional mobility by replacing missing limbs in amputees [18], as well as shoulder disarticulation arm prostheses [19,20], wrist prostheses [21], and disarticulated hip prostheses [22].
The integration of humanoid robots into medical rehabilitation and assistance offers exciting opportunities. These include personalized therapy, precise motivation and tracking, assisted mobility, and the objective assessment of patients’ progress.
Parallel robots have advanced significantly in the fields of architectural [23] and mathematical modeling, particularly in kinematic [24,25,26] and dynamic analyses [27]. These robots can move at high speeds due to their lightweight and simple structural design [28]. They are also highly rigid, making them ideal for tasks requiring substantial force or pressure [29]. Their high-precision design minimizes unwanted movements and vibrations [30]. Furthermore, they can support heavier loads [31,32] and offer better positioning accuracy due to their high rigidity and low weight, which ensure minimal deformation [33]. Utilizing sensor technology and control algorithms, these parallel robots can automatically adjust to meet each patient’s specific needs, whether for rehabilitation or assistance, thus delivering a highly personalized experience.
However, there is a gap in the current literature concerning the use of parallel robots in the fields of rehabilitation, assistance, and humanoid systems. This review aims to address this gap by summarizing the available evidence on the utilization of parallel robots.
Therefore, this article aims to review the state of parallel robot technology as applied to rehabilitation, assistance, and humanoid systems, focusing on joints with three degrees of freedom in the human body: the neck, shoulder, wrist, hip, and ankle. Initially, the search strategy, inclusion and exclusion criteria, quality assessment, and data extraction methods are defined. Subsequently, the search results are presented, along with a detailed description of the biomechanics of the joints, parallel robots, and applications in the medical field. The article then discusses the timeline and advancements of parallel robots between 2012 and 2023 and examines the technology readiness levels (TRLs), design, number of degrees of freedom, kinematics structure, workspace assessment, functional capabilities, performance methods, and material selection in the development of parallel robotics, as well as the critical technological challenges and future prospects in rehabilitation, assistance, and humanoids. Finally, conclusions are presented. […]
[Textbook] Orthopedic Rehabilitation – Principles and Practice
Posted by Kostas Pantremenos in Books, Educational, REHABILITATION on August 12, 2023
Editors: Tony K. George, S. Ali Mostoufi, Alfred J. Tria Jr.
- A concise, practical guide to the principles and practice of orthopedic rehabilitation for residents and fellows
- Utilizes a consistent chapter format, arranged anatomically and covering each joint
- Written and edited by experts in both the orthopedic and physical medicine field
Sections
- Table of contents
- About this book
- Keywords
- Editors and Affiliations
- About the editors
- Bibliographic Information
This is a preview of subscription content, access via your institution.
Table of contents (11 chapters)
- Rehabilitation Principles for Interventional Orthopedics and Orthobiologics
- Walter I. Sussman, Marc P. Gruner, David R. Bakal, Kenneth R. Mautner
- Rehabilitation of Cervical Spine Disorders
- Laurent Delaveaux, Matthew Thomas, Brielle Hansen, Tony K. George
- Rehabilitation of Thoracic Spine Disorders
- Tony K. George, Sneha Varghese, Mindy Chu, Brittney Tout, Hemant Kalia
- Rehabilitation of Lumbar Spine Disorders
- Tony K. George, Matthew Thomas, Sruthi Nanduri, Liya Thomas, Wayne Bonkowski, Bobby Oommen
- Rehabilitation of Shoulder Disorders
- William Micheo, Anthony Lombardi, Claudia Jimenez
- Rehabilitation of Elbow Disorders
- Robert Bowers, Joshua M. Romero, Robert Pagan-Rosado, Dennis A. Colón
- Rehabilitation of Hand Disorders
- Remy V. Rabinovich, Robert M. Zbeda, Steven Beldner, Daniel B. Polatsch
- Rehabilitation of Wrist Disorders
- Robert M. Zbeda, Remy V. Rabinovich, Steven Beldner, Daniel B. Polatsch
- Rehabilitation of Hip Disorders
- David A. Harwood, Anna H. Green, John P. Stelmach, Alfred J. Tria Jr.
- Rehabilitation of Knee Disorders
- Giles R. Scuderi, Matt H. Nasra, Jeremy Silver, Kara L. Sarrel, Alfred J. Tria Jr.
- Rehabilitation of Foot and Ankle Disorders
- Seyed Behrooz Mostofi, Naveen Joseph Mathai
About this book
This pocket-sized guide provides a practical and comprehensive resource for orthopedic, PM&R, and musculoskeletal specialists, as well as primary care physicians who work in the community outpatient clinic setting. Its consistent chapter format covers each area with anatomy, physical examination, preoperative management, and postoperative rehabilitation sections for the spine and extremities.
The book presents treatment protocols for various injuries, including physical therapy measures such as weight bearing status, PRE, closed or open chain exercises, and timing for returning to routine or sport activities. Its concise presentation of rehabilitation for the upper and lower extremities, the hip and pelvis, and the spine enables quick reference and clinical decision-making.
Furthermore, the book includes a chapter on rehabilitation following the use of orthobiologics, making it a valuable resource for healthcare professionals involved in orthopedic rehabilitation after regenerative intervention.
[ARTICLE] Shoulder Joint Hybrid Assistive Limb Treatment for Chronic Stroke Patients with Upper Limb Dysfunction – Full Text
Posted by Kostas Pantremenos in Paretic Hand on February 12, 2023
Abstract
Upper extremity dysfunction after stroke affects quality of life. Focusing on the shoulder joint, we investigated the safety and effectiveness of rehabilitation using a shoulder joint hybrid assistive limb (HAL). Eight patients with chronic stroke and upper extremity functional disability were enrolled and used a shoulder joint HAL, which assisted shoulder movement based on the user’s intention, through myoelectric activation of the shoulder flexor. Ten training sessions of 30–40 min each were performed to assist voluntary movement of upper limb elevation on the affected side through triggering the deltoid muscle. All patients completed the interventions without shoulder pain. Surface electromyography evaluation indicated post-intervention improvement in coordinated movement of the affected upper extremity. Significant improvements in voluntary and passive shoulder joint range of motion were obtained after the intervention, suggesting improvement in shoulder muscle strength. A significant decrease in the modified Ashworth scale and improvements in functional scores in the upper limb were also observed. Along with safe use for our study patients, the shoulder HAL provided appropriate motor learning benefits. Improvements in shoulder joint function and whole upper limb function were observed, suggesting that HAL could be an optimal treatment method.
1. Introduction
Upper extremity dysfunction due to stroke significantly affects activities of daily living, influencing quality of life [1]. It has been reported that approximately 50% of patients with stroke continue to experience upper limb dysfunction six months after stroke onset, and approximately 60% of those with severe or complete paralysis are unable to perform any movement with their affected limbs [2,3,4]. Recent advances in imaging examinations, such as functional magnetic resonance imaging and near-infrared spectroscopy, have shown that brain plasticity or reorganization can be expected after stroke. Recently, robotic rehabilitation has emerged as a training method to improve patients’ limb dysfunction post-stroke [5,6]. The hybrid assistive limb (HAL) is an exoskeletal robot that controls and assists movements based on bioelectrical activity generated through voluntary movements. By means of generating feedback to the central nervous system, it has been hypothesized that this device stimulates functional recovery through inducing plasticity in the impaired central nervous system [7]. There are four types of HAL, namely, lower limb, single joint (for elbow and knee joints), and lumbar types. One study that used a single joint HAL for the elbows reported improvements in upper limb motor function in patients with stroke [8]. Focusing on shoulder dysfunction after stroke, we previously conducted training using a shoulder joint HAL developed by our research group in patients with stroke. Furthermore, we published a case report showing that this training could be performed safely, while improving shoulder joint function and coordinated movements of the upper limb on the affected side [9]. Rehabilitation therapy focusing on the shoulder joint is extremely important, as improving shoulder joint function not only improves activities of daily living, such as changing clothes, but also ameliorates distal control of the upper extremity and prevents shoulder pain [10,11,12]. In this study, we aimed to determine the utility of shoulder joint HAL training applied in eight patients with chronic stroke and moderate-to-severe upper limb dysfunction.
2. Materials and Methods
2.1. Patients
Eight patients (six males, two females) were enrolled in this study. Patients’ clinical data are shown in Table 1. The mean patient age (± standard deviation) was 68.4 ± 8.38 (range, 53–84) years. The mean time from stroke onset was 5.86 ± 6.40 (range, 0.93–19.7) years. All patients showed moderate-to-severe hemiplegia with a shoulder flexion manual muscle test (MMT) score of ≤2. Their grip power was <50% on the affected side compared with the unaffected upper limb and three patients were unable to complete grip dynamometer measurements. In Patient 8, bilateral grip power measurements could not be measured as the unaffected upper limb had been amputated at the hand level due to trauma in childhood. This study was conducted in accordance with the Declaration of Helsinki, with approval from the Ethics Committee of the Tsukuba University Faculty of Medicine (approval no.: TCRB18-38). All patients provided written informed consent for participation and publication, including the use of any accompanying images.
Table 1. Patient characteristics.

2.2. HAL Intervention
We set up the single-joint HAL in accordance with previous studies [5,6]. In brief, the proximal section of the HAL was fixed to a tripod using an attachment, and the distal section was fitted to the patient’s upper arm with a belt for the elbow joint, which was attached to the HAL (Figure 1a). The elbow was extended to its full range of motion (ROM); the forearm was placed in a slightly externally rotated position to prevent external rotation of the humerus and was immobilized near the wrist joint using a splint and bandage (Figure 1b). Flexion electrodes were placed on the skin of the anterior deltoid fibers and triggered for upper limb elevation. Instead of using the electrodes as triggers, relaxation of the shoulder flexor muscle and gravity functioned to trigger extension. The ground was placed on the bone touching the site where the bone was palpable, without interfering with the surface electromyography device.
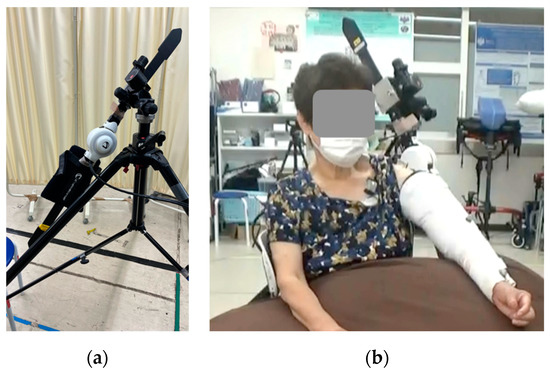
Figure 1. Images of the shoulder joint HAL device. (a) Single-joint HAL fixed to a tripod with attachments, (b) shoulder joint HAL fixed with splints and an elastic bandage. HAL, hybrid assistive limb.
The upper limb raising angle during training was measured prior to fitting the HAL, and the shoulder joint ROM was initiated at approximately 20° less than the ROM at the shoulder joint and then gradually increased while observing the training condition. Two methods were used to adjust the actual angle: (i) adjustment of the HAL, and (ii) adjustment using a tripod attachment. The HAL angle could be adjusted from 0° to 120°, and was used for adjustment. When the HAL assist angle of 120° was considered to be insufficient, a further increase in the angle of elevation was obtained through changing the tilt of the HAL itself using a tripod attachment.
All eight patients who participated in the study underwent a total of 10 HAL training sessions, with each session lasting 30–40 min, with at least one week between each intervention. The actual training time for upper extremity raising was approximately 20–30 min, including breaks, after approximately 5–20 min for electrode preparation and HAL placement and removal.
During training, a therapist stabilized the medial side of the patients’ forearms to avoid excessive internal rotation or flexion of the upper limbs during the raising of the upper limbs. The direction of upper limb elevation was evaluated while observing the raising of the scapular plane, which needs to be considered to prevent excessive interference between the humerus and scapula (Figure 2). The pace of each exercise was set so that patients could fully extend their arms one at a time to avoid vigorous raising and then repeat raising the upper arm. […]
[Abstract] AGREE: A compliant-controlled upper-limb exoskeleton for physical rehabilitation of neurological patients
Posted by Kostas Pantremenos in Paretic Hand, Rehabilitation robotics on February 1, 2023
Abstract
In this work, we introduce the Agree exoskeleton, a robotic device designed to assist in upper-limb physical rehabilitation for post-stroke survivors. We detail the exoskeleton design at the mechatronic, actuation, and control levels. The Agree exoskeleton features a lightweight and adaptable mechanical design, which can be used with both the right and left arm, supporting three active degrees-of-freedom at the shoulder and one at the elbow. The device embodies a spring-pulley anti-gravity system to minimize torque requirements and has torque sensors on each joint for safe and smooth interaction with the user. The Agree control system, which employs a loadcell-based impedance control method, offers various modes of human-robot interaction, such as passive-assisted, active-assisted, and active-resistive exercises. Results from our experimental characterization demonstrate that the exoskeleton is capable of both compliant and rigid behavior, providing a wide range of haptic impedance and transparent behavior to both user-generated and therapist-generated forces. Our findings indicate that the Agree exoskeleton may be a viable option for safely assisting patients with neurological conditions.
[Abstract] CURER: A Lightweight Cable-Driven Compliant Upper Limb Rehabilitation Exoskeleton Robot
Posted by Kostas Pantremenos in Paretic Hand, Rehabilitation robotics on December 21, 2022
Abstract
Upper limb exoskeletons show promise for improving functionalities required for stroke patients. Despite recent progress, most of current upper limb rehabilitation devices are still bulky, heavy, and less compliant to be applied. This article presents a cable-driven compliant upper limb rehabilitation exoskeleton robot (CURER) with a lightweight frame and comfortable human–robot interaction. A modular series elastic actuator (SEA) was designed to provide controlled torque for each active robotic joint, and Bowden cables were applied to transfer controlled torque to distal joints. A six-bar double parallelogram mechanism was designed to implement 3 active degrees of freedom (DOFs) of a shoulder. An actuated elbow with 1 DOF and a wrist with a passive DOF were also developed for CURER. The anthropomorphic shoulder, elbow, and wrist joints can minimize misalignment between human upper limbs and the robot. The length of anthropomorphic arm was adjustable for a wide range of users. It can apply up to a 33 N·m torque in shoulder flexion/extension, abduction/adduction, intra/extra rotation, and elbow flexion/extension, with a range of 7.6–8.0 Hz position bandwidth in each actuation. CURER has a large range of motion and can provide accurate torque control for stroke patients’ requirements. Besides, a comprehensive rehabilitation strategy including robot-in-charge mode and human-in-charge mode was developed for different recovery stages. Experiments carried out on CURER actuation units demonstrated good position and impedance control performance. Finally, a virtual reality training system was developed to assist the subjects to accomplish upper limb rehabilitation efficiently.
[Abstract] Design of an Exoskeletal Prototype to Contribute to the Partial Rehabilitation of the Upper-Limb
Posted by Kostas Pantremenos in Paretic Hand, Rehabilitation robotics on December 11, 2022
Abstract:
Rehabilitation processes are very important to recover the movements of the limbs of the human body, but in many countries where technology is very scarce, rehabilitation procedures are performed traditionally; that is why the objective of this research is to design an exoskeleton prototype that contributes to the rehabilitation of patients with partial mobility of the upper limbs. For the development of the prototype, the VDI 2206 methodology is applied, where the research is divided into mechanical systems and electronic systems. For the design of the mechanical structure, it is considered that the links are adjustable to achieve a greater scope of use, whose parameters are for patients whose height is in the range of 155 cm to 175cm; the development of the robotic structure is designed in SolidWorks software. For the electronic design, EMG sensors and triaxial accelerometers are considered to detect the movements that the patient wants to perform. Also, a circuit with an LCD screen is made so that the specialist can program the routines according to the patient’s requirements. The results obtained after being subjected to a stress analysis simulation are that the structure can support a maximum weight of 76 kg, which is equivalent to a person whose height is 175cm, and the suitable material is 6061 aluminum alloy; the results of the electronic design show the good interaction of the sensors with the controller as it performs the movements of the actuators properly.
[Abstract] CLEVERarm: A Lightweight and Compact Exoskeleton for Upper-limb Rehabilitation
Posted by Kostas Pantremenos in Paretic Hand, Rehabilitation robotics on January 4, 2022
Abstract
This paper presents the electromechanical design, system architecture, baseline control development, and the preliminary evaluation of a novel upper-limb exoskeleton, named CLEVERarm. The developed system can support the motions of inner shoulder, glenohumeral joint, elbow and wrist’s pronation/supination and flexion/extension. Enhanced portability, design robustness, and ergonomic performance are chosen as the pillars of the design. These qualities are selected due to their importance for enabling exoskeletons’ use outside the clinical and research setting. CLEVERarm’s links are manufactured using carbon-fiber-reinforced 3D-printed plastic to achieve a lightweight and compact design. For design robustness, minimizing maintenance requirements and usability risks are taken into account in the selection and placement of actuation, sensing and controller components. Finally to realize an ergonomic interaction, inner shoulder motions are supported by a back-drivable motorized design, controlled by an impedance controller. This architecture enables accommodating natural variations in scapulohumeral rhythm among users. The performance of the developed exoskeleton is evaluated using experiments involving healthy subjects. It is shown that despite its lightweight, CLEVERarm is structurally stiff and supports a large subset of the healthy range of motion. Additionally, experimental results confirming the performance of the baseline controller are presented.
[WEB PAGE] An Orthopedic Approach to the Hemiparetic Upper Limb: Understanding the Biomechanics and Pathoanatomy of the Shoulder.
Posted by Kostas Pantremenos in Paretic Hand on December 23, 2020
By Henry Hoffman
Before I co-founded Saebo, I was a practicing occupational therapist specializing in non-operative orthopedic medicine and manual therapy of the upper quadrant. While working at Burke Rehabilitation Hospital in White Plains, NY, part of my caseload was dedicated to orthopedic rehabilitation including the treatment of overhead athletes. Through the International Academy of Orthopedic Medicine (IAOM), I received my post-professional education training on diagnosis specific musculoskeletal management.
In addition to treating clients with orthopedic injuries, I had the blessed opportunity to periodically work with stroke survivors in the outpatient setting at Burke (which became the beginning of Saebo, but I will save that story for another time). While treating neurologically impaired clients, I found myself applying key orthopedic principles I developed during my training with the Academy. I believed (and still do) having an orthopedic background, coupled with a good understanding of evidenced based treatment for the neurologically impaired population, enhanced my therapeutic outcomes. Whether it was identifying a patient’s source of pain, performing joint specific mobiIization techniques, or providing appropriate strength training drills, my comprehensive ortho/neuro hybrid treatment approach was more successful with clinical outcomes than using traditional “neuro” based strategies alone.
Whether we are treating a young overhead athlete that reports pain and clicking during the cocking phase of throwing or a middle-aged stroke survivor who is unable to touch the back of his head due to a capsular pattern, licensed occupational and physical therapists must be knowledgeable in understanding the biomechanics and pathomechanics of the shoulder complex in order to properly examine and treat these conditions. Regardless of the diagnosis, subacromial pathologies are the same. Yes, the causal factors may be different, but mechanics are mechanics and lesion sites are lesion sites despite the pathogensis.
The purpose of today’s blog is to offer an introductory review of the bio- and pathomechanics of the glenohumeral joint and scapulothoracic articulation. By developing a better understanding of the shoulder, we as clinicians will be more suited to resolve the functional limitations of our clients and offer them an improved quality of life.
Biomechanics of Arm Elevation:
Arm elevation is the most important function of the shoulder. There are 3 types of arm elevation – flexion, abduction, and scaption (plane of the scapula). In order to perform full arm elevation, the glenohumeral, scapulothoracic (articulation), sternoclavicular, acromioclavicular joints along with the cervico-thoracic junction have to participate in a coordinated, concomitant, and smooth pattern.
Scapulohumeral Rhythm
Normal maximum shoulder elevation is 180 degrees. Traditional theorists feel the overall glenohumeral-scapulothoracic rhythm is a 2:1 ratio. Recent literature now suggests that the 2:1 ratio is not consistent across an entire arc of shoulder elevation. The first 30-60 degrees of elevation has been termed the setting phase. The scapula is seeking a position of stability in relation to the humerus during this phase. As the arm elevates, the scapula has the tendency to tip secondary to the weight. To prevent this, the trapezius and serratus anterior contract to stabilize the scapula. In addition, these 2 muscles combine to form a force couple that upwardly rotates the scapula. In this early phase, motion occurs primarily at the GHJ.
Note: Poppen and Walker report a 4:1 glenohumeral to scapulothroacic ratio during the first 25 degrees, thereafter, an almost equal 5:4 ratio occurs. Doody showed a 7:1 ratio during the first 30 degrees, thereafter, a 1:1 ration from 90-150.
In the middle 60 degrees, elevation phase, glenohumeral motion is about equal to scapulothoracic motion. The last 60 degrees, glenohumeral motion is again more than scapulothoracic motion (5:1). The final scapular motion is the result of clavicular rotation and elevation of the acromioclavicular joint.
Scapulothoracic Motion
Movement at the scapulothoracic articulation is important for normal biomechanics of the shoulder joint. Scapulothoracic rhythm is important because it (1) sets the most functional position of the GHJ, (2) prevents active insufficiency of the scapulohumeral muscles, and (3) allows for sufficient ROM between the humeral head and the subacromial space.
Arthokinematics
The glenoid fossa and the humeral head are incongruent surfaces. Rotation of the joint cannot take place as a pure spin, but requires that the motions of the humerus be accompanied by a combined rolling and gliding of the humeral head on the glenoid fossa in a direction opposite of the movement of the shaft of the humerus. The humeral head slides posteriorly and inferiorly in flexion, anteriorly and superiorly in extension, and inferiorly in abduction, and superiorly in adduction. In external rotation, the humeral head slides anteriorly and in internal rotation it slides posteriorly.
Muscles Contributing to Arm Elevation
Deltoid Muscle
The largest and most important glenohumeral muscle. As the humerus elevates, the translatory component of the deltoid as a whole increases joint compression. When the humerus is in the plane of the scapula, the anterior and middle deltoid are optimally aligned to produce elevation of the humerus. In this motion, the posterior deltoid primarily serves as a joint compressor.
Supraspinatus Muscle
The primary function of this muscle is abduction with the secondary motion being external rotation. It exerts maximum effort at approximately 30 degrees of abduction. The secondary functions of the supraspinatus are to compress the GHJ and to provide stability at the humerus during elevation.
Infraspinatus, Teres Minor, Subscapularis Muscles
The function of these muscles are to depress the humeral head and prevent superior impaction of the humeral head into the acromion. In addition, they provide muscular balance and help stabilize the joint capsule.
Latissmus Dorsi, Pectoralis Major, and Teres Major
Latest EMG studies are showing that during arm elevation, the above muscles are acting as humeral head depressors. In addition, the muscles function as stabilizers for the anterior capsule.
Upper and Lower Trapezius and Serratus Anterior Muscles
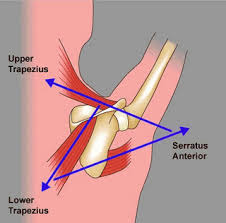
These muscles form a force couple that drives the scapula into upward rotation. In elevation, the force of the trapezius is more critical to the movement of upward rotation than the force of the serratus anterior. However, in order to perform full elevation both of these muscles must be firing.
Pathomechanics of Arm Elevation:
Prior to and following an orthopedic injury to the shoulder, pathologic changes take place. Because of this, normal mechanical behavior of the shoulder is substituted with asynchronous and faulty mechanics. Following a neurological injury (UMN lesion) damage to the sensory and motor areas of the cerebral cortex and brain stem may lead to primary impairments such as weakness, motor control, sensation, and tone. These clients often suffer from paralysis or abnormal tone in the muscles controlling their glenohumeral joint and scapula resulting in poor biomechanics which can lead to microtraumatic lesions. Therefore, an orthopedic or neurologic injury can cause the entire upper quadrant elevation chain to be affected.
When poor mechanics or soft tissue lesions are present, it is the clinician’s job to identify the source so proper treatment strategies can be provided. Below are examples of some of the common shoulder pathologies seen by orthopedic and neurologic clients:
Rotator Cuff Injuries
1. Subacromial Impingement – involves painful compression of one of the soft tissue structures located between the head of the humerus and the acromion, coracoacromial ligament, coracoid process, or AC joint. Impingement may occur due to structural narrowing (primary) or from underlying instability of the glenohumeral joint (secondary). Biomechanical changes after a neurological injury place affected clients at greater risk for impingement.
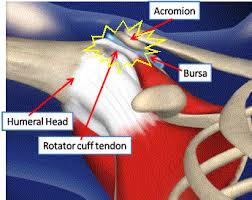
Note: Soft tissue structures that can be impinged:
- Supraspinatus
- Infraspinatus
- Subscapularis
- Teres minor
- Subacromial-subdeltoid bursa
- Joint capsule
- Long Head of Biceps tendon
2. Tensile Failure – repetitive eccentric overload of the rotator cuff muscles.
3. Internal Impingement – impingement of the soft tissues of the rotator cuff and joint capsule on the glenoid or between the glenoid and the humerus (i.e., overhead athlete).
Capsuloligamentous Injuries: result in partial separation of the humerus from the glenoid fossa. The rotator cuff is the primary stabilizing factor during mid range motions. At end range motions, the capsular ligaments become the stabilizing force. It is common for clients that performed repetitive overhead tasks to develop instability due to challenging the integrity of the ligaments. In addition, paralysis of the shoulder girdle due to a neurological injury may comprise the dynamic stability of the cuff muscles leading to an unstable joint.
3 Main Directions of Instability
- Anterior Instability: humeral head migrates excessively in an anterior direction relative to the glenoid.
- Inferior Instability: excessive inferior movement of the humeral head relative to the glenoid.
- Posterior Instability: excessive movement of the humeral head in a posterior direction relative to the glenoid.
The most common type of instability (subluxation) associated with hemiplegia is in an inferior direction. Inferior subluxations occur when muscle weakness leads to a downward rotation of the scapula in relation to the thorax. The labrum and inferior portion of the glenoid fossa can no longer provide sufficient support to secure the humeral head into the glenoid. In addition to the faulty mechanics at the scapula, the proximal migrators of the shoulder (deltoids) are no longer able to support the weight of the arm. Gravitational forces applied to the weakened arm stretches the inert and non-inert structures to the point that the humeral head migrates distally below the glenoid fossa.

Capsular Pattern (Frozen Shoulder):
Capsular pattern is synonymous with frozen shoulder, immobilization arthritis, and adhesive capsulitis. It consists of greater limitation of external rotation than abduction and a greater limitation of abduction than internal rotation, in a ratio of 3:2:1, respectively. Hemiparetic patients with limited movement often develop a capsular pattern (and pain) due to progressive adaptive changes to the collagen. Loss of motion occurs from thickening and contracture of the coracohumeral ligaments and rotator interval which prevents external rotation. As the pathology progresses, abduction and internal rotation are eventually affected as well.
It is not uncommon for neurological clients to report a painful shoulder while in therapy. For moderate to severely impaired clients who are unable to raise their arm mid range or higher, pain may result from spasticity and contractures. For mildly impaired clients that exhibit overhead active motion, pain may be due to compressive forces – primary or secondary impingement. This can come from mild weakness of the scapular or rotator cuff muscles or instability due to a previous subluxation event that resolved itself.
Although the above clinical pathologies are not inclusive, it does reflect some of the more commonly seen concerns in the clinic. Understanding the biomechanics and pathomechanics of the shoulder is paramount for proper musculoskeletal management. Clients suffering from an upper motor neuron lesion, with passive or active movement limitations will have some degree of pathomechanical issues. Therefore, clinicians must understand how the entire kinetic chain operates as a complete unit in order to improve upper limb function.
If you are a clinician who mainly treats neurologically impaired clients, seek out orthopedic based continuing education courses to enhance your clinical assessment and treatment skills. The added value of having a good understanding of the musculoskeletal system can be extremely significant when treating neurological clients suffering from joint pathology.
Henry graduated from D’Youville College in Buffalo, NY in 1997 with a Masters degree in Occupational Therapy. He has worked in a variety of clinical settings including home health, acute, sub-acute, and outpatient rehab. Prior to leaving Burke Rehabilitation Hospital in New York in 2002, he worked as a clinical specialist in orthopedic medicine and manual therapy of the Upper Quadrant. After leaving Burke, Henry co-founded Saebo with the goal of creating innovative and life changing solutions for the physically impaired population. He currently holds over 15 patents with products that have helped over 30,000 clients regain function. Saebo’s name is an acronym for Henry’s grandmother “Sarah Eileen Booth”. Her entire life was dedicated to providing a hand to others in need. Saebo’s mission is to match her spirit, dedication, and desire to help others.
[Abstract] A Home-based Bilateral Rehabilitation System with sEMG-based Real-time Variable Stiffness
Posted by Kostas Pantremenos in Paretic Hand, REHABILITATION, Rehabilitation robotics, Tele/Home Rehabilitation on October 19, 2020
Abstract
Bilateral rehabilitation allows patients with hemiparesis to exploit the cooperative capabilities of both arms to promote the recovery process. Although various approaches have been proposed to facilitate synchronized robot-assisted bilateral movements, few studies have focused on addressing the varying joint stiffness resulting from dynamic motions. This paper presents a novel bilateral rehabilitation system that implements a surface electromyography (sEMG)-based stiffness control to achieve real-time stiffness adjustment based on the user’s dynamic motion. An sEMG-driven musculoskeletal model that incorporates muscle activation and muscular contraction dynamics is developed to provide reference signals for the robot’s real-time stiffness control. Preliminary experiments were conducted to evaluate the system performance in tracking accuracy and comfortability, which showed the proposed rehabilitation system with sEMG-based real-time stiffness variation achieved fast adaption to the patient’s dynamic movement as well as improving the comfort in robot-assisted bilateral training.

