Posts Tagged physical activity
[WEB] Exercise Releases Chemical Signals that Boost Brain Health
Posted by Kostas Pantremenos in Neuroplasticity on December 17, 2023

Physical activity is frequently cited as a means of improving physical and mental health. Researchers at the Beckman Institute for Advanced Science and Technology have shown that exercise may also improve brain health more directly. They studied how the chemical signals released by exercising muscles promote neuronal development in the brain.
Their work appears in the journal Neuroscience.
When muscles contract during exercise, like a bicep working to lift a heavy weight, they release a variety of compounds into the bloodstream. These compounds can travel to different parts of the body, including the brain. The researchers were particularly interested in how exercise could benefit a particular part of the brain called the hippocampus.
“The hippocampus is a crucial area for learning and memory, and therefore cognitive health,” said Ki Yun Lee, a PhD student in mechanical science and engineering at the University of Illinois Urbana-Champaign and the study’s lead author. Understanding how exercise benefits the hippocampus could therefore lead to exercise-based treatments for a variety of conditions including Alzheimer’s disease.
To isolate the chemicals released by contracting muscles and test them on hippocampal neurons, the researchers collected small muscle cell samples from mice and grew them in cell culture dishes in the lab. When the muscle cells matured, they began to contract on their own, releasing their chemical signals into the cell culture.
The research team added the culture, which now contained the chemical signals from the mature muscle cells, to another culture containing hippocampal neurons and other support cells known as astrocytes. Using several measures, including immunofluorescent and calcium imaging to track cell growth and multi-electrode arrays to record neuronal electrical activity, they examined how exposure to these chemical signals affected the hippocampal cells.
The results were striking. Exposure to the chemical signals from contracting muscle cells caused hippocampal neurons to generate larger and more frequent electrical signals — a sign of robust growth and health. Within a few days, the neurons started firing these electrical signals more synchronously, suggesting that the neurons were forming a more mature network together and mimicking the organization of neurons in the brain.
However, the researchers still had questions about how these chemical signals led to growth and development of hippocampal neurons. To uncover more of the pathway linking exercise to better brain health, they next focused on the role of astrocytes in mediating this relationship.
“Astrocytes are the first responders in the brain before the compounds from muscles reach the neurons,” Lee says. Perhaps, then, they played a role in helping neurons respond to these signals.
The researchers found that removing astrocytes from the cell cultures caused the neurons to fire even more electrical signals, suggesting that without the astrocytes, the neurons continued to grow — perhaps to a point where they might become unmanageable.
“Astrocytes play a critical role in mediating the effects of exercise,” Lee says. “By regulating neuronal activity and preventing hyperexcitability of neurons, astrocytes contribute to the balance necessary for optimal brain function.”
Understanding the chemical pathway between muscle contraction and the growth and regulation of hippocampal neurons is just the first step in understanding how exercise helps improve brain health.
“Ultimately, our research may contribute to the development of more effective exercise regimens for cognitive disorders such as Alzheimer’s disease,” Lee says
[WEB] Exercise Just Once a Month Can Boost Later Cognitive Function
Posted by Kostas Pantremenos in Cognitive Rehabilitation on March 9, 2023

A STUDY FOUND EXERCISING AS INFREQUENTLY AS ONCE A MONTH WAS LINKED TO IMPROVED COGNITIVE FUNCTION LATER IN LIFE.
A new study led by UCL researchers has found that exercising at least once a month at any time in adulthood is linked to better cognitive functioning in later life.
The study, published in the Journal of Neurology, Neurosurgery, and Psychiatry, looked at data from 1,417 people who completed surveys about their leisure-time physical activity (sports and exercise) over three decades and took cognitive tests at the age of 69.
The research team found that people who reported being physically active at least one to four times a month in five separate surveys, aged 36, 43, 53, 60-64, and 69, had the most significant cognitive effect.
This effect was more significant than for those who reported frequently exercising (more than five times a month) during at least one survey period but who did not necessarily keep this up across multiple surveys.
“Our study suggests that engaging in any leisure-time physical activity, at any point in adult life, has a positive effect on cognition,” said Sarah-Naomi James, PhD, lead author. “This seems to be the case even at light levels of activity, between once to four times a month. What’s more, people who have never been active before, and then start to be active in their 60s, also appear to have better cognitive function than those who were never active.”
The study participants were from the 1946 British Birth Cohort, the UK’s longest-running population-based cohort who were all born in the same week in 1946 and whose health has been tracked throughout their life.
The researchers aimed to investigate if there was a period of life when physical activity was essential for later-life cognitive function, in the same way that cardiovascular health in middle age appears to be more important for later cognitive health than during other times of life.
But, rather than finding that one period of life was more important than others, they concluded that starting some form of physical activity and maintaining it over a long time may be more important than the timing of this activity.
At age 69, study participants took several cognitive tests, including the Addenbrooke’s Cognitive Examination, which assesses overall cognitive state and is used to screen people for cognitive impairment. They also did a word learning test and a visual processing speed test, where they were asked to cross out all instances of a particular letter in a page of text.
The researchers also looked at other factors that might explain the link between exercise and cognitive functioning.
They found that, while a link remained after accounting for many other factors, including mental health and cardiovascular health, half to two-thirds of the association could be explained by education level, childhood cognition, and socioeconomic background.
People who engaged more in physical activity were also more likely to have taken A-levels and gone to university, had parents from a more privileged background, and done better in tests at the age of eight, and these factors may separately contribute to better cognitive function in later life.
However, a separate link remained between exercise and cognitive function, and the researchers said more work was needed to understand this link better.
The research was supported by Alzheimer’s Research UK (ARUK) and the Medical Research Council and involved researchers from the MRC Unit for Lifelong Health & Ageing at UCL and the UCL Queen Square Institute of Neurology.
[Review] Mobile health applications for improving physical function, physical activity, and quality of life in stroke survivors: a systematic review – Full Text
Posted by Kostas Pantremenos in Apps on November 10, 2022
Abstract
Purpose
To evaluate the effectiveness of mobile health applications (mHealth apps) containing a physical training component on physical function and physical activity in stroke rehabilitation.
Materials and methods
A systematic literature search was conducted in three databases for studies published from inception to 12 July 2022. Clinical trials including mHealth apps with a physical training component were included using outcomes of physical function and physical activity. Quality of life was extracted as a secondary outcome.
Results
Five RCTs, two non-RCTs, and four uncontrolled clinical trials were included with a total of 264 stroke survivors. Eleven apps were identified with a physical training component using features of gamification (six apps), exercise prescription (three apps), and physical activity (two apps). Six out of seven studies reported statistically significant improvements in physical function in favor of the experimental group, with the most robust findings for upper extremity function. For physical activity, statistically significant improvements were seen in the experimental groups. Only one study showed significant improvement in quality of life. Overall study quality was fair.
Conclusions
mHealth apps containing a physical training component are promising for physical function and physical activity in stroke rehabilitation. Further research is warranted to confirm these conclusions.
- Implications for rehabilitation
- Design content of mobile apps with a physical training component were focused on gamification, exercise prescription, and physical activity
- Using mobile app-delivered therapy seem promising for improving upper extremity function in stroke rehabilitation
- Using mobile apps also supported an increase of physical activity in people with stroke
- Studies using mobile apps should report more specifically the dosage of physical training and adherence
- Using mobile apps seems promising as an additional tool for clinical work, however, more studies are required to understand their effectiveness in stroke rehabilitation.
Introduction
Stroke is one of the leading causes of death and long-term disability worldwide, accounting for approximately 12% of total deaths [1]. The absolute number of stroke deaths has increased by 43% in the last 30 years and stroke was the third most common cause of disability worldwide in 2019 [1]. At stroke onset, stroke survivors suffer from very heterogeneous symptoms and signs. Symptoms of stroke vary individually with a wide range of motoric, mental, lingual, sensory, and cognitive impairments that cause functional challenges in daily life and decrease the quality of life (QoL) [2–5]. The most common impairments are paresis experienced in upper (69%) and lower (61%) extremities in the acute stage of stroke [6]. At three years post-stroke, 26% of stroke survivors are still moderately or severely disabled and more than half of the stroke survivors are inactive [7]. Moreover, people with stroke throughout all stages have lower physical activity (PA) levels compared to healthy age-matched individuals [8]. Furthermore, physical inactivity is associated with lower chances of independence in activities of daily living [9]. Also, stroke survivors have reported a decline in QoL [3,10].
To reduce disability after stroke, physiotherapy plays an important role in rehabilitation and the amount of time spent in therapy is highly correlated with functional recovery after stroke [11,12]. In the recent decade, more attention has been given to telerehabilitation, mobile health applications (mHealth apps), or other technological therapy modalities in stroke rehabilitation [13–16]. Due to the rapid increase of smartphone and tablet apps in common daily life, interest in using a mHealth app has also increased in healthcare and rehabilitation services [17]. mHealth app is defined as a health and well-being mobile service delivered using a mobile app or other wireless technology in medical care, which enables two-way health-related information delivery and communication [18]. Interest has grown mainly with the assumption that mHealth apps support specific rehabilitation goals, promote self-management, and increase adherence to home-rehabilitation exercises [19]. Moreover, one systematic review concluded that mHealth apps have the potential to facilitate adherence to chronic disease management in diabetes mellitus, cardiovascular diseases, and chronic lung diseases, but the current evidence of the association between mHealth apps and adherence to disease management is still rather mixed [20]. For instance, only 58% of the studies reported usability, feasibility, or acceptability of mHealth apps in the previous review [20]. Moreover, the usefulness of mHealth apps in stroke rehabilitation is still unclear. Another review provided an overview of the number of commercially available mHealth apps in stroke rehabilitation to offer a low-cost strategy and utility in the rehabilitation of stroke survivors in everyday life [21]. However, the mHealth apps were not reviewed for its scientific evidence on particular outcomes of interest in stroke rehabilitation, such as physical function (PF), PA, and QoL.
Another topic related to the growth of mHealth apps is the various content that the apps can provide for stroke rehabilitation. A previous scoping review listed 39 mHealth apps with a vast heterogeneity in the content of apps, of which the most common focuses were upper extremity function (32%), medical management and secondary prevention (26%), exercises, PA, or mobility (24%) [16]. Other previous scoping or systematic reviews have also indicated similar directions where mHealth apps have been implemented in stroke rehabilitation, namely physical, cognitive, and language rehabilitation [22,23]. These previous reviews show that mHealth apps are becoming an interest of study in stroke rehabilitation and their findings show its potential where such apps have been targeted in stroke rehabilitation [24]. However, previous reviews have not yet focused on particular outcomes such as PF, PA, or QoL. Nor there has not been an overview of mHealth apps that can be targeted to physical training at home settings [23].
The aim of this systematic review is to evaluate the effectiveness of mHealth apps containing a physical training component on PF, PA, and QoL in stroke rehabilitation. Moreover, this review includes apps that have the potential to be applied independently of the therapist.[…]
[REVIEW] Do digital interventions increase adherence to home exercise rehabilitation? A systematic review of randomised controlled trials – Full Text
Posted by Kostas Pantremenos in COVID-19, REHABILITATION, Tele/Home Rehabilitation on November 7, 2022
Abstract
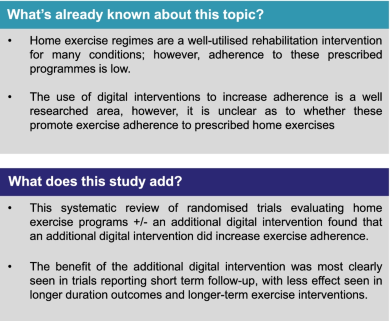
Background
Home exercise regimes are a well-utilised rehabilitation intervention for many conditions; however, adherence to prescribed programmes remains low. Digital interventions are recommended as an adjunct to face-to-face interventions by the National Health Service in the UK and may offer increased exercise adherence, however the evidence for this is conflicting.
Method
A systematic review was undertaken using MEDLINE and CINAHL databases using the PRISMA guidelines. Randomised controlled trials in any clinical population evaluating the adherence to prescribed home exercise interventions with and without additional digital interventions were included. Publication quality was assessed using the Cochrane Risk of Bias tool.
Results
The search strategy returned a total of 1336 articles, of which 10 randomised controlled trials containing data for 1117 participants were eligible for inclusion. 565 participants were randomised to receive the interventions, and 552 to the control. Seven of the ten trials reported a significant difference in adherence between the control and intervention groups favouring an additional digital intervention. Three trials reported equivalent findings. These three reported longer-term outcomes, suggesting an interaction between adherence and duration of intervention. There was substantial heterogeneity in outcome assessment metrics used across the trials prohibiting formal meta-analysis. This included studies were of low to moderate quality in terms of risk of bias.
Conclusion
The addition of a digital interventions to prescribed home exercise programmes can likely increase exercise adherence in the short term, with longer term effects less certain.
Introduction
The emerging use of digital technology in physiotherapy service delivery has been discussed for years; however, the recent Covid-19 pandemic caused major disruption to face-to-face clinical interactions with most outpatient appointments ceased abruptly in March 2020. There is a new focus on health services operating under a more blended approach, incorporating both face-to-face and digitally augmented appointments and treatments [1].
There is already a well-established use of digital technology to augment clinical management in conditions such as diabetes, chronic obstructive pulmonary disease (COPD), chronic heart failure and cardiovascular disease [2, 3]. Patient centred exercise prescription is a well-recognised therapeutic intervention [4], and home exercise programs are frequently provided to patients as part of clinical rehabilitation or to help self-manage long-term conditions [5]. Completing the recommended exercise prescription and adhering to these exercises brings about long-term benefits, which may include better physical function, reduced pain and being able to reach agreed goals [6]. Long-term adherence can also have a considerable benefit in patients’ quality of life and can have a positive benefit on the economy as it can reduce the burden on healthcare systems, as patients are able to self-manage more effectively [7]. A well-established problem when delivering rehabilitation interventions however is the low adherence rate to home exercise programs [8].
Adherence can be defined as ‘the degree a behaviour corresponds with an agreed-on recommendation’ [9]. It has been reported by Argent et al. [10] that adherence to home exercise programs supplied by physiotherapists could be as low as 50%. Low levels of adherence, specifically mid- to long-term, can limit the effectiveness of rehabilitation and may lead to reoccurrence of injuries or not being able to self-manage long-term conditions, resulting in pain, reduced function and subsequently negative outcomes [11].
Adherence, as a concept, is not well understood by researchers [12]. There are many reasons why a patient may struggle to adhere to exercise programmes, which may include perceived barriers such as not having enough time, work schedules, reduction in self-efficacy, the belief that the treatment is ineffective or seeing early positive results so they then feel they do not need to continue with the treatment [10].
There are many forms of digital technology; from mobile applications to websites to simple phone calls. These technologies can help patients self-manage long term conditions or rehabilitate after an injury by providing education, advice, information, feedback and communication from rehabilitation practitioners, which can in turn enhance a patient’s motivation [13].
The use of digital interventions to improve physical outcomes is well researched area, however, surprisingly, there is little consensus as to whether digital interventions promote exercise adherence in patients undergoing physiotherapy [13]. The aim of this review was therefore to evaluate whether the addition of digital interventions to physiotherapist prescribed home exercise programs for any specified clinical condition improved adherence to these programs.[…]
[Abstract] Effects of a combined group physical activity program in people with chronic stroke: A randomized, cross-over trial in a low-income setting
Posted by Kostas Pantremenos in REHABILITATION on September 24, 2022
Abstract
Background: The prevalence of physical inactivity after stroke is high and exercise training improves many outcomes. However, access to community training protocols is limited, especially low-income settings.
Objective: To investigate the feasibility and efficacy of a new intervention: Circuit walking, balance, cycling and strength training (CBCS) on activity of daily living (ADL) limitations, motor performance, and social participation restrictions in people after stroke.
Methods: Forty-six community-dwelling individuals with chronic stroke who were no longer in conventional rehabilitation were randomized into an immediate CBCS group (IG; initially received CBCS training for 12 weeks in phase 1), and a delayed CBCS group (DG) that first participated in sociocultural activities for 12 weeks. In phase 2, participants crossed over so that the DG underwent CBCS and the IG performed sociocultural activities. The primary outcome was ADL limitations measured with the ACTIVLIM-Stroke scale. Secondary outcomes included motor performance (balance: Berg Balance Scale [BBS], global impairment: Stroke Impairment Assessment Set [SIAS] and mobility: 6-minute and 10-metre walk tests [6MWT and 10mWT] and psychosocial health [depression and participation]). Additional outcomes included feasibility (retention, adherence) and safety.
Results: ADL capacity significantly improved pre to post CBCS training (ACTIVLIM-stroke, +3,4 logits, p < 0.001; ES 0.87), balance (BBS, +21 points, p < 0.001; ES 0.9), impairments (SIAS, +11 points, p < 0.001; effect size [ES] 0.9), and mobility (+145 m for 6MWT and +0.37 m/s for 10mWT; p < 0.001; ES 0.7 and 0.5 respectively). Similar improvements in psychosocial health occurred in both groups. Adherence and retention rates were 95% and 100%, respectively.
Conclusion: CBCS was feasible, safe and improved functional independence and motor abilities in individuals in the chronic stage of stroke. Participation in CBCS improved depression and social participation similarly to participation in sociocultural activities. The benefits persisted for at least 3 months after intervention completion.
[ARTICLE] Exercise interventions for post-stroke depression – Full Text
Posted by Kostas Pantremenos in Depression on September 9, 2022
A protocol for systematic review and meta-analysis
Abstract
Background:
Post-stroke depression (PSD) is one of the most common neuropsychiatric complications after stroke and is associated with increased risk of death and poor functional outcomes. Strong evidence shows that exercise has benefits for depression. However, it is not clear whether exercise has benefits specifically for PSD. This study aims to explore the effects of exercise on PSD and to establish safe and effective exercise prescriptions.
Methods and analysis:
The PubMed, Cochrane Library and EMBASE, databases will be searched using prespecified search strategies. Randomized controlled trials and non-randomized prospective controlled cohort studies regarding exercise for PSD will be included. The primary outcomes are depression scale and stroke outcome. The secondary outcomes are the occurrence of adverse events, cognitive function, quality of life indices, and the expression of nerve cell factors. The methodological quality of each study will be evaluated by the physiotherapy evidence database scale. The heterogeneity will be evaluated using the I2 test. If I2 > 50%, random effects models will be used in the analysis; otherwise, fixed effects models will be used to pool the data.
Results:
This study will assess the efficacy and safety of exercise for PSD.
Conclusions:
Our findings will be helpful for clinicians to re-examine the clinical decision-making in the treatment of PSD, by assessing the efficacy of a promising treatment modality for patients with PSD.
1 Introduction
Stroke is the second leading cause of death and disability after ischemic heart disease and the third-leading cause of disability-adjusted life-years.[1] In the United States, approximately 795,000 people have a stroke every year. On average, there is a stroke every 40 seconds and a stroke-related death every four minutes.[2] The cost of informal care for stroke patients accounts for more than half of the total cost of informal care for cardiovascular disease.[3] Stroke places a huge burden on affected individuals and health systems, and can lead to functional limitations and psychological disorders. Much attention is paid to motor disorders and physical disabilities following stroke, but the associated psychological disorders are often ignored. However, stroke has been associated with several psychological disorders, including anxiety, apathy, depression, cognitive impairment, mania, and mental illness.[4–6] Post-stroke depression (PSD) is one of the most common neuropsychiatric complications after stroke. Approximately 31% of stroke patients develop depression at some point within five years after the stroke.[7–9] The clinical manifestations are physical dysfunction, depression, slow thinking, and a series of autonomic nervous dysfunctions. Serious PSD reduces the patient’s confidence in therapy and recovery, thus affecting the functional rehabilitation process, deteriorating the patient condition, and increasing mortality.[10]
Drug and psychological therapy have been traditionally used to treat PSD. In several published reviews, drug therapy and psychological therapy were shown to be effective for depression in the elderly and in people with associated physical illness.[11–13] However, because PSD may differ in important ways, it is not appropriate to extrapolate such data to PSD. The use of antidepressants can counteract the negative effects of depression on functional recovery after stroke.[14] However, it will also lead to bleeding, cardiovascular side effects, metabolic enzyme inhibition, effects on the central nervous system, and other adverse events.[15,16] Psychotherapy is commonly applied to treat the psychological problems of patients with PSD, and the available evidence suggests that pharmacological interventions and psychological therapy may prevent depression and improve mood after stroke. However, these conclusions are characterized by very low levels of evidence.[17]
Some studies have shown that exercise may be a complementary treatment for depression.[18–21] Exercise may affect depressive symptoms through various mechanisms. For example, the hypothalamus-pituitary-adrenal axis and immune function may be maladjusted in depression, resulting in elevated cortisol levels. Exercise can improve the regulation of the hypothalamus-pituitary-adrenal response and increase immunity.[22–24] A meta-analysis of adults with depression (not including PSD) showed that exercise plays a positive role in people with non-stroke depression.[25] However, a previous meta-analysis of stroke patients with depression indicated that only higher intensity exercise had a significant effect on depressive symptoms, while lower intensity exercise protocols did not.[26] The use of antidepressant medications was not documented in most studies, so that its potential confounding interaction with exercise could not be assessed. After that systematic review, several well-designed trials have been conducted to investigate the association between exercise and risk of PSD, with conflicting conclusions. Moreover, there is a lack of consensus on the timing, type, intensity, and duration of exercise in patients with PSD. Therefore, it is necessary to conduct a new systematic review and meta-analysis to evaluate whether exercise is effective for PSD.[…]
[Abstract] Gains in Daily Stepping Activity in People with Chronic Stroke after High-Intensity Gait Training in Variable Contexts
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop on July 17, 2022
Abstract
Objective. Many physical therapist interventions provided to individuals with chronic stroke can lead to gains in gait speed or endurance (eg, 6-Minute Walk Test [6MWT]), although changes in objective measures of participation are not often observed. The goal of this study was to determine the influence of different walking interventions on daily stepping (steps per day) and the contributions of demographic, training, and clinical measures to these changes.
Methods. In this secondary analysis of a randomized clinical trial, steps per day at baseline and changes in steps per day following 1 of 3 locomotor interventions were evaluated in individuals who were ambulatory and > 6 months after stroke. Data were collected on 58 individuals who received ≤30 sessions of high-intensity training (HIT) in variable contexts (eg, tasks and environments; n = 19), HIT focused on forward walking (n = 19), or low-intensity variable training (n = 20). Primary outcomes were steps per day at baseline, after training, and at a 3-month follow-up, and secondary outcomes were gait speed, 6MWT, balance, and balance confidence. Correlation and regression analyses identified demographic and clinical variables associated with steps per day.
Results. Gains in steps per day were observed across all groups combined, with no between-group differences; post hoc within-group analyses revealed significant gains only following HIT in variable contexts. Both HIT groups showed gains in endurance (6MWT), with increases in balance confidence only following HIT in variable contexts. Changes in steps per day were associated primarily with gains in 6MWT, with additional associations with baseline 6MWT, lower-extremity Fugl-Meyer scores, and changes in balance confidence.
Conclusion. HIT in variable contexts elicited gains in daily stepping, with changes primarily associated with gains in gait endurance.
[Abstract] IMproving Physical ACtivity after stroke via Treadmill training (IMPACT) and self-management: A randomized trial
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop on July 15, 2022
Abstract
Aim:
To determine if treadmill training embedded in self-management education commencing during stroke inpatient rehabilitation results in more physical activity than usual gait training.
Method:
A prospective, parallel-group, randomized trial with concealed allocation, blinded measurement, and intention-to-treat analysis involving 119 stroke survivors undergoing rehabilitation who were able to walk independently was undertaken. The experimental group undertook treadmill training (40–60% heart rate reserve) and self-management education for 30 min, three times a week for 8 weeks, and the control group undertook the same amount of usual gait training. Outcomes were measured at baseline (Week 0), on completion of the intervention (Week 8), and beyond the intervention (Week 26). The primary outcome was physical activity measured as steps/day using an activity monitor. Secondary outcomes were walking ability, cardiorespiratory fitness, cardiovascular risk, depression, self-efficacy, perception of physical activity, participation, and quality of life.
Results:
After 8 weeks, the experimental group took 1436 more steps/day (95% confidence interval (CI) = 229 to 2643) than the control group. By 6 months, they took 871 more steps/day (95% CI −385 to 2129) than the control group. There was no difference between groups in any other outcome.
Conclusion:
In individuals undergoing rehabilitation after stroke, 8 weeks of treadmill training embedded in self-management resulted in more physical activity than usual gait training and this was largely maintained at 6 months, despite little effect on walking or cardiorespiratory fitness, suggesting the self-management was responsible.
[WEB] Getting Motivated to Move
Posted by Kostas Pantremenos in Caregivers, Uncategorized on March 8, 2022
GETTING MOTIVATED TO MOVE
Posted by Deborah Overman

PHOTO CAPTION: A combination of enjoyable exercises and positive feedback can help motivate clients to increase their activity and improve performance.
NOW MORE THAN EVER, IT’S IMPORTANT FOR CLIENTS TO COUNTERACT THE EFFECTS OF A SEDENTARY LIFESTYLE BY INCREASING MOVEMENT.
By Rosemary Peng, PT, MSPT
Three years ago, I wrote an article about the increasing sedentary lifestyle around the globe and its effects on public health. I never would have predicted that a global pandemic would occur in my lifetime, let alone that it would last for 2 years. Yet here we are, entering the third year of the COVID-19 pandemic with continuing effects on public health as seen through social, emotional, and physical lenses. It seems like a good time to revisit this topic with added importance because of the 2-year health and safety restrictions imposed to prevent deaths from COVID-19-related illness.
Throughout history, humans have been inventing machines and devices to improve work capacity and efficiency. In the last 50 years, computers and their applications have fundamentally changed our school, work, and recreational lives.
CONSEQUENCES OF CONVENIENCE
One consequence of this increased convenience is the reduction in the need for humans to move their bodies for work, school, or fun. This is illustrated by a statistic published in 1969 that reported 40% of school-age children walked or rode their bikes to school. By 2001, that number dropped to 13% as more children were driven to school.1 Sedentary patterns aren’t just limited to the United States. Other countries are seeing similar trends of declining physical activity. In Japan, for example, a study of more than 2,000 adults older than age 40 years showed that 50% of waking time was sedentary.2
Contributing to the increased amount of sedentary behavior is not only the use of cars to move from place to place, but also the use of technology and services for work, daily chores, and activities. The percentage of high-activity jobs showed a decrease and low-activity jobs showed an increase in the years between 1970 and 2000.1 In recent years, the availability of technology and services has reduced the time spent doing daily chores that once required physical activity. Robots now vacuum and cut the lawn. Clicking a computer can send groceries to the store curb or a shopper’s front door. A touch of the button not only changes the channel of the TV, but opens the garage door, turns on the oven, and opens the blinds. Voice-activated devices are another way to perform activities that once required walking, standing, bending, and reaching.
Medical professionals see the effect of this decrease in physical activity in public health and well-being. A recent systematic review and meta-analysis looked at the effect of sedentary lifestyle on disease, hospitalization, and mortality in adults.3 It found that prolonged sedentary time was associated with deleterious health effects. As can be seen from research, despite humans’ cleverness in developing tools to reduce their need to move, the body needs to move for its own good.
ENTER THE COVID-19 PANDEMIC
Winter of 2020 changed our lives as the aggressive COVID-19 virus spread rapidly and immediately brought severe illness and death to communities around the globe. Protective health measures of public lockdowns, social distancing, and changes in work life were put in place immediately to protect life and prevent the spread of the disease caused by the virus. The result was even more sedentary behaviors including for those who were otherwise physically active. Schools became remote, so children were no longer getting exercise from walking to or within the school, physical education class, or after-school activities. Those who now worked from home had only to walk from one room to another in their home instead of walking even from the parking lot to the office. Community gyms and other physical recreational facilities were closed, and many who regularly participated no longer had access to exercise equipment. Although those strict measures to reduce death and disability have recently been modified and reduced, there are still ongoing measures that continue to reduce the physical activity of people around the world.
Many research articles and papers have since been written about the effect of the pandemic emergency measures on community health, including physical and mental health. One review paper published as early as September 2020 discussed the decline of physical activity caused by the confined lifestyle after the pandemic was declared, concluding that “practicing physical activities has a key role in the levels of physical fitness and is essential to balance and improve health and quality of life during the COVID-19 pandemic.”4 Another systematic review published in December 2020 found several health benefits from physical activity during the pandemic including reduction in stress level, improved sleep, decreased depression, and decreased anxiety in those who exercised regularly.5 Indeed, there are many research articles since these that describe the negative effects of the COVID-19 pandemic on the health of all age groups and the importance of improving physical activity today.
FOUR PRINCIPLES
Therapists see the effects of sedentary life in the form of pain, joint or muscle injury, obesity, high blood pressure, diabetes, stroke, and osteoporosis. Therapists are in a position to educate and address the dysfunctions and adverse health effects that this sedentary lifestyle has created. Four principles can help therapists develop an exercise or activity prescription for patients of any age and medical condition.
1) Identify the patient’s prior fitness level. This requires not just questioning once but having ongoing discussion about what the patient’s typical day is like and how much movement they get at school, work, home, and in the community. How much exercise does the patient get in a typical week? One question that would be helpful is “How often do you sit during the day?” or “How much of the day do you sit?” Use objective measurements to determine the patient’s level of strength and fitness, such as the 6-Minute Walk Test, 30-Second Chair Stand, Five Times Sit to Stand, or 2-Minute Step Test.
2) Educate patients about the consequences of inactivity or being sedentary. Use stories and analogies to help create a picture for the patient of movement versus being sedentary. Discuss ways that they can increase movement in their day, even helping them to make smart choices of when to use versus when not to use available technology or services.
3) Progress exercise in a thoughtful, patient-specific manner. Patients that have a history of being more active can be progressed more quickly to higher levels of intensity and duration than patients that have a long history of being sedentary. One rep max test should be used when possible to determine appropriate resistance levels for strength training, and HR or RPE should be used to determine whether aerobic exercise is reaching the level needed for change.
4) Motivate and encourage patients to achieve a high level of exercise performance. A recent study of experts looked at features of physical activity apps that would improve participation in individual, recreational sports.6 Several features found that were important for effectiveness of app design to encourage use include fun or enjoyment, feedback and feedforward information, rewards, and social components. These features can be applied to physical therapy for improving patients’ effort and performance.
FITNESS CAN BE FUN
What is fun for one person is not necessarily fun for everyone. For example, one older patient who wants to stand for longer periods of time but who feels fatigue quickly may stand for longer periods of time while drawing a picture in an artist’s pad, while another may be more motivated by a Wii bowling game. A younger person who may be inactive and deconditioned may find fun in using a device that imitates sports, such as the Pro Fitter 3D Cross Trainer from Fitterfirst, Calgary, Alberta, Canada. This device allows the user to integrate the rhythmic weight transfer of skiing, as well as motions that build strength and balance among the 20 functional exercises it provides. For patients who may enjoy walking but want to begin a program in the clinic, an elliptical device that provides a natural walking motion such as the SXT7000 from Scifit, Tulsa, Okla, may be appropriate.
Crafts, music and dancing, board games, interactive video games, and virtual reality are some ways to make therapy enjoyable and transferable to home. New virtual reality screens are available on exercise bikes, treadmills, steppers, ellipticals, and balance machines that enhance the user’s level of enjoyment.
“Gamification” of therapy can include the use of interactive video games, which can be off-the-shelf options, such as Wii and Kinect, or new video games being developed for therapy use. Therapists are still involved in the treatment, watching and correcting form, or setting up the environment to promote the movement wanted.
Feedback can take many forms. Verbal feedback can always be given by the PT. But one benefit of technology is that exercise equipment now often comes with screens that provide feedback on performance. Gait trainer treadmills have graphic information such as footsteps and targets for stride length and cues to “take longer step right” to help. Many pieces of equipment provide information about mileage, step count, calories, and reps per minute. They may also have target options with visual feedback comparing the target to the performance. This information should be shared with the patients so that they have feedback about their performance with results that therapists can use to encourage progression on the next visit.
POWER OF POSITIVE FEEDBACK
Rewards are very easy to provide, and patients of all ages respond to them. It can be as simple as a thumbs-up or “high five” sign, or more complicated such as points accrued on a video game. According to the study by design and IT professionals, the reward should be received regardless of the level of difficulty of the goal. Again, technology is increasing the availability of rewards for patients. For example, the Biodex gait trainer treadmill from Shirley, NY-headquartered Biodex Medical Systems Inc will provide rewards on the screen such as “good job” when the target stride length is reached. Treadmills and stepper machines that include a quarter-mile track on the screen provide rewards such as colored balls or arrows that light up the distance attained on the track. Even young children feel rewarded when they see the “green peas” on such a screen and want to continue walking to get another one.
FIT LIFESTYLE
While healthcare professionals are encountering an increasing challenge of a less fit society, a poorly conditioned body is not an inevitability. Physical therapists have a deep understanding of how the body functions, but also are in a position to get to know their patients and understand which activities and technologies are most likely to get them their buy-in. Combining these complementary components of care, physical therapists are well-positioned to move their patients to higher levels of fitness and, hopefully, toward a more fit lifestyle. PTP
Rosemary Peng, PT, MSPT, is a clinical specialist at Kessler Institute for Rehabilitation with specialties in neurology and pediatrics. She is a 1985 graduate of the Arcadia University PT program and has more than 30 years of experience in inpatient and outpatient rehabilitation, home care, early intervention, and school settings. For more information, contact PTPEditor@medqor.com.
References
- Brownson RC, Boehmer TK, Luke DA. Declining rates of physical activity in the United States: what are the contributors? Annu Rev Public Health. 2005;26:421-43
- Chen T, Kishimoto H, Honda T, et al. Patterns and levels of sedentary behavior and physical activity in a general Japanese population: the Hisayama study. J Epidemiol. 2018;28(5):260-265.
- Biswas A, Oh Pi, Faulkner GE, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Internal Med. 2015;162(2):123-132.
- Pinho CS, Caria ACI, et al. The effect of the COVID-19 pandemic on levels of physical fitness. Rev Assoc Med Bras. 2020;66 Suppl 2:34 – 37. DOI: 10.1590/1806-9282.66.S2.34
- Violant-Holz V, Gallego-Jiminez MG, et al. Psychological health and physical activity levels during the COVID-19 pandemic: A Systematic Review. Int J Environ Res Public Health. 2020;17(24):9419. DOI: 10.3390/ijerph17249419
- Dallinga J, Janssen M, van der Werf J, Walravens R, Vos S, Deutekorn M. Analysis of the features important for the effectiveness of physical activity–related apps for recreational sports: expert panel approach. JMIR Mhealth Uhealth. 2018;6(1):1-12.
[WEB] Physical Activity After Traumatic Brain Injury – ACRM
Posted by Kostas Pantremenos in TBI on October 9, 2021
Traumatic brain injury (TBI) refers to damage to the brain from a physical force. This can include falls, car accidents, or gunshots, among other causes. TBI can cause difficulties with cognition (thinking) and function (movement). More than 2.5 million Americans experience a TBI each year. Many individuals with TBI do not complete regular physical activity.
What is “physical activity”?
- •Physical activity is any bodily movement produced by skeletal muscles that results in the expenditure of energy
- •Exercise is a physical activity that is planned, structured, repetitive, and performed to improve health or fitness
- •The Health and Human Services Physical Activity Guidelines1 provide recommendations about the time and intensity of physical activity needed to maintain health and well-being
- •The Health and Human Services Physical Activity Guidelines1 advise individuals to get at least:
- ○150 minutes of moderate activity (eg, walking briskly, dancing, gardening) per week OR
- ○75 minutes of vigorous physical activity (eg, running, tennis, hiking uphill, heavy housework) per week AND
- ○2 or more days of strength training per week
Benefits of physical activity after TBI
- •Physical activity increases the release of growth factors in the brain that help build new brain cells2 and increase brain size,3 which leads to:
- •Social benefits of physical activity8
- ○Improved life satisfaction
- ○Decreased stress
- •Social benefits of group physical activity8
- ○Social interaction with peers
- ○Opportunities to build new friendships
- ○Increased communication skills
- •Physical health benefits of physical activity
Reasons you might not be physically active and ways to overcome them
There are many reasons why you may find it challenging to be physically active.14,15Table 1 identifies some of the barriers and potential solutions.Table 1Possible solutions to overcome barriers to physical activity
| Barriers to Physical Activity | Potential Solutions |
|---|---|
| Transportation | •Use public transportation or ride sharing applications •Ask family or friends |
| Access to fitness center | •Complete activity in a large room in your home •Go to the local park |
| Cost | •Find low cost or free activities such as brisk walking •Use resistance bands or household items as weights |
| Do not know how to exercise | •Ask a certified inclusive fitness trainer or physical therapist •Talk with your doctor |
| Cognition and memory | •Keep a consistent routine•Use a planner to schedule physical activity •Set reminders on electronic devices such as your phone •Use written step-by-step directions |
| Poor motivation | •Find a partner or group •Explore what inspires or motivates you and others |
| Fatigue | •Participate during times you have more energy •Start with tasks at home that do not cause fatigue •Know your limits and schedule rest breaks |
The key is to be as active as you can—do what you can when you can. Even if you can only tolerate a few minutes of physical activity at a time, try to do it 2 to 3 times per day. Gradually increase your activity goal to 30 minutes daily. Table 2 lists example activities and ways to modify them according to your fitness and functional levelsTable 2Examples of activities and modifications.
| Activities | Modification |
|---|---|
| Improve Endurance | |
| Walk | If too easy: increase the speed, time, or distance If too hard: slow down, take shorter walks more often |
| Bicycle | If too hard: use a stationary bicycle with a back rest to help with balance |
| Improve Leg Strength | |
| Squats: stand with legs shoulder-width apart and lower your buttocks toward the ground slowly before coming back up | If too easy: add weights or try 1 leg at a time If too hard: practice standing up from a chair |
| Heel raises: stand up on your tip toes | If too easy: do 1 leg at a time If too hard: hold on to the wall or a table for balance |
| Improve Arm Strength | |
| Bicep curls: hold a weighted object (such as a can of soup) in each hand at your side and bring up to the shoulder while bending your elbow | If too easy: increase the weight or use a resistance band by standing on the band with your feet If too hard: do without a weight |
| Shoulder abduction: hold a weighted object in each hand at your side and move your arms away from the body until they are parallel to the ground | If too easy: increase the weight or use a resistance band by standing on the band with your feet If too hard: do without a weight |
| Pushups: keep your hands on the ground next to your shoulders and toes on the floor. Push up from the ground keeping your body straight | If too easy: increase the number you do If too hard: put your knees on the ground when completing the movement. You can also do when standing next to a wall and push off from the wall |
| Improve Balance | |
| Yoga, tai chi, and leg strength exercises | If too easy: close your eyes If too hard: use a chair or the wall for challenging poses |
Your health care team can help you be more physically active
- •Consult your physician if you are unsure how to safely start adding more physical activity into your daily life
- •Physical therapists are rehabilitation professionals who diagnose and treat a variety of movement impairments associated with health-related conditions or injuries to improve quality of life
- •Certified inclusive fitness trainers have advanced training and can help safely adapt physical activities for individuals with physical, sensory, and cognitive disabilities
Resources for becoming more physically active
- •Move United (www.moveunitedsport.org/sports/adaptive-sports)
- •National Center on Health, Physical Activity and Disability (www.nchpad.org)
- •LoveYourBrain Yoga (www.loveyourbrain.com/yoga)
- •YMCA provides memberships with sliding scale payment (www.ymca.net)
Authorship
This page was developed by Shanti M. Pinto, MD (e-mail address: Shanti.Pinto@atriumhealth.org ); Eric M. Watson, PhD; Wendy A. Contreras, MD; Kaitlin A. Luffman, PT, DPT, CBIS; and Mark A. Newman, PhD, MPH.
Disclaimer
This information is not meant to replace the advice of a medical professional and should not be interpreted as a clinical practice guideline. This Information/Education Page may be reproduced for noncommercial use for health care professionals and other service providers to share with their patients or clients. Any other reproduction is subject to approval by the publisher.
Acknowledgment
Supported by the Brain Injury-Interdisciplenary Special Interest Group (BI-ISIG) Chronic Brain Injury Task Force.
References
- US Department of Health and Human Services
- Wogensen E.
- Malá H.
- Mogensen J.
- Erickson K.I.
- Voss M.W.
- Prakash R.S.
- et al.
- Richards M.
- Hardy R.
- Wadsworth M.E.J.
- Chin L.M.
- Keyser R.E.
- Dsurney J.
- Chan L.
- Colcombe S.J.
- Kramer A.F.
- Erickson K.I.
- et al.
- Grealy M.A.
- Johnson D.A.
- Rushton S.K.
- Eime R.M.
- Young J.A.
- Harvey J.T.
- Charity M.J.
- Payne W.R.
- Swift D.L.
- Johannsen N.M.
- Lavie C.J.
- Earnest C.P.
- Church T.S.
- Kovács E.
- Sztruhár Jónásné I.
- Karóczi C.K.
- Korpos A.
- Gondos T.
- Jain R.K.
- Vokes T.
- Chin L.M.K.
- Chan L.
- Woolstenhulme J.G.
- Christensen E.J.
- Shenouda C.N.
- Keyser R.E.
- Hassett L.
- Moseley A.M.
- Harmer A.R.
- Driver S.
- Ede A.
- Dodd Z.
- Stevens L.
- Warren A.M.
- Hassett L.M.
- Tate R.L.
- Moseley A.M.
- Gillett L.E.
Article Info
Publication History
Published online: February 17, 2021
Identification
DOI: https://doi.org/10.1016/j.apmr.2020.12.020
Copyright
© 2021 by the American Congress of Rehabilitation Medicine All rights reserved.
ScienceDirect
Access this article on ScienceDirect
Tables
- Table 1Possible solutions to overcome barriers to physical activity
- Table 2Examples of activities and modifications.
Related Articles
- Review of the Status of Physical Activity Research for Individuals With Traumatic Brain Injury
- Community-Based Physical Activity Interventions after Moderate to Severe Traumatic Brain Injury
- Characterizing Physical Activity and Sedentary Behavior in Adults With Persistent Postconcussive Symptoms After Mild Traumatic Brain Injury
- Physical Activity Intensity among Individuals with Traumatic Brain Injury During Inpatient Rehabilitation
- What Makes a Community-Based Physical Activity Program Successful for Adults With Moderate-Severe Traumatic Brain Injury?
