Introduction
Severe, persistent paresis occurs in over 40% of stroke patients (1) and is reported to significantly decrease their quality of life (2). Thus, much research has been conducted to develop interventions, with many specifically targeting upper extremity hemiplegia. Among the many examples of neuroscience-based rehabilitation (neuro-rehabilitation) strategies, there is strong evidence supporting robotic therapy, constraint-induced movement therapy (CIMT), and task-oriented training (3, 4).
Robotic therapy is considered an effective intervention for mild to severe hemiplegic arm (5, 6), and is cost-effective for chronic stroke patients in terms of both manpower and medical costs (7, 8). However, its effects may be limited for some patients. Some researchers have found that robotic therapy effectively improves arm function as measured by the Fugl-Meyer Assessment (FMA) (9) and Action research arm test (ARAT) (10), but does not improve the use of the affected arm in activities of daily living (ADL) as measured by the Motor activity log (MAL)-14 (11) and by analysis of data from an accelerometer attached to the affected arm (6, 12–14).
On the contrary, CIMT is the most well-established intervention for improving the use of the affected arm in ADL (15). CIMT consists of three components: (1) a repeated task-oriented approach, (2) a behavioral approach to transfer the function gained during training to actual life (also called the “transfer package”), and (3) constraining use of the affected arm. Some researchers consider the transfer package the most important component of CIMT. In fact, research has shown that usage of the affected arm in daily life is significantly different between patients treated with and without the transfer package component (16, 17). However, many therapists question whether CIMT could benefit their patients because of the shortage of sites possessing the clinical resources to provide the intervention for the long duration required for effectiveness (18).
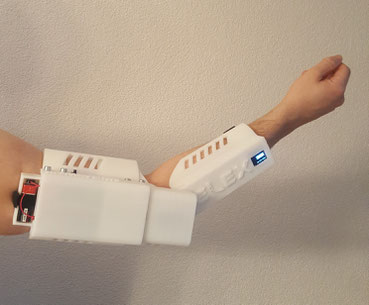
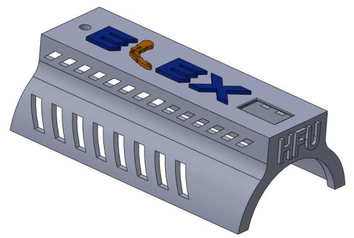
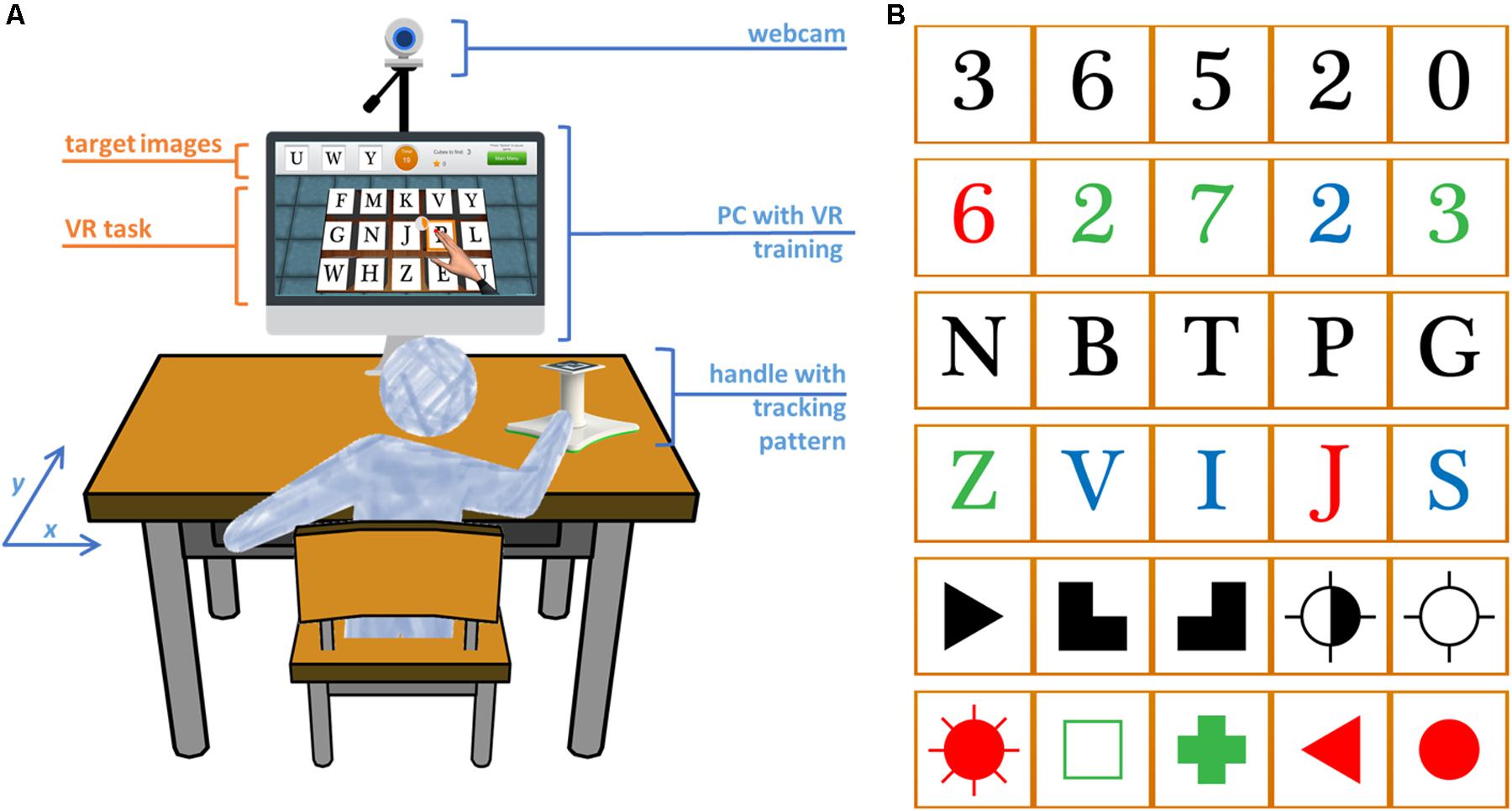
Therefore, there is an urgent need to establish an effective therapeutic approach, especially for upper-limb hemiplegia during the chronic stage of stroke recovery for which there are few clinical resources (In Japan, the insurance system only allows 260 min per month). Therefore, we will compare the efficacy of several therapy methods. As a control, we will monitor changes in arm function in patients undergoing a short, standard rehabilitation by a therapist and standard self-training (control group). This will be compared to similar self-training including robotic therapy with the ReoGo-J device as an adjuvant therapy (RT group). Finally, the robotic therapy will be compared to combined therapy including robotic therapy and CIMT (CT group). Through these comparisons, we will investigate the effect of robotic therapy, both alone and in combination with CIMT, which we hypothesize will complement each other in chronic stroke rehabilitation. Here, we report the structure and protocol of a multi-center, randomized controlled trial.[…]