Posts Tagged ABI
[WEB] Lifelong Adjustment and Behavioral Changes with TBI/ABI
Posted by Kostas Pantremenos in Caregivers, TBI on January 18, 2023
By Leif E. Leaf, Ph.D.
Life after a brain injury is different, but worth living! The changes that happen after a brain injury often result in lifelong consequences and challenges. As the physical recovery becomes more stable, the cognitive and behavioral challenges remain. The progress and gains made in physical therapy, occupational therapy, speech therapy, and adaptive functioning can help with a person’s recovery. The cognitive and behavioral challenges, however, continue to impact one’s success in reentering community and evolving into the new “person.”
The impact of changes to behavior after brain injury
The neurobehavioral consequences of a brain injury can have a long-term impact on adjustment, relationships, social interaction, vocational reentry, and life satisfaction. Like it or not we live in a social oriented society and culture. As social beings, we need interaction, support, feedback, and positive regard from those we care about.
When we think of behavior, we need to recognize how complicated it is to manage all the changes in life. One way to understand the challenges of behavior issues after a brain injury is to break behavior down into three separate parts.
The first part to remember is that behavior is controlled by the command center, that three-pound universe called the brain. A major influence on behavior will be the type of injury, severity, and integrity of the brain. Damage to the frontal and temporal lobes is common in traumatic brain injuries and often involved with acquired brain injury, and behavioral issues can arise due to the injury to the brain’s communication. Control issues with the primary areas of self-management can arise as well. Our frontal-temporal areas have been shown to be critical for integrating and assessing cognitive, emotional, and social events in one’s world. Damage to these areas can result in disinhibition, emotional discontrol, and reduced ability to manage everyday life. It is important to remember that a lack of insight, confusion, or inability to recognize the effects of their actions along with poor motivation may have an organic basis that is misattributed to intentional behavioral incidents. The person is not intentionally being disagreeable.
Secondly, the person injured has a history and a personality, and nothing happens outside the realm of who they are and what they were like at the time of the injury. The person’s social style, personality style, and their sense of self are critical in assessing and intervening with behaviors. A family member who has lived with the person has insight into their values and how they managed anger and frustration before the injury. Generally, after an injury the person will be like their old self only at times exaggerated.
Finally, the environment where a behavior occurs can be telling. From a management perspective, the environment is generally the easiest factor to control. You may see certain behaviors in some settings but not in others, be aware of these. The person may have sensitivities to how differing settings impact them. Knowing this can go a long way to reducing behavioral incidents. After a brain injury, a person may easily be overstimulated by an environment that is too active. If so, they can be removed or redirected. This is where knowing the person’s preferences can be helpful.
When dealing with behavior, be aware that what may be labeled inappropriate behavior may in fact be the residual deficits from the injury. Understanding the changes in the brain and awareness of the cognitive, personality and social history of the person can help in managing the behavior and creating a safe environment.
Addressing behaviors
In looking at some specific situations in which behavior may be an issue there are some important fundamentals to review. The first is not to take behaviors personally. The situation, the person’s injury, and how you respond all need to be considered. The person’s pre-injury personality will generally be exaggerated from their preinjury personality style. They may feel anxious, agitated, and angry that they are different without appreciating the severity of their injuries.
Always try to remain calm and in charge of your emotional responses. When dealing with the person, try and maintain the 3 C’s: stay cool, calm, and in control (of yourself). In the hospital or rehabilitation center, the person with a brain injury was in a controlled environment with staff that are trained to assist and manage behavioral issues. In the community that responsibility falls on the person and the family or significant others.
After a brain injury, new learning may be difficult due to memory changes, poor attending, concentration skills, lack of awareness of deficits and limited insight. The inability to see the other person’s point of view or to recognize one’s own responsibility is common with frontal-lobe injuries. Taking it slowly and intentionally is critical to helping the person learn new and effective strategies for self-control.
When addressing behaviors, try not to make it a control issue. You want the person to participate willingly to achieve the desired outcome. Talk to the person, discuss the situation if able. Starting here allows you to move on by working together to find a solution. Always listen and treat them with respect.
One way to encourage participation is to offer choices. This gives a sense of control and not being forced to do something. As with most brain injuries, cognitive skills can be a challenge. Try to avoid arguing and reasoning when emotions are high, they can’t process what you are saying. Take a timeout and redirect the person, come back to it after things have cooled.
Remember, we all like to feel good and needed, and it is critical that you reinforce the good and whenever possible ignore the bad. When you can catch them doing it right, it will go a long way to building positive self-management.
The key to behavior management is to understand the injury, the person and control the environment. Treat a person according to their potential, not their disability.
[WEB] Investigating Brain Activity After Acquired and Traumatic Brain Injury: Applications of Functional MRI
Posted by Kostas Pantremenos in Radiology/Imaging technology, TBI on December 3, 2022
About this Research Topic

Every year, the lives of millions of people are affected by traumatic (TBI) or acquired brain injury (ABI). The search for treatments and interventions that aid in TBI and ABI after-effects should be the priority in modern clinical research. In recent decades there has been great progress in functional neuroimaging techniques and analysis methods. However, a disconnect between functional neuroimaging findings and their application to clinical settings remains. Examining the mechanism of brain injury can greatly advance our knowledge of the consequences and functional outcomes of ABI and TBI. Further, it can help characterize the nature of cognitive deficits after brain injury. More importantly, understanding how the functioning of the brain changes after ABI and TBI has the potential to promote development of targeted and effective interventions.
There are methodological barriers that might explain why functional neuroimaging has not received sufficient attention in these patient groups.
Functional neuroimaging in brain injury presents substantial challenges to researchers. Both patient populations are diverse in terms of brain anatomy and lesion locations. Selecting the appropriate control group and control condition can be challenging. The most significant challenge is accurate measurement and interpretation of signal in the damaged brain, because it is not well known how the blood flow to non-damaged areas is affected by the lesion. The main goal in this area of study is to disentangle blood flow effects due to meaningful brain activity and those due to lesion. Alternative methods of imaging, such as perfusion weighted imaging using ASL (arterial spin labeling) are only now beginning to be explored.
Despite the above challenges, functional neuroimaging is still a fruitful and promising area of investigation in TBI and ABI with substantial knowledge and insight into the mechanisms of brain injury remaining to be gained. The ultimate goals of functional neuroimaging in TBI and ABI are in line with the need for solution-oriented research in today’s society. This under-studied area bridges human neuroscience and neurology.
In this Research Topic, we present a collection of original research and review articles focused on functional neuroimaging in TBI and ABI, including task-based functional Magnetic Resonance Imaging (fMRI), resting state MRI, ASL, PET, etc. The assembled articles address
1) how the challenges of working with lesioned brain can be overcome,
2) how findings on cognitive function after ABI and TBI can be linked with brain mechanisms, and
3) how findings about brain mechanisms can be applied to improving quality of care and rehabilitation strategies.
[WEB] About brain injury
Posted by Kostas Pantremenos in TBI on September 26, 2022
An acquired brain injury (ABI) is an injury caused to the brain since birth. There are many possible causes, including a fall, a road accident, tumour and stroke.
This section gives an overview of the brain, brain injury and the practical issues that can arise.
It is divided into sections for individuals who are affected by brain injury, professionals who work in the field of brain injury, and further information about brain injury.
Because of your cookies settings you are unable to see this video. If you’d like to view it, please visit our cookies page, scroll down and click the ‘Cookies Settings’ button. Enabling cookies will allow you to view all of the content on our website. After enabling cookies (above link) please click to refresh the page to show the video.
Information for individuals
Find out about how acquired brain injury affects survivors, family members, carers and the people around them. We provide information to help at the different stages of brain injury, from hospital to home.
Types of brain injury
Acquired brain injury can have a number of different causes. Some of the most common types of brain injury include:
- Traumatic brain injury (for instance road traffic collisions, falls or assaults)
- Minor head injury and concussion (loss of consciousness of less than 15 minutes)
- Aneurysm (also known as a cerebral aneurysm)
- Brain haemorrhage (also known as a haemorrhagic stroke)
- Brain tumour
- Carbon monoxide poisoning
- Encephalitis
- Hypoxic/anoxic brain injury (caused a reduction or loss of oxygen to the brain)
- Meningitis
- Stroke
Effects of brain injury
A brain injury can lead to a wide range of effects. While many people recover quickly after a minor head injury (often known as concussion), this is not always the case and people may experience longer-term effects.
The more severe the brain injury, the longer-term and more pronounced the effects are likely to be. Some people may spend time in a coma, or experience a more prolonged reduced awareness state. During the early stages of recovery, brain injury survivors often go through a stage called Post-traumatic amnesia, where they have no continuous memory of day-to-day events and their behaviour may be very uncharacteristic and confused.
A brain injury can cause behavioural and emotional changes, hormonal imbalances, difficulties with cognition and memory, a range of communication problems, physical effects and, very commonly, fatigue.
Hospital treatment and early recovery after brain injury
The time immediately after the injury is bound to be full of worry and uncertainty for everyone concerned.
We provide information on the different stages of recovery, from the time in the hospital and early rehabilitation through to discharge. Families may be able to access a grant to help with the unexpected costs of brain injury by applying to our Emergency Fund.
You can also set up a page on our I’m calling about Chris website to post updates on your loved one’s situation and allow family and friends to keep up-to-date. They can also access our information that explains how to support a family that is dealing with brain injury.
Rehabilitation and continuing care after brain injury
Rehabilitation aims to help the brain learn alternative ways of working in order to minimise the long-term impact of the brain injury. Rehabilitation also helps the survivor and the family to cope successfully with any remaining disabilities.
In this section you can find out more about what brain injury rehabilitation involves, and get information on the rehabilitation team that you will be working with.
After the initial phase of rehabilitation is complete, you may require continuing care, and want to find out about ways you can self-direct your support.
Practical issues after brain injury
A brain injury can lead to a wide range of difficulties in day-to-day life. For many people, a priority may be to seek financial support. This could involve getting legal advice to pursue compensation, applying for welfare benefits or applying for a grant from the Headway Emergency Fund.
In the longer-term, many brain injury survivors may want to return to driving, or get back to work or education.
They may also qualify for a Brain injury identity card, which is designed to provide brain injury survivors with added confidence in everyday social scenarios, and ensure they get the right support if they come into contact with the police.
Relationships after brain injury
For some people, the emotional, behavioural, physical and cognitive changes of brain injury can have an impact on existing and future relationships.
We explain how a brain injury effects relationships, with further information for partners and friends. We also provide in-depth information on an often overlooked issue – the affect of brain injury on sex and sexuality.
There is also useful information to help people with brain injury to cope with parenting and supporting children.
Information library
You can browse our full range of free booklets and factsheets in the information library.
Brain injury and me
Brain injury and me is an innovative and exciting website that raises awareness of brain injury through personal stories.
The Living with brain injury section contains a wide range of practical advice, incorporating the experiences and views of survivors and carers.
You can find the information you need using the menu or the quick links below. If you can’t find what you are looking for or have any more questions, please contact our helpline.
[BLOG POST] Understanding Brain Injuries
Posted by Kostas Pantremenos in Educational, TBI on September 24, 2022
Understanding brain injuries: What is an acquired brain injury?
An acquired brain injury (ABI) is an injury to the brain that occurs after birth. It is not hereditary, congenital, degenerative, or induced by birth trauma. There are two basic types of acquired brain injury: traumatic and non-traumatic.
Traumatic brain injury (TBI) is the most common form of acquired brain injury. It occurs when a sudden trauma causes damage to the brain. TBI can result when the head violently hits an object, as in a car crash, or when an object penetrates the skull and enters the brain as in a shooting. Symptoms of a TBI can be mild, moderate, or severe, depending on the extent of the injury to the brain. For a detailed breakdown of the causes and symptoms of TBI, read this Mayo Clinic overview.
Far and away the leading cause of death and disability among persons under the age of 45, TBI strikes 1.7 million Americans each year, with over 50,000 dying of their injuries. In addition, the CDC estimates that 5.7 million Americans are permanently disabled with Traumatic Brain Injury – roughly 2% of the population! Millions more whose injuries do not quite meet the rigorous standard of legal disability struggle with life-altering deficits.
No one is immune: Toddlers on the playground, young adults out for a joy ride, weekend warriors on their mountain bikes, and seniors on stairs. However, falls are the single most significant single cause of TBI – 40%, comprised mainly of the youngest and oldest among us. Children and young adults predominantly suffer sports-related concussions or other brain injuries, as well as auto accidents. In the middle decades, we are most likely to be involved in a motor vehicle accident or an assault. Older persons are the most likely to succumb to their injuries. Overall, men are three times more likely to die from an injury than women.
The other large class of acquired brain injuries is non-traumatic acquired brain injuries, the vast majority of which are strokes. A stroke occurs when the blood supply to part of one’s brain is interrupted or reduced, preventing brain tissue from getting oxygen and nutrients. Brain cells begin to die in minutes. There are two leading causes of stroke: a blocked artery (ischemic stroke) or leaking or bursting blood vessels (hemorrhagic stroke). For a detailed breakdown of the causes and symptoms of stroke, read this overview from the Mayo Clinic:
Over 800,000 Americans suffer a stroke each year, with 130,000 dying. Remarkably, 34% of stroke victims are under the age of 65. Including stroke, TBI, and other forms of acquired brain injury (such as aneurysm, drowning, drug overdose, poisoning, smoke inhalation, carbon monoxide poisoning, heart attacks, etc.), brain injuries represent one of the top public health challenges. An astounding 2.5 million injuries per year at an annual cost of care of approximately $110 billion – 25% more than the cost of care for people with cancer! Brain injury is often a lifelong challenge for survivors, families, and loved ones.
Conventional medicine takes survivors of severe ABI only so far, often ending at the nursing home door or heavily medicated at home, facing long empty hours and overwhelming family resources. Safe alternative therapies are not merely a reasonable option; they may be necessary.
Every one of the millions of persons who suffer an ABI begins a journey none of us would choose to take, yet millions inevitably will. The BART Foundation provides, in an accessible form, knowledge of safe alternative therapies for brain injuries– which ones are likely to help, where they can be found, and how to afford them. We are dedicated to assisting survivors in living more fulfilling, productive, and joyful lives. Our outreach includes survivors, caregivers, and health professionals.
[Abstract] “It gave her that soft landing”: Consumer perspectives on a transitional rehabilitation service for adults with acquired brain injury
Posted by Kostas Pantremenos in REHABILITATION on May 19, 2022
ABSTRACT
Transitional rehabilitation service models for people with acquired brain injury (ABI) may address sub-optimal support for individuals returning home after hospitalization for ABI. This study investigated perspectives of people with ABI and close others who received transitional rehabilitation. A qualitative study involving semi-structured interviews with 10 individuals with ABI and 12 associated close others was conducted as part of a mixed-method evaluation of an Australian transitional rehabilitation service (TRS) pilot project. Thematic analysis based on the Framework method was conducted independently by two researchers. Three broad themes illustrated participants’ experience of the TRS: (1) structure after hospital discharge; (2) a “soft landing”; and (3) equipped for community living. Findings suggest that home-based, interdisciplinary transitional rehabilitation after hospital discharge was perceived as an important stage of rehabilitation by participants. Valued features relate to post-hospital rehabilitation structure: a single point of contact to facilitate organization and information exchange, a known discharge destination, and consistent communication; support and therapy within a familiar home environment; and being equipped with relevant knowledge and strategies to manage ongoing challenges. Further research exploring the experiences of individuals with ABI without close family or social support, and research capturing longitudinal outcomes from transitional rehabilitation is recommended.
[WEB] Brain Injury Overview – Brain Injury Association of America
Posted by Kostas Pantremenos in Educational, TBI on April 22, 2022
ABOUT BRAIN INJURY

Brain Injury Overview
An acquired brain injury (ABI) is an injury to the brain that is not hereditary, congenital, degenerative, or induced by birth trauma. Essentially, this type of brain injury is one that has occurred after birth. The injury results in a change to the brain’s neuronal activity, which affects the physical integrity, metabolic activity, or functional ability of nerve cells in the brain.
There are two types of acquired brain injury: traumatic and non-traumatic.
A traumatic brain injury (TBI) is defined as an alteration in brain function, or other evidence of brain pathology, caused by an external force. Traumatic impact injuries can be defined as closed (or non-penetrating) or open (penetrating).
Often referred to as an acquired brain injury, a non-traumatic brain injury causes damage to the brain by internal factors, such as a lack of oxygen, exposure to toxins, pressure from a tumor, etc. Read on for an overview of some of the common causes of brain injury.
| TRAUMATIC BRAIN INJURY CAUSES | NON-TRAUMATIC BRAIN INJURY CAUSES |
|---|---|
| Falls Assaults Motor Vehicle Accidents Sports/Recreation Injuries Abusive Head Trauma (Shaken Baby Syndrome) Gunshot Wounds Workplace Injuries Child Abuse Domestic Violence Military Actions (Blast Injury) | Stroke (Hemorrhage, Blood Clot) Infectious Disease Meningitis Encephalitis Seizure Electric Shock Tumors Metabolic Disorders Neurotoxic Poisoning (Carbon Monoxide, Lead Exposure) Lack of Oxygen (Drowning, Choking, Hypoxic/Anoxic Injury) Drug Overdose Aneurysm |
While the list above is certainly not exhaustive, it includes many of the most common causes of injury. Click through the “Continue Reading” sections below to learn more about injury severity, terms you might hear at the hospital, and what to expect after a brain injury.
For personalized support and resources, contact BIAA’s National Brain Injury Information Center at 1-800-444-6443 or email us at info@biausa.org. You can also visit the Frequently Asked Questions of our website for more information.
CONTINUE READING
Functions of the Brain
Brain Injury Overview
Understanding the Injury
After the Injury
Injury Severity
For more visit site.
[Abstract] Return-to-driving following acquired brain injury: A neuropsychological perspective
Posted by Kostas Pantremenos in TBI on March 29, 2022
Abstract
Background: Return to driving after an acquired brain injury (ABI) has been positively associated with return to employment, maintenance of social relationships, and engagement in recreational and other community activities. Safe driving involves multiple cognitive abilities in a dynamic environment, and cognitive dysfunction resulting from ABI can negatively impact driving performance.
Objective: This manuscript examines the post-injury return-to-driving process, including performances on the in-office and on-road assessments, and the role of a rehabilitation neuropsychologist in helping patients resume driving.
Method: In this study, 39 of 200 individuals (approximately 20%) treated at an outpatient neurorehabilitation facility, who performed satisfactorily on a pre-driving cognitive screening, completed a behind-the-wheel driving test.
Results: Of the 200 individuals, 34 (87%) passed the road test. Among the remaining five individuals who did not pass the road test, primary reasons for their failure included inability to follow or retain examiner directions primarily about lane position, speed, and vehicle control. The errors were attributable to cognitive difficulties with information processing, memory, attention regulation, and dual tasking.
CONCLUSION The rehabilitation neuropsychologist contributed to the process by assessing cognition, facilitating self-awareness and error minimization, providing education about driving regulations and safety standards, and preparing for the road test and its outcomes.
Similar articles
- Characterizing on-road driving performance in individuals with traumatic brain injury who pass or fail an on-road driving assessment.Stolwyk RJ, Charlton JL, Ross PE, Bédard M, Marshall S, Gagnon S, Gooden JR, Ponsford JL.Disabil Rehabil. 2019 Jun;41(11):1313-1320. doi: 10.1080/09638288.2018.1424955. Epub 2018 Jan 15.PMID: 29334804
- Safe return to driving following severe acquired brain injury: role of a short neuropsychological assessment.Saviola D, De Tanti A, Conforti J, Posteraro L, Manfredini A, Bagattini C, Basagni B.Eur J Phys Rehabil Med. 2018 Oct;54(5):717-723. doi: 10.23736/S1973-9087.17.04905-X. Epub 2017 Nov 16.PMID: 29144107
- Awareness of deficits and on-road driving performance.Griffen JA, Rapport LJ, Bryer RC, Bieliauskas LA, Burt C.Clin Neuropsychol. 2011 Oct;25(7):1158-78. doi: 10.1080/13854046.2011.609841. Epub 2011 Sep 27.PMID: 21951140
- Relationships between cognitive functions and driving behavior in Parkinson’s disease.Ranchet M, Broussolle E, Poisson A, Paire-Ficout L.Eur Neurol. 2012;68(2):98-107. doi: 10.1159/000338264. Epub 2012 Jul 4.PMID: 22759624 Review.
- Community reintegration following holistic milieu-oriented neurorehabilitation up to 30 years post-discharge.Perumparaichallai RK, Lewin RK, Klonoff PS.NeuroRehabilitation. 2020;46(2):243-253. doi: 10.3233/NRE-192968.PMID: 32083599
[Abstract] Psychological status and role of caregivers in the neuro-rehabilitation of patients with severe Acquired Brain Injury (ABI)
Posted by Kostas Pantremenos in Caregivers, Neuroplasticity on November 16, 2020
ABSTRACT
Objective
To investigate the relationships between (a) the psychological status of the caregiver, (b) the specific features of caregiving as perceived by the cognitive therapist in neuro-rehabilitation, (c) the caregivers’ subjective approach to neuro-rehabilitation, and (d) the functional outcome of the patient.
Methods
Twenty-four patients with severe acquired brain injury and their 24 caregivers participated in this observational study. Caregivers underwent a psychological assessment examining emotional distress, burden and family strain; their subjective approach to neuro-rehabilitation has been evaluated by two specific answers. The patients’ cognitive therapists responded to an ad-hoc questionnaire, namely the “Caregiving Impact on Neuro-Rehabilitation Scale” (CINRS), evaluating the features (i.e., amount and quality) of caregiving. Finally, the functional outcome of the patient was assessed through standardized scales of disability and cognitive functioning.
Results
The caregivers’ psychological well-being was associated to the features of caregiving, to the subjective approach to neuro-rehabilitation, and to the functional recovery of their loved ones. A better caregivers’ approach to neuro-rehabilitation was also associated to an overall positive impact of caregiving in neuro-rehabilitation and to a better functional outcome of the patients.
Conclusions
We posited a virtuous circle involving caregivers within the neuro-rehabilitation process, according to which the caregivers’ psychological well-being could be strictly associated to a better level of caregiving and to a better functional outcome of the patients that, in turn, could positively influence the caregivers’ psychological well-being. Although preliminary, these results suggest a specific psycho-educational intervention, aimed at improving the caregivers’ psychological well-being and at facilitating their caring of the loved one.
[ARTICLE] The Use of Therapeutic Music Training to Remediate Cognitive Impairment Following an Acquired Brain Injury: The Theoretical Basis and a Case Study – Full Text
Posted by Kostas Pantremenos in Cognitive Rehabilitation, Music/Music therapy on September 17, 2020
Abstract
Cognitive impairment is the most common sequelae following an acquired brain injury (ABI) and can have profound impact on the life and rehabilitation potential for the individual. The literature demonstrates that music training results in a musician’s increased cognitive control, attention, and executive functioning when compared to non-musicians. Therapeutic Music Training (TMT) is a music therapy model which uses the learning to play an instrument, specifically the piano, to engage and place demands on cognitive networks in order to remediate and improve these processes following an acquired brain injury. The underlying theory for the efficacy of TMT as a cognitive rehabilitation intervention is grounded in the literature of cognition, neuroplasticity, and of the increased attention and cognitive control of musicians. This single-subject case study is an investigation into the potential cognitive benefit of TMT and can be used to inform a future more rigorous study. The participant was an adult male diagnosed with cognitive impairment as a result of a severe brain injury following an automobile accident. Pre- and post-tests used standardized neuropsychological measures of attention: Trail Making A and B, Digit Symbol, and the Brown– Peterson Task. The treatment period was twelve months. The results of Trail Making Test reveal improved attention with a large decrease in test time on both Trail Making A (−26.88 s) and Trail Making B (−20.33 s) when compared to normative data on Trail Making A (−0.96 s) and Trail Making B (−3.86 s). Digit Symbol results did not reveal any gains and indicated a reduction (−2) in free recall of symbols. The results of the Brown–Peterson Task reveal improved attention with large increases in the correct number of responses in the 18-s delay (+6) and the 36-s delay (+7) when compared with normative data for the 18-s delay (+0.44) and the 36-s delay (−0.1). There is sparse literature regarding music based cognitive rehabilitation and a gap in the literature between experimental research and clinical work. The purpose of this paper is to present the theory for Therapeutic Music Training (TMT) and to provide a pilot case study investigating the potential efficacy of TMT to remediate cognitive impairment following an ABI.
1. Introduction
An acquired brain injury (ABI) can result in impairment in a variety of domains including motor, speech, emotional, and cognitive. Cognitive impairment is the most common sequelae following an ABI [1,2,3,4] and is a result of deficit in one or more areas of cognition such as the various forms of attention, working memory, memory, executive function, or processing speed [5,6,7,8,9,10,11]. An individual with cognitive impairment may experience challenge to suppress distraction, remain on task, shift between tasks, follow directions, organize and initiate a response, or have difficulties with memory. Cognitive impairment can impact participation and progress in rehabilitation therapies for any of the above domains due to reduced attention, poor executive functioning, or impaired memory. The inability to attend to instructions of the therapist, to cognitively plan and organize a response, or to remember rehabilitation objectives outside the therapy session can potentially disqualify an individual from participation in rehabilitative programs or may impede progress in them. Furthermore, cognitive impairment is reported by family and caregivers as a significant source of stress [8,12,13,14]. Addressing cognitive impairment should be a priority in patient treatment following an acquired brain injury. Therefore, it is important to have on-going research into potentially effective cognitive rehabilitation tools.Music training has been noted in the literature to impact areas of non-musical functioning including phonological awareness [15], speech processing [16], listening skills [17], perceiving speech in noise [18] and reading [19,20]. Of significance to the theory of Therapeutic Music Training, the literature demonstrates the impact of music training on cognitive abilities including attention and executive functioning [21,22,23,24,25,26,27].Therapeutic Music Training (TMT) is a music therapy model in which the use of music training, specifically learning to play the piano, is used to address and remediate cognitive impairment following an acquired brain injury [28]. TMT is informed by clinical work and is grounded in literature. The hypothesis of the efficacy of TMT to remediate cognitive impairment is supported by literature regarding the influence of music training on cognition [23,24,25,29], musician’s enhanced abilities in attention, working memory, and cognitive control [26], theories of attention [30,31,32,33,34,35] and the neuroplasticity of the brain, including following injury [36,37,38,39,40]. Because of the engagement of the prefrontal cortex and the demands placed on working memory and attention during TMT, it can be an effective tool to address cognitive impairment. Although functionally interconnected, specific aspects of cognition such as working memory, attention, executive function, and memory are targeted in TMT tasks. TMT is a remedial approach to cognitive rehabilitation, that is, the goal is to drive, strengthen, and improve the underlying neural processes involved in the target cognitive areas. This is in contrast to a compensatory approach to cognitive rehabilitation, in which the goal is to provide the individual with strategies and accommodations to deal with the outcomes of cognitive impairment. The tangible outcome of producing a song provides motivation for the client to engage in cognitive rehabilitation and to remain in the rehabilitative process for an extended period of time as is required to stimulate a neuroplastic response and for the remediation of neural processing to take place.TMT is distinct from modified music education in that the goal of TMT is the remediation of cognitive processes rather than music performance. Tasks involved in learning to play the piano are designed with the goal of placing demands on the various components of cognition. The sequencing and pacing of tasks are determined by the cognitive goals with consideration to target cognitive processes and the time required to drive and strengthen the networks involved. Novelty and the gradual increase in complexity of tasks are utilized to place on-going demands on attention networks and to gradually benefit higher cognitive processes. This is in contrast to modified music education, in which the primary goal is the acquisition of musical abilities and performance.TMT is distinct from other models of music therapy in that it uses music training as the intervention for rehabilitative purposes. TMT contrasts from other music therapy models which use music primarily for expressive purposes, lack corrective feedback from the therapist, or use isolated music tasks which are not intended as music training. TMT is distinct from Neurologic Music Therapy (NMT) [41] in addressing cognitive goals as NMT does not use music training in its music-based rehabilitative interventions. Bruscia highlighted the importance of the music therapist’s “non-judgemental acceptance of what the client does musically” [42] (p. 3). While the TMT therapist would express empathy and support to the client, s/he would also provide constructive and corrective feedback as required in the learning to play an instrument. As in other models of music therapy, the therapist’s use-of-self and the role of the client–therapist relationship are important contributors to the success of the therapy.Remarkably, much of cognitive rehabilitation is not grounded in the literature [36,43,44,45]. This may be due in part to the fact that rehabilitation therapy used to address cognitive impairment is most often based on a compensatory approach, accommodating or supporting the impairment, rather than attempting to remediate the cognitive processes that have been impaired. While the use of music and instrument playing for motor rehabilitation has been widely investigated [41,46,47,48], there is sparse literature investigating the potential efficacy of music-based cognitive rehabilitation interventions. This paper provides a brief introduction to the theory for TMT. This case study investigates the hypothesis of the potential effectiveness of therapeutic music training, TMT, to remediate cognitive impairment and serves as a pilot project to inform future, more rigorous studies. This investigation can contribute to the literature regarding music-based cognitive rehabilitation and inform clinical practice. There is a gap between cognitive experimental research and treatment applications [49]. The hypothesis for TMT has been informed by clinical work and this study can help fill in the gap between experimental research and clinical application. […]
Continue —-> https://www.mdpi.com/2227-9032/8/3/327/htm
[ARTICLE] Virtual reality-based treatment for regaining upper extremity function induces cortex grey matter changes in persons with acquired brain injury – Full Text
Posted by Kostas Pantremenos in Paretic Hand, REHABILITATION, Virtual reality rehabilitation on September 14, 2020
Abstract
Background
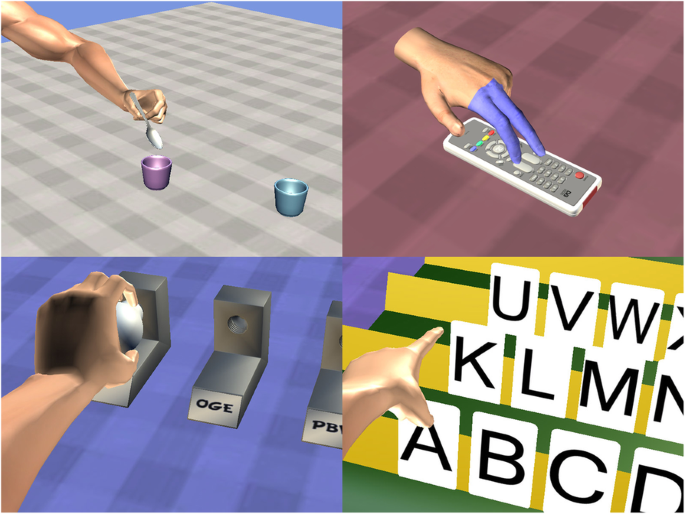
Individuals with acquired brain injuries (ABI) are in need of neurorehabilitation and neurorepair. Virtual anatomical interactivity (VAI) presents a digital game-like format in which ABI survivors with upper limb paresis use an unaffected limb to control a standard input device and a commonplace computer mouse to control virtual limb movements and tasks in a virtual world.
Methods
In a prospective cohort study, 35 ambulatory survivors of ABI (25/71% stroke, 10/29% traumatic brain injury) were enrolled. The subjects were divided into three groups: group A received VAI therapy only, group B received VAI and physical/occupational therapy (P/OT), and group C received P/OT only. Motor skills were evaluated by muscle strength (hand key pinch strength, grasp, and three-jaw chuck pinch) and active range of motion (AROM) of the shoulder, elbow, and wrist. Changes were analyzed by ANOVA, ANCOVA, and one-tailed Pearson correlation analysis. MRI data was acquired for group A, and volumetric changes in grey matter were analyzed using voxel-based morphometry (VBM) and correlated with quantified motor skills.
Results
AROM of the shoulder, elbow, and wrist improved in all three groups. VBM revealed grey matter increases in five brain areas: the tail of the hippocampus, the left caudate, the rostral cingulate zone, the depth of the central sulcus, and the visual cortex. A positive correlation between the grey matter volumes in three cortical regions (motor and premotor and supplementary motor areas) and motor test results (power and AROM) was detected.
Conclusions
Our findings suggest that the VAI rehabilitation program significantly improved motor function and skills in the affected upper extremities of subjects with acquired brain injuries. Significant increases in grey matter volume in the motor and premotor regions of affected hemisphere and correlations of motor skills and volume in nonaffected brain regions were present, suggesting marked changes in structural brain plasticity.
Background
Neurological disorders, including acquired brain injuries (ABIs) are important causes of disability and death worldwide [1, 2]. Although age-standardized mortality rates for ischemic and hemorrhagic strokes have decreased in the past two decades, the absolute number of stroke survivors is increasing, with most of the burden in low- and middle-income countries [3]. Another major issue is that trends toward increasing stroke incidence at younger ages has been observed [4]. Moreover, this type of ABI is the leading cause of long-term disability in the United States, with an estimated incidence of 795,000 strokes yearly [2].
In more than 80% of stroke survivors, impairments are seen in at least one of the upper limbs. Six months after a stroke, 38% of patients recover some dexterity in the paretic arm, though only 12% recover substantial function even in spite of having received physical/occupational therapy (P/OT) [5]. Only a few survivors are able to regain some useful function of the upper limb. Failing to achieve useful function has highly negative impacts on the performance of daily living activities [6, 7]. Regaining control and improving upper limb motor function after ABIs are therefore crucial goals of motor system rehabilitation. In left-sided limb impairment, neglect syndrome can contribute to a worsened clinical state, making the alleviation of symptoms even more difficult to achieve. Mirror therapy has been reported as a promising approach to improve neglect symptoms [8, 9].
MRI has been used to track changes in brain connectivity related to rehabilitation [10], and several studies of healthy individuals playing off-the-shelf video games have demonstrated changes in the human brain resulting from interactions in a virtual world (VW) [11, 12]. Furthermore, playing video games results in brain changes associated with regaining improved, purposeful physical movements [13, 14]. The socio-cultural relevance of virtual reality (VR) and VW applications lies, more generally, in the fact that these technologies offer interactive environments to users. These interactive environments are actually present in the users’ experiences while less so in the world they share as biological creatures [15]. The way in which we engage with VWs allows for rehabilitation exercises and activities that feel similar to their actual physical world counterparts [11]. In the past two decades, researchers have demonstrated the potential for the interactive experiences of VWs to provide engaging, motivating, less physically demanding, and effective environments for ABI rehabilitation [9, 16,17,18].
One of the suitable rehabilitation methods seems to be exercises and tasks in VW called virtual anatomical interactivity (VAI) [19]. This method provides sensory stimulation / afferent feedback and allows the independent control of an anatomically realistic virtual upper extremity capable of simulating human movements with a true range of motion. ABI survivors are able to relearn purposeful physical movements and regain movement in their disabled upper extremities [19]. Contrary to conventional therapy, which exercises impaired upper limbs to improve limb movement, the general VAI hypothesis is that brain exercises alone (or combined with traditional therapy) may positively influence neuroplastic functions. In the VW, subjects can move their virtual impaired limbs using their healthy hands, meaning simulated physical movements are survivor-authored. Virtual visuomotor feedback may help regain functional connectivity between the brain and the impaired limb, therefore also regaining voluntary control of the limb.
The aim of the study was to test if the shoulder, elbow, and wrist movement; hand pinch strength; and grip strength of the paretic side improved through the use of VAI exclusively or combined with P/OT for upper extremities and how these approaches improved functional outcomes measured by the Action Reach Arm Test [20]. The relationship between changes in abilities to control upper extremities and volumetric changes in cortex grey matter measured by VBM and using MRI was also explored.[…]
Continue —-> https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-020-00754-7