Archive for November, 2021
[ARTICLE] Home-based self-help telerehabilitation of the upper limb assisted by an electromyography-driven wrist/hand exoneuromusculoskeleton after stroke – Full Text
Posted by Kostas Pantremenos in Paretic Hand, REHABILITATION, Rehabilitation robotics, Tele/Home Rehabilitation on November 29, 2021
Abstract
Background
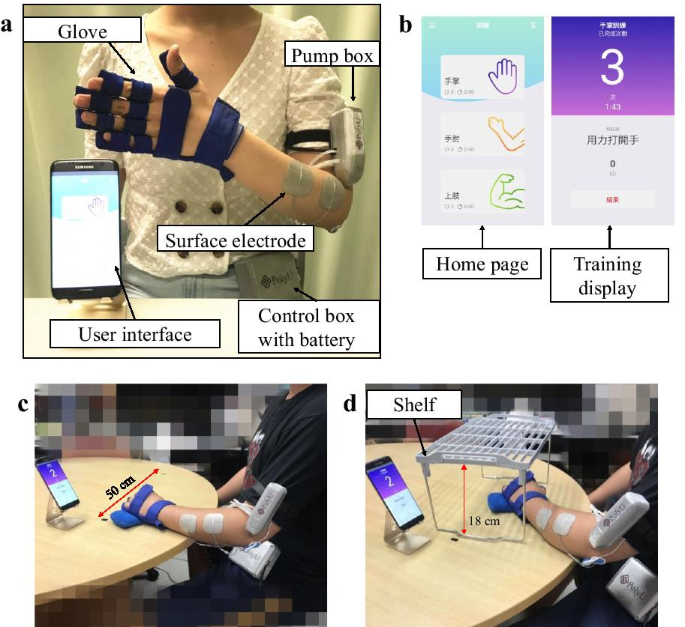
Most stroke survivors have sustained upper limb impairment in their distal joints. An electromyography (EMG)-driven wrist/hand exoneuromusculoskeleton (WH-ENMS) was developed previously. The present study investigated the feasibility of a home-based self-help telerehabilitation program assisted by the aforementioned EMG-driven WH-ENMS and its rehabilitation effects after stroke.
Methods
Persons with chronic stroke (n = 11) were recruited in a single-group trial. The training progress, including the training frequency and duration, was telemonitored. The clinical outcomes were evaluated using the Fugl–Meyer Assessment (FMA), Action Research Arm Test (ARAT), Wolf Motor Function Test (WMFT), Motor Functional Independence Measure (FIM), and Modified Ashworth Scale (MAS). Improvement in muscle coordination was investigated in terms of the EMG activation level and the Co-contraction Index (CI) of the target muscles, including the abductor pollicis brevis (APB), flexor carpi radialis-flexor digitorum (FCR-FD), extensor carpi ulnaris-extensor digitorum (ECU-ED), biceps brachii (BIC), and triceps brachii (TRI). The movement smoothness and compensatory trunk movement were evaluated in terms of the following two kinematic parameters: number of movement units (NMUs) and maximal trunk displacement (MTD). The above evaluations were conducted before and after the training.
Results
All of the participants completed the home-based program with an intensity of 63.0 ± 1.90 (mean ± SD) min/session and 3.73 ± 0.75 (mean ± SD) sessions/week. After the training, motor improvements in the entire upper limb were found, as indicated by the significant improvements (P < 0.05) in the FMA, ARAT, WMFT, and MAS; significant decreases (P < 0.05) in the EMG activation levels of the APB and FCR-FD; significant decreases (P < 0.05) in the CI of the ECU–ED/FCR–FD, ECU–ED/BIC, FCR–FD/APB, FCR–FD/BIC, FCR–FD/TRI, APB/BIC and BIC/TRI muscle pairs; and significant reductions (P < 0.05) in the NMUs and MTD.
Conclusions
The results suggested that the home-based self-help telerehabilitation program assisted by EMG-driven WH-ENMS is feasible and effective for improving the motor function of the paretic upper limb after stroke.
Introduction
Most patients with stroke who are discharged home from inpatient poststroke rehabilitation have residual motor impairment of the upper limb, especially in the distal joints (i.e., the wrist and the fingers), which greatly inhibits their ability to perform activities of daily living (ADLs) [1, 2]. Although the traditional viewpoint on poststroke rehabilitation suggested that significant motor recovery mainly occurs in the first 6 months after the onset of a stroke (i.e., acute and subacute periods) [3], more recent studies have indicated that significant motor improvements could also be achieved in the chronic period after stroke through physical training as long as such training is as intensive as the one provided to inpatients [4, 5]. Continuous and regular physical therapy is required to improve the wrist/hand function of outpatients with chronic stroke [6]. The restoration of limb function after stroke depends on intensive and repetitive training of the paralyzed limb [7, 8] with maximized voluntary motor effort [9, 10] and minimized compensatory motions in close-to-normal muscular coordination [10, 11]. However, the provision of effective wrist/hand rehabilitation services for outpatients with chronic stroke is insufficient in the current healthcare system in the world.
In most cases, outpatients have limited access to wrist/hand treatments with the necessary training intensity [12, 13] because of resource constraints due to factors such as an expanding stroke population and a lack of professionals worldwide [14, 15], as well as other difficulties such as commuting [2] to the outpatient services in day hospitals, and the restriction of social distancing during the COVID-19 pandemic. Home-based telerehabilitation with minimum assistance and remote supervision by professionals (i.e., self-help operation) is a promising approach for sustaining of physical treatment after discharge and enhancing the accessibility of rehabilitation resources to improve the wrist/hand motor functions of discharged patients [16,17,18].
However, few studies have focused on techniques for effective self-help upper limb rehabilitation, especially for distal joints [16]. Currently, most studies on home-based telerehabilitation have been based on virtual reality (VR) techniques because home-based VR training is more convenient for and accessible to outpatients than conventional therapy in a clinic or day hospital [16, 19]. Nevertheless, those systems focus on assessment or monitoring of limb performance rather than providing the necessary physical assistance for the patients to achieve the desired movements [16, 20,21,22,23,24]. Rehabilitation robots have been developed to provide mechanical assistance that mimics physical support from a therapist in conventional therapy; these robots can alleviate the labor-intensive aspects of hands-on physical therapy by performing repetitive therapeutic tasks intensively under the supervision of a therapist [15], and these robotic therapies for distal joints have been reported to be effective for improving upper limb motor function [1, 25]. However, the majority of the existing rehabilitation robots are heavy, have complex mechanical designs, and require large power supplies, large physical spaces in conventional environments (e.g., clinic), and close professional supervision, which are significant deterrents to their use by patients independently at home [15, 26].
Furthermore, using robot alone has a limitation in directly activating the desired muscle groups because the target muscles of patients with stroke usually cooperate with compensatory motions from other muscular activities [27]. Compensatory motions from the trunk and the proximal joints, i.e., abnormal motor synergies, are commonly observed in most persons with chronic stroke when they attempt to reach an object or orient their hand to grasp an object [28]. When neuromuscular electrical stimulation (NMES) combined with robotic therapy, the robotic assistance could provide sensorimotor experiences with precise kinematics to realize the desired movements [29], and NMES could activate the target muscles and reduce compensation from alternative muscle synergies [30]. Thus, the combined NMES-robot treatment has been suggested to facilitate close-to-normal muscular coordination with reduced compensation motions, and it has yielded more effective rehabilitation outcomes than upper limb rehabilitation treatments that use only NMES or only robots [31]. Electromyography (EMG) of the paralyzed limb to indicate voluntary intention to integrate voluntary motor effort during practice has been recommended for optimizing therapeutic outcomes [32]. EMG-driven training systems have yielded superior improvements in motor functions with longer sustainability than those with passive limb motions [33], especially for voluntary motor control of the upper limb. Therefore, EMG-driven NMES-robot therapy for home-based self-help training is desirable for effective wrist/hand rehabilitation for outpatients with chronic stroke.
A novel EMG-driven exoneuromusculoskeleton (ENMS) for self-help upper limb rehabilitation after stroke was developed recently by our team [34, 35]. Taking the advantages of exoskeleton, pneumatic muscle, and NMES, the developed system is lightweight, compact, and has low power consumption. The system can assist the extension and flexion of the elbow, wrist, and finger joints under voluntary effort control through EMG. The system consists of an elbow module and a wrist/hand module that can work collectively or separately. The wrist/hand module can work independently as an EMG-driven wrist/hand ENMS (WH-ENMS) to assist wrist/hand movements during training (Fig. 1). The rehabilitation effects of the EMG-driven ENMS have been investigated in 15 participants with chronic stroke [35], followed by a 20-session training program in a neurorehabilitation laboratory, where the participants completed the training independently with the system after they received a tutorial session and three guided training sessions (including practicing device operation and training setup). The participants exhibited significant improvements in voluntary motor control and muscle coordination of the paretic limb after the EMG-driven ENMS-assisted upper limb training [35]. No safety problems were reported by either the experiment operators or the participants throughout the study period. The system offers the possibility of home-based self-help wrist/hand training for discharged patients with chronic stroke. However, the feasibility of using the EMG-driven WH-ENMS for self-help upper limb training and its rehabilitation effects in a home setting had not been investigated.
[BLOG POST] Futuristic remote tech is empowering a “revolution” in stroke rehab at home
Posted by Kostas Pantremenos in Assistive Technology, REHABILITATION, Tele/Home Rehabilitation, Video Games/Exergames, Virtual reality rehabilitation on November 29, 2021

Thanks to a “technological revolution” in stroke rehabilitation, stroke recoveries could now take a smoother path, with a new interactive health system from Evolv offering telemonitored rehabilitation sessions in stroke survivors’ homes.
Designed with Microsoft’s Azure Kinect camera at its centre, the compact Evolv RehabKit can monitor a user’s precise movements, keeping a close eye on them as they take part in a series of task-based games and exercises. These form part of EvolvRehab, a pioneering virtual rehabilitation platform that runs on the RehabKit.
The therapeutic game-like activities in EvolvRehab have been designed by professional therapists to bolster stroke and brain injury survivors’ self-confidence while increasing their mobility, assisting in their ongoing progression to stand, reach, grasp, walk and speak.Advertisement | Continue story below
Having already seen “life-changing” results in its initial phases, Evolv RehabKit could become even more transformational, according to Microsoft.
Traditional stroke rehabilitation methods are centred around patients having face-to-face sessions in hospitals and specialist centres, which can last for months and sometimes years.
In contrast, the Evolv RehabKit can be used independently at home, with sessions replicating approved exercises, personalised by professional therapists for each survivor. This frees up clinicians’ time and improves patient outcomes through engaging games while easing pressure off the NHS.
David Fried, CEO of Evolv, said: “Our goal was to help deliver rehabilitation out of the clinical setting, providing the repetitive therapeutic activity that’s required to improve outcomes for stroke survivors directly into their homes ideally, or it could be in a day centre, community centre, or residential care home. It can help take the burden off the NHS sites.
“Microsoft is a really big part of that.”
The Evolv RehabKit has also been used to benefit others needing physical rehabilitation, such as those with Parkinson’s, multiple sclerosis, spine and brain injuries, or those who are at risk of falls.
Running from a mini-PC, EvolvRehab is powered by a suite of Microsoft technology, chiefly Azure Kinect, which captures the movement of the user. It also comes with Microsoft Teams, meaning patients and their therapists can communicate via video calls to set goals, share progress and provide feedback.
All the data gathered is stored in the Microsoft Azure cloud. Information and performance results can only be accessed by the user’s authorised physiotherapist. Healthcare professionals can also use Power BI to visualise patient performance and create user reports.
David further highlighted how the Evolv RehabKit offers a service that can’t be replicated elsewhere.
He added: “You need to treat stroke survivors like elite athletes, the same concept, training every day, a healthy lifestyle, positivity and repetition over and over again to improve performance. But you can’t have hundreds of them showing up to an NHS Trust and doing 1000s of repetitions of exercises in a rehabilitation ward.”
The rehabilitation technology has proved particularly helpful during the COVID-19 pandemic, where lockdown restrictions made it impossible for many therapists and stroke patients to meet in person.
In September 2020, Microsoft helped Evolv as it made more RehabKits available to healthcare teams. These were given to stroke survivors, allowing their vital progress to continue at home.
“What we try to do in our platform is offer different types of activities that touch upon different types of therapy. The important thing is the activities can be personalised to each individual at home,” David continued.
“For example, you’d be playing a game where barriers come out towards you, and you have to lift your leg to get over them, which helps balance and coordination. They are games, you are doing repetition, you are doing therapeutic activity that’s prescribed and personalised to you, but you have no idea you are doing exercise – you are simply playing a game.”
Evolv works closely with the specialist National Hospital for Neurology and Neurosurgery in Queen Square, London, which is part of University College London Hospitals NHS Foundation Trust. It has also partnered with academic institutions such as the universities of Reading, East Anglia and Cambridge, as well as collaborating with private physiotherapy providers.
While its physical challenges offer upper and lower extremity training, and fine motor skills for the hand, EvolvRehab also contains dual-tasking ‘exergames’ (exercise while playing gaming). These combine language and motor training to encourage thinking and moving simultaneously.
For example, a word is displayed on-screen along with several pictures of different items, and the “player” must reach out and touch the correct picture of the item based on the given word. At other times, they will touch the item that rhymes with a given word or starts with a certain sound.
It is through gamifying physiotherapy with points and trophies that the EvolvRehab software ensures survivors want to continue treatment, according to Microsoft.
Evolv is part of the Microsoft for Startups and Global Social Entrepreneurship programme, a global programme that offers new companies access to technology and go-to-market and community benefits to help them grow.
EvolvRehab is currently available in 10 different languages, with clinical validation in seven countries, and has been used to provide telerehabilitation in a dozen countries.
[BLOG POST] Holiday Struggles – Overcoming a Traumatic Brain Injury (TBI)
Posted by Kostas Pantremenos in Caregivers, TBI on November 29, 2021
by toliverio@90
Since the holidays are coming up, I figured I would talk about the struggles individuals with TBI deal with. I don’t know about you but overtime it has gotten better for me around the holidays.

The number one thing I have dealt with is overstimulation. It’s great seeing family I don’t get to see often. At the same time, I would struggle because of dealing with loud noises. The noises would be bouncing off the walls and amplified. When I hear constant sound like that, it would make me very overwhelmed. It would make my anxiety bad and send me into having a pain attack. I have learned over time on how to cope with this so I can enjoy the moment.

Depending on where I am, I will go into a quiet room to relax. There wasn’t an exact time of how long I needed quiet time. When I was done, relaxing my family has learned to not give me any attention towards what I just did. For me with people wondering why I did what I did makes my brain get overwhelmed.
Overtime, I have learned to take a break once and awhile in a quiet room. I do that even if I don’t feel overstimulated. In doing that, it helps prepare me for anything that could overwhelm me.
Another thing that I like to do is to take naps when I can. When an individual has a TBI, they are going to become exhausted because of the constant stimulation. It’s going to be harder for me to take naps this year because of my daughter. When she takes a nap, I am going to take a nap myself lol.

Tips on individuals with TBI’s or concussions surviving the holidays: https://youtu.be/Vj4gSikYZpA
When you get overwhelmed on the holidays, remember to use all your positive coping skills. You will get through the day the best you can. For individuals that don’t have anyone on the holidays, my heart goes out to you! Try to think of what you do have! God kept you around for a reason! Always remember to NEVER GIVE UP and you are a BADASS!!

Disclaimer:
I created a blog to talk about my story of my recovery and the daily struggles I deal with. I am a recreational therapist on top of having a TBI. Since I am able to see the side of a therapist and client/patient, it allows me to understand what individuals are really going through. I educate only on my symptoms that I deal with on a daily basis. I am not saying you need to do these things and that I am right. I am right for when it comes to talking about what I go through on a daily basis only. I just want you to know I empathize what you are going through. I have been through hell myself!
[Slideshow] How ADHD Affects Your Relationship – WebMD
Posted by Kostas Pantremenos in Caregivers on November 28, 2021
Your ADHD Relationship Survival Guide
Medically Reviewed by Smitha Bhandari, MD

You, Me, and ADHD
1/16
Attention deficit hyperactivity disorder can send your most important relationship off the rails. Distraction, procrastination, and other ADHD symptoms can stir anger, frustration, and hurt feelings for both the person with ADHD and the partner. But your marriage or relationship can thrive with proper treatment and tactics to ward off misunderstandings.

Distraction
2/16
This is the main symptom of ADHD. Your ADHD partner doesn’t seem to listen when you talk or fails to follow through on promises. You feel unheard, ignored, and unwanted. In reality, they may love you very much but are too distracted by the TV, the phone, or their own thoughts to show it.

Distraction Strategies
3/16
First, calmly tell your ADHD partner how you feel. Bottled-up feelings can lead to resentment and anger. If conversations are a big problem, set a time to talk to your partner face-to-face, away from distractions. It may help to touch your partner while you talk. If you’re the one with ADHD and start to zone out, fess up. Ask your partner to repeat what they said. If the conversation goes on too long and your mind wanders, it’s harder to reconnect.

Hyperfocus
4/16
This is the flip side of distraction. You may be so engrossed in something it’s hard to shift your attention away. You can’t drag yourself away from that new best seller or look up from your smartphone. Hyperfocus can be a gift for productivity. But unchecked, it can make your loved one feel less important than whatever has grabbed your attention.

Hyperfocus Strategies
5/16
If you’re prone to hyperfocus during certain activities, like online games or crossword puzzles, avoid them close to mealtimes or whenever you need to engage with your partner. Set alarms and track the time you spend on doing one thing. Get up or move to break your preoccupation when you realize you’re hyperfocusing. If you’re the partner or the spouse, try not to take it personally.

Forgetfulness
6/16
You blanked out on your dinner date and left your husband stranded at the restaurant. Maybe your power got shut off because you forgot to pay your electric bill. Your partner feels they can’t trust you with even basic tasks. You feel like a failure. Anger builds on both sides.

Forgetfulness Strategies
7/16
Forgetfulness and other ADHD symptoms aren’t character flaws. Avoid lectures and don’t label the behavior as rude or uncaring. Don’t take over for your partner, either. That can leave you both resentful. Instead, work with your partner to help them remember. Use a day planner or reminders on a smartphone or a laptop.

Disorganization
8/16
The partner with ADHD may skip chores or leave jobs unfinished. Or constantly misplace the car keys or lose important papers. Disorganization can cause stress and wasted time and money. It also can lead to nagging and leave the other person feeling controlled.

Disorganization Strategies
9/16
Calm down and talk about the issues. Then look for fixes. Maybe the partner with ADHD can take charge of cooking and laundry instead of paying bills or organizing carpools. Play to each of your strengths to avoid the chore wars. Respect the ADHD partner’s need to keep items in certain spots — it may be their way of staying organized.

Impulsivity
10/16
People who have the hyperactive type of ADHD also tend to be impulsive. They often act before thinking. One common problem is impulsive spending. You may blow money on things you don’t need or max out the credit cards. Some people may have risky sex or drive dangerously. Or they may blurt out inappropriate comments at parties.

Impulsivity Strategies
11/16
Self-control can be learned. You can help your partner role-play how to act in social situations. Or how to wait their turn. If you’re apt to overspend, bring cash and stick to your shopping list. Cut out temptations. Toss catalogues and unsubscribe from retailers’ emails. If impulsive behaviors are out of hand, you may need help from a therapist with expertise in ADHD.

Procrastination
12/16
We all put off boring or hard tasks from time to time. But for some people with ADHD, procrastination is a giant hurdle. You might not know how to get started, or feel overwhelmed by a project. You may need last-minute deadlines as motivation. That’s a recipe for a chaotic lifestyle that’s hard on you and your partner.

Procrastination Strategies
13/16
It’s easier to tackle a project when you break it into small chunks. Focus on only the first part — don’t think about the rest of it until you finish step one. If you’re the partner, see if you can share a part of the task to offer company. But take care not to take over their responsibility. Most importantly, don’t think of procrastination as a personal defect, but as a trait that can be managed.

Mood Swings
14/16
People with ADHD often have trouble controlling emotions. You might lash out in anger or have sudden or wide mood swings. That’s because you feel anxiety and frustration — as well as joy and happiness — more intensely than some others. That can leave your partner on edge.

Mood Swing Strategies
15/16
A healthy diet, good sleep, and regular exercise can head off mood swings. Yoga or tai chi can ease stress and help you control your impulses. If you’re the partner, don’t overreact to flare-ups. Instead, empathize but also explain how they affect you. Go on a hike or do something together.
[WEB] Transcutaneous Auricular Vagus Nerve Stimulation
Posted by Kostas Pantremenos in REHABILITATION on November 28, 2021
Recently, a noninvasive form of VNS known as transcutaneous auricular vagus nerve stimulation (taVNS) has emerged (George 2000). Unlike surgically-implanted VNS, taVNS is an inexpensive, low-risk, easy to administer, and portable option to modulate the vagus system. taVNS is appealing as it allows for rapid translation of basic VNS research in exploring potential treatments of central and peripheral disease.
Vagus nerve stimulation (VNS) involves surgical implantation of electrodes onto the cervical branch of the vagus nerve. Electrical pulses are delivered to the vagus nerve via an implanted pulse generator (IPG) surgically implanted in the chest. VNS is currently FDA-approved for epilepsy, refractory depression, and chronic obesity and long-term safety of VNS is well established.
taVNS on the other hand, delivers electrical stimulation to the auricular branch of the vagus nerve (ABVN), an easily accessible target that innervates the human ear (Peukar and Filler 2002). Over the last decade, several groups have demonstrated the safety and tolerability of this method, including central and peripheral nervous system effects, and behavioral effects in neuropsychiatric populations (Kreuzer et al 2012, Clancy et al 2014, Rong et al 2016, Bauer et al 2016 ). taVNS is also being explored in individuals to enhance cognitive and social functioning (Jacobs et al 2015,Jongkees et al 2018,Colzato et al 2018). Furthermore, side-effects of taVNS are minimal, with skin irritation or redness being the most common side-effect.

The optimal stimulation targets are still being explored (Badran et al 2018), however, the two most common placements are the anterior wall of the outer ear canal (tragus) and the cymba conchae. Sham stimulation may be conducted by stimulating the earlobe of the ear, an area believed to have minimal ABVN innervation. Alternatively, sham may be delivered via a passive control method in which electrodes are attached to active sites, but no stimulation is delivered. Stimulation parameters used have varied between groups, however according to the literature, stimulation is delivered in a pulsatile fashion (pulse width: 250–500 μs, frequency: 10–25 Hz) and delivered at an individualized constant current (< 5 mA).
taVNS Stimulator by Soterix Medical

Based on the revolutionary mini-CT platform, Soterix Medical introduces the first transcutaneous auricular vagus nerve stimulator (taVNS) specially developed for clinical (human) brain stimulation research. The system provides the necessary pulse parameter settings (frequency, train duration, inter-train interval, session duration) that allow testing commonly used protocols. With option to unlock device in as many as three different ways (code-based , time-based, ElectraRx web-based), the system provides researchers with flexibility to plan taVNS trials as they wish.
taVNS Accessories
The Soterix Medical taVNS ear stimulation electrodes are the first and only electrodes optimized specifically for rigorous human trials.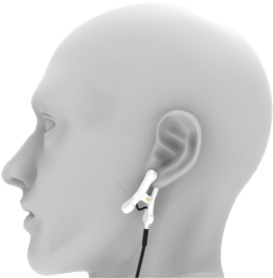
Easy-Clip
The Soterix Medical EASY-Clip electrode is designed for ease-of-use and flexible application. The optimal spring mechanism has been validated to ensure a comfortable and robust contact whether targeting the auditory canal (tragus) or the ear lobe for SHAM stimulation
.
RELIfit-Tragus
The Soterix Medical RELIfit-Tragus solution is uniquely designed to hook around the ear for fail safe positioning in real-world applications, The simple and convenient design offers the option for either short duration (saline sprayed sponge) or extended duration (gel) applications.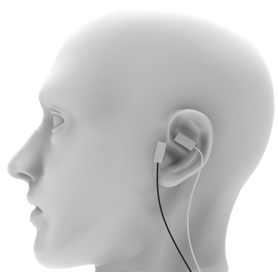
RELI-Stick
The Soterix Medical RELI-Stick electrode offers unmatched versatility. These single use flexible hydrogel electrodes with optimal adhesion performance can be positioned anywhere on the ear for ultimate customization and subject comfort.
References
- George, M.S. et al. Vagus nerve stimulation: a new form of therapeutic Brain Stimulation.CNS Spectrums. 5 (11), 43-52 (2000).
- Peuker, E.T., & Filler, T.J. The nerve supply of the human auricle. Clinical Anatomy. 15 (1), 35-37 (2002).
- Kreuzer, P.M. et al. Transcutaneous vagus nerve stimulation: retrospective assessment of cardiac safety in a pilot study. Frontiers in Psychiatry. 3, 70 (2012)
- Clancy, J.A. et al. Non-invasive vagus nerve stimulation in healthy humans reduces sympathetic nerve activity. Brain Stimulation. 7 (6), 871-877 (2014).
- Bauer, S. et al. Transcutaneous vagus nerve stimulation (tVNS) for treatment of drug-resistant epilepsy: a randomized, double-blind clinical trial (cMPsE02). Brain Stimulation. 9 (3), 356-363 (2016).
- Jacobs, H.I., Riphagen, J.M., Razat, C.M., Wiese, S., & Sack, A.T. Transcutaneous vagus nerve stimulation boosts associative memory in older individuals. Neurobiology of Aging. 36 (5), 1860-1867 (2015)
- Jongkees, B.J., Immink, M.A., Finisguerra, A., & Colzato, L.S. Transcutaneous Vagus Nerve Stimulation (tVNS) Enhances Response Selection During Sequential Action. Frontiers in Psychology. 9, 1159 (2018).
- Colzato, L.S., Ritter, S.M., & Steenbergen, L. Transcutaneous vagus nerve stimulation (tVNS) enhances divergent thinking. Neuropsychologia. 111, 72-76 (2018).
- Badran, B.W. et al. Tragus or cymba conchae? Investigating the anatomical foundation of transcutaneous auricular vagus nerve stimulation (taVNS). Brain Stimulation. 11 (4), 947-948 (2018).
[VIDEO] Recovery from Brain Injury Occurs for the Rest of a Person’s Life
Posted by Kostas Pantremenos in Recovery Plateau, REHABILITATION, TBI, Video on November 27, 2021
The human brain is a wonderful organ with amazing flexibility. Dr. Dave Hovda advocates for those who have had traumatic brain injuries and discusses the process of recovery.
Check out more BrainLine content at: https://www.brainline.org/
Explore our other channels!
Reading Rockets – https://www.youtube.com/user/wetalear…
Colorin Colorado – https://www.youtube.com/user/colorinc…
[Abstract] MIDAS: Multi-sensorial Immersive Dynamic Autonomous System Improves Motivation of Stroke Affected Patients for Hand Rehabilitation – Full Text PDF
Posted by Kostas Pantremenos in Paretic Hand, Rehabilitation robotics, Video Games/Exergames, Virtual reality rehabilitation on November 27, 2021

In this paper, we present the design and development of MIDAS. MIDAS is intended to be a portable immersive system inclusive of an exoskeleton, a smell releasing device, and a VR game that will help stroke patients feel more motivated during a hand rehabilitation session. MIDAS engages four out of five senses during rehabilitation. MIDAS uses EMG signals taken from the subject’s forearm to predict their intention before activating physical assistance (tactile) in the opening or closing of the fingers of their hand. To evaluate the performance of MIDAS, a pilot study is done using established tools to quantify the user experience, comfort, pleasure, and motivation of the subjects in using MIDAS for rehabilitation exercises.
PDF file Download (1005.78 kB)
[Abstract] A Hybrid Arm-hand Rehabilitation Robot with EMG-based Admittance Controller
Posted by Kostas Pantremenos in Paretic Hand, Rehabilitation robotics on November 27, 2021
Abstract
Reach-and-grasp is one of the most fundamental activities in daily life, while few rehabilitation robots provide integrated and active training of the arm and hand for patients after stroke to improve their mobility. In this study, a novel hybrid arm-hand rehabilitation robot (HAHRR) was built for the reach-and-grasp task. This hybrid structure consisted of a cable-driven module for three-dimensional arm motion and an exoskeleton for hand motion, which enabled assistance of the arm and hand simultaneously. To implement active compliance control, an EMG-based admittance controller was applied to the HAHRR. Experimental results showed that the HAHRR with the EMG-based admittance controller could not only assist the subject in fulfilling the reach-and-grasp task, but also generate smoother trajectories compared with the force-sensing-based admittance controller. These findings also suggested that the proposed approach might be applicable to post-stroke arm-hand rehabilitation training.
[ARTICLE] The Effect of a Full Upper-Limb Control System and Its Usage in Stroke Rehabilitation – Full Text
Posted by Kostas Pantremenos in REHABILITATION, Virtual reality rehabilitation on November 25, 2021
Abstract
Backgrounds: Transferring behaviors of a human’s upper-limbs to an avatar is widely used in the field of virtual reality rehabilitation. To realize the transfer, movement tracking technology is required. Traditionally, wearable tracking devices are used to do the tracking, however the devices are expensive and cumbersome. Recently, non-wearable upper-limb tracking solutions are proposed, which are cheaper and more comfortable to interact. But most of the existing products cannot track full upper-limbs including both the arms and all the fingers, which limits the motion paradigm and further may lead to limited rehabilitation effect.
Methods: In this paper, a novel method was first proposed for full avatar’s upper-limb control which integrates the fine finger motion and the arm wide range motion. Then, based on the method, a Virtual Reality Rehabilitation System (VRRS) was developed for upper-limb rehabilitation. To test the performance of VRRS, two experiments were designed. First, in order to investigate the effect of VRRS on virtual body ownership, agency, location of the body and usability, we compared it with the partial upper-limb tracking method based on Leap Motion controller (LP) in same virtual environments. Then, to study the feasibility of VRRS in rehabilitation, we recruited 16 stroke patients and split them into two groups: the experimental group and the control group. Each group consisted 8 patients, with and without employing VRRS respectively.
Results: The control of full avatar’s upper-limbs improved the users’ senses on body ownership, agency and location of the body. The users preferred to use VRRS. In addition, although the upper-limb motor function of patients from both groups were improved, the difference between the FM scores tested on the first day and the last day of the experimental group was more significant than that of the control group.
Conclusions: VRRS based on the proposed method for full avatar’s upper-limbs control was developed, which improved the user experience on embodiment and effectively improved the rehabilitation effect for upper-limbs of stroke patients.
Introduction
Stroke is common in all kinds of people, the consequence is obvious muscle weakness on one side of the body [1]. It is estimated that 50–75% of patients suffering stroke have persistent impairment of the affected upper limb and they need to do boring repeated physical training to recover their motor function [2]. To provide a more enjoyable and personalized experience on motor rehabilitation, the usage of virtual environment is gradually popular in the field for its richness and interesting [3]. The virtual nature of the environment allows the behaviors that cannot be realized or highly costed in reality to be implemented in a low-cost way. Previous works indicate that the strength and activity ability of the affected side of body can be effectively restored by controlling the avatar’s upper-limbs to interact with objects in a virtual environment. Triandafilou et al. [4] developed a 3D, networked multi-user Virtual Environment for Rehabilitative, Gaming Exercises (VERGE) system, for home therapy with a low-cost Kinect device. Cuesta-Gómez et al. [5] used an LMC system and serious games for upper limb rehabilitation. Besides, Sucar et al. [6] introduced a virtual reality-based platform for rehabilitation of the upper-limbs with gesture therapy.
In many applications and studies of virtual reality, avatars are used as the medium of people interacting with the virtual environment [28]. Movement tracking is one of the key technologies for avatar control [29]. For partial upper-limb tracking, consumer devices including hand-held controllers such as Oculus Touch or HTC VIVE controllers and Motion Sensing devices such as Kinect and Leap Motion controller are widely used [27]. Granqvist et al. [12] used HTC VIVE controllers with inverse kinematics for partial upper-limb tracking. However, the hand-held controller can only track the position of the hand and cannot give the position information of the fingers. Collingwoode-Williams et al. [11] built a system to study the effect of lip and arm synchronization on the feeling of body ownership. They used a Kinect device for body tracking and an Oculus Rift for head rotation measuring. But the Kinect device can only track arms and part of finger joints. It is proved that complete upper-limb tracking enhances the realism of avatar’s upper-limb behavior which influences patients’ cognition and motor recovery. Generally, in order to have a high-quality full upper-limb tracking, the user need to use marker-based tracking systems that require them to wear tracking suits such as with the OptiTrack system [7][8]. The suits are expensive and cumbersome. Usage of consumer devices is another solution which is cheaper. Lin et al. [10] used the Oculus Rift headset with a Kinect sensor, a Leap Motion controller and a dance pad to navigate and manipulate objects inside synthetic scenes. In the method, only one Kinect was used and cannot recognize which side of the body is facing the device. Wu et al. [9] introduced a set-up which integrates multiple Kinects for robust and accurate full-body 3D skeleton tracking and a Leap Motion controller for hands. However, the tracking area of the Leap Motion controller was limited to a small range above the device.
In this paper, a low-cost method was proposed which can fully control avatar’s upper-limbs by tracking movements of both arms and all fingers in large tracking area. We also developed a Virtual Reality Rehabilitation System (VRRS) based on this method. In the virtual environment of VRRS, movement of the user’s upper-limbs is mapped to an avatar’s upper-limbs to improve the sense of engagement with the virtual environment. In order to dynamically match the motor function of patients, the difficulty of tasks can be modified conveniently, which is important for motor learning in general [13] and rehabilitation in particular [14].
We first performed a preliminary experiment to compare VRRS with the partial tracking method based on the Leap Motion controller [30]. In the experiment, we built a virtual environment customized for upper-limb motion, and measured the senses of body ownership, agency, location of the body and the usability of the systems. Then, in order to evaluate the feasibility of VRRS in rehabilitation training, another experiment is performed. In the experiment, 16 stroke patients are recruited and the Fugl-Meyer (FMA) of the patients’ upper-limb motor functions are evaluated.
The hypothesis was that VRRS can elicit higher senses on body ownership, agency and location of the body and users were satisfied with VRRS. We also expected VRRS to enrich motion paradigm and thereby be more effective in rehabilitation training to help stroke patients recover their upper-limb motor function.[…]

[ARTICLE] Motor-cognitive intervention concepts can improve gait in chronic stroke, but their effect on cognitive functions is unclear: A systematic review with meta-analyses – Full Text
Posted by Kostas Pantremenos in Cognitive Rehabilitation, Gait Rehabilitation - Foot Drop on November 25, 2021
Highlights
• Motor-cognitive intervention concepts should be classified as sequential or simultaneous and as competing or incorporated.
• Motor-cognitive trainings are superior to single physical training in improving gait speed and walking endurance in chronic stroke.
• Of different motor-cognitive intervention concepts, simultaneous-incorporated exergames seem to be the most promising type for improving gait speed and potentially other functions.
• Whether motor-cognitive trainings can improve cognitive functions in chronic stroke remains unclear, thus future studies are warranted.
Abstract
Motor-cognitive intervention concepts are promising to counteract residual gait and cognitive impairments in chronic stroke. There is, however, considerable variation in motor-cognitive intervention types, which may lead to different effects. This systematic review strived to summarize and compare the effects of different motor-cognitive intervention concepts on gait and cognitive functions in chronic stroke. The systematic search identified twenty-nine articles, which were allocated to three types of motor-cognitive training concepts; SEQUENTIAL, SIMULTANEOUS-ADDITIONAL, and SIMULTANEOUS-INCORPORATED. Random-effects meta-analyses revealed that motor-cognitive interventions may be better than non-combined training approaches for improving gait function in chronic stroke (e.g. gait speed: g = 0.43, 95 % CI [0.22, 0.64], p < 0.0001). SIMULTANEOUS-INCORPORATED motor-cognitive training seems the most promising concept. As very few articles measured both, spatiotemporal gait parameters and cognitive outcomes, future studies are warranted to investigate the effects of motor-cognitive intervention concepts on gait control and cognitive functions in chronic stroke.
1. Introduction
Stroke is a major cause for long-term disability worldwide (Benjamin et al., 2019; Feigin et al., 2017). While only a fourth of stroke survivors fully regain pre-stroke levels of participation and functioning in daily life (Lai et al., 2002; Mayo et al., 2002), approximately half of them stay moderately to severely impaired (FragileSuisse, 2021). Moreover, four-fifths of stroke survivors have been reported to not feeling completely recovered from the incident within four years (Gadidi et al., 2011). Accordingly, stroke survivors are often disappointed with professional services because they feel rehabilitation programs end too abruptly and are not specific enough to substantially improve the perceived quality of life (Robison et al., 2009).
Stroke survivors may face a broad range of impairments affecting their motor and cognitive abilities (Jorgensen et al., 2010; Maaijwee et al., 2014; Sun et al., 2014; Tang et al., 2018). A majority of stroke survivors suffer from hemiparesis, a one-sided weakness of one or both extremities, which results in loss of motor function (Langhorne et al., 2009; Sheffler and Chae, 2015). Hemiparetic gait is characterized by asymmetries and changes in spatiotemporal parameters, resulting in reduced gait speed and increased energy costs for walking (Balaban and Tok, 2014; Patterson et al., 2010; Sheffler and Chae, 2015). Furthermore, cognitive impairments may persist after the sub-acute phase of stroke, including deficits in attention, executive functions, visuo-spatial skills, and processing speed (Cumming et al., 2013; Tang et al., 2018). Formulating their top ten research priorities, stroke patients first named the need to improve cognition, followed by the need to address long-term consequences; the need to improve balance and gait is the seventh priority on this list (Pollock et al., 2012). In contrast to the priorities mentioned from the patients’ perspective, hardly any RCTs have focused on cognitive functions in stroke survivors, and effective treatments for memory and executive functions, for example, are largely lacking (Cumming et al., 2013).
Moreover, the first and seventh patients’ priority are closely related as many daily life activities simultaneously challenge walking and cognitive abilities. While healthy individuals cope well with simultaneous performance of motor and cognitive activities, people suffering from a neurological condition such as stroke struggle with it (Cockburn, 1998). Stroke has been linked to Motoric Cognitive Risk syndrome, where cognitive and gait impairments are intertwined (Allali et al., 2016), as post-stroke cognitive and gait impairments share structural and functional roots (Hamacher et al., 2015; Ursin et al., 2019; Verstraeten et al., 2016). Consequently, it can be hypothesised that interventions that focus on both motor and cognitive aspects within the same treatment are beneficial in chronic stroke. A promising approach are motor-cognitive training intervention concepts. These concepts are designed such that they require sequential or simultaneous performance of both motor and cognitive tasks (Herold et al., 2018; Levin et al., 2017). According to the “guided plasticity facilitation” model (Bamidis et al., 2014; Fissler et al., 2013), motor-cognitive intervention concepts should especially trigger neuroplasticity, a main goal of stroke rehabilitation (Maier et al., 2019; Pin-Barre and Laurin, 2015).
Various reviews and intervention studies have reported beneficial effects of motor-cognitive interventions on single- and dual-task walking, balance, and cognition in healthy or cognitively impaired older adults and neurological patients (N. E. Fritz et al., 2015; Lauenroth et al., 2016; Law et al., 2014; Levin et al., 2017; Raichlen et al., 2020; Zhu et al., 2016). In subacute stroke patients with vascular cognitive impairments, a motor-cognitive intervention has been found to improve various cognitive functions (Bo et al., 2019). Furthermore, studies with chronic stroke patients have found promising effects of motor-cognitive interventions on mobility, balance, gait speed and walking endurance as well as for reducing fall risk (An et al., 2014; Lee et al., 2017; Pang et al., 2018).
However, the effects of different motor-cognitive intervention concepts on gait and cognitive functions in chronic stroke have never been investigated systematically. Currently it is unclear whether motor-cognitive intervention concepts are more effective than single motor- and/or cognitive-training interventions. Furthermore, the variation in motor-cognitive interventions is considerable depending on the applied concept (Herold et al., 2018); as a result, different motor-cognitive intervention concepts could yield different results in chronic stroke. For this reason, this systematic review assesses how different types of motor-cognitive training intervention concepts affect gait and cognitive functions in chronic stroke. Our aim is to identify, summarize and contrast randomized controlled trials (RCTs), which evaluate motor-cognitive intervention concepts compared to single training interventions in chronic stroke regarding gait and cognitive functions.[…]

