Posts Tagged Self-Esteem
[BLOG POST] The Need to Please: The Psychology of People-Pleasing
Posted by Kostas Pantremenos in Cognitive Rehabilitation, Educational on August 14, 2021
In this article, you’ll learn about the psychology of people-pleasing: Why we do it and how to reduce people-pleasing and codependent behaviors.

Do you have a strong desire to please others?
When was the last time you told someone “No, I can’t help you with that” or “I have a different opinion”? It can feel risky – emotionally vulnerable – to set limits or assert our needs or opinions (especially if we know they are different than other people’s).
Of course, it’s normal to want to be liked and accepted, but for some of us, the need to please is so strong that we’ll sacrifice our identities, our needs, and our wants, in order to be accepted.
The root cause of people-pleasing and codependency
Our need to please is actually more of a need to belong. And our need to belong was probably written in our DNA millions of years ago.
In order to survive, prehistoric man had to form groups or tribes that offered protection from predators, pooled resources, and shared work. And if you weren’t accepted by the group, there was a high probability that you’d starve to death or get eaten by a saber tooth tiger.
Certainly, it’s much easier to live a solitary life in modern society, but it’s not very fulfilling. Most of us want to belong and form lasting bonds with other people.
And we find it very painful to be rejected or criticized by others. We fear being alone and that being alone means we’re inadequate or unlovable. So, we go to extreme lengths to please others – to avoid rejection or abandonment, to avoid being alone.
I was taught that it’s important to care about others and to be polite – and you probably were, too. What’s wrong with that? Isn’t this how we should be raising our children? Well, the short answer is Yes, of course! But like most things, the devil is in the details. It’s possible to overdo politeness and caretaking.
Sometimes we call this codependency – when the need to please gets out of control and we become self-sacrificing martyrs instead of well-balanced adults.
Codependency is essentially a coping strategy that we develop when living in a chaotic or dysfunctional family. Codependency can also be passed down through the generations.
In an effort to stay physically and emotionally safe, we tune in to other people’s feelings and issues. We try to keep the peace by being super compliant. And we can become perfectionistic as a way to get some positive attention or to avoid criticism and punishment.
Reflective Questions:
- What experiences molded you into a people-pleaser?
- What contributed to your fear of rejection, abandonment, conflict, or criticism?

You think too much about other people and not enough about yourself
Yes, we should think about other people. We should care about their feelings and needs. However, we shouldn’t only care about others and minimize or suppress our own feelings and needs.
You are just as important as everybody else. And yet, many of us behave like we matter very little, if at all. We care more about others than we do about ourselves. Again, this may sound like a value you learned as a child, but it’s not sustainable. You can’t remain a healthy, patient, kind, energetic, caring person if you constantly give but never replenish your needs.
We all have needs – and they matter
This brings us to another common problem: We don’t think we should have any needs or we act like we don’t need anything. We want to be easy-going, low-maintenance, and agreeable.
Agreeableness is a desirable quality, but it’s not realistic to think your needs, ideas, interest, and values will line up with other people’s all the time. Sometimes we will have conflicts with others and that’s okay. Healthy relationships can tolerate disagreements and resolve conflicts.
Everyone has needs. They range from the basics (food, water, clothing, shelter, sleep) to the more complex (belonging, connection, to be understood, physical affection, mental stimulation, spiritual enlightenment, and so forth). When we don’t meet our own needs (and ask others to help us meet our needs), we get depleted – physically exhausted and sick, irritable and resentful, discouraged or hopeless.
Reflective Questions:
- Which of your needs that frequently go unmet?
- How do you feel when you don’t practice self-care or don’t express your opinions and wants?
- Why do you undervalue your needs and ideas? What happens when you do this?

You assume others are judging or criticizing you
What goes through your head when you think about speaking your mind, asking for what you need, or setting a boundary?
Perhaps your inner voice sounds something like this:
Will they be angry?
They’re going to hate me.
I’m a terrible person.
I know they don’t like me.
They’re going to think I’m difficult.
What’s wrong with me?
These types of thoughts are assumptions – negative assumptions to be more accurate – and they contribute to people-pleasing behaviors.
Most of the time we don’t actually know what other people think of us. We may have some ideas given their behavior, but remember even our observations filter through our assumptions and negativity bias, so they aren’t completely accurate. Consider that your assumptions might be wrong; people may not think as negatively about you as you imagine.
Inevitably, some people won’t like you or agree with your choices or values. We can’t control what others think about us. All we can do is live authentically and try to feel good about who we are and what we do.
When you live according to your values and do things to meet your needs, you’ll feel good about your choices and you won’t need other people’s approval. On the other hand, if your actions don’t align with your values and needs, you’ll seek external approval to quiet our
Here’s an example: If I’m getting sick and tell my coworker that I can’t cover her shift tomorrow as planned, I probably won’t feel bad or guilty. I don’t need her approval because I know that I’m doing what’s right for me.
Reflective Questions:
- What prevents you from being assertive?
- How can you tolerate the pain of someone being angry at you or not liking you?
- How can you comfort yourself?
- What can you say to yourself to remind yourself that disagreeing is okay and meeting your own needs is healthy?
Overcome people-pleasing, codependency, and low self-esteem
As we work to overcome problematic people-pleasing, we need to find a balance between pleasing others (meeting their needs) and pleasing ourselves (meeting our own needs).
We can do this by:
- Recognizing that your needs matter as much as everyone else’s
- Noticing negative assumptions and challenging them (don’t assume that people think ill of you or that differing opinions won’t be accepted)
- Tolerating the discomfort of being criticized or not liked
- Nurturing or seeking relationships with people who accept you for who you are
- Getting to know yourself better (knowing what you like, what you need, what your goals are)
- Identifying your values
- Living authentically (in alignment with your beliefs and interests)
- Being assertive
- Setting boundaries without guilt (remembering that boundaries are kind and helpful)
- Accepting that not everyone will like you or be happy with you all the time
- Maintaining a give-and-take in relationships and limiting time with “takers” who don’t reciprocate
- Accepting that you can’t control what others’ think of you
Reflective Questions:
- How can you balance your needs and other people’s needs?
- How can you ask for what you need?
- How can you express your opinions and ideas more honestly?
- How will your health and relationships improve if you take better care of yourself?

Read more
[ARTICLE] Social Anxiety and Self-Esteem in Patients with Epilepsy – Full Text PDF
Posted by Kostas Pantremenos in Epilepsy on November 19, 2020
Abstract
Background: Epilepsy is the second most common and frequently encountered neurological condition that imposes a heavy burden on individuals, families, and also on healthcare systems. Epilepsy is a chronic disorder characterized by a spontaneous tendency to recurrent seizures which affects the patient’s cognitive, behavioral, psychological, and social functioning. Epileptic patients face various problems that result in lower self-esteem and fear about epileptic attacks in public places.
Objective: The aim of the present study is to measure social anxiety and self-esteem among patients with epilepsy and normal group.
Methods: The sample consisted of 100 patients with epilepsy and normal group (50 epilepsy and 50 normal group) selected from OPD of Central India Institute of Mental Health and Neuro Sciences (CIIMHANS) and near the village (Dewada&Kopidih) of CIIMHANS, Dewada, Rajnandgoan (Chhattisgarh) by using a purposive sampling method. Socio-demographic and clinical details of all the patients with epilepsy and the normal group were assessed by using the Liebowitz Social Anxiety Scale (LSAS) and Rosenberg Self-Esteem Scale (Rosenberg, M. 1965).
Results: Social anxiety and self-esteem scores were significant differences among patients with epilepsy and normal group. Higher social anxiety and lower self esteem in patients with epilepsy compared to normal groups.
Conclusion: Mental health profession should improve the self-esteem of patients with epilepsy and set up a support group for epilepsy to enhance their self-esteem as well as reduce their social anxiety.
[Abstract] Coping strategies and personality traits among individuals with brain injury and depressive symptoms
Posted by Kostas Pantremenos in Depression on October 23, 2020
Abstract
OBJECTIVE:The objective of this observational cohort study was to compare coping strategies and personality traits among individuals with acquired brain injury (ABI), based on their level of depression symptoms.
METHODS:Participants were recruited from an ABI outpatient clinic in Ontario, Canada. Participants were selected using the following inclusion criteria: 1) diagnosed with an ABI, 2) 18 years of age, and 3) able to read and write in English. Individuals completed the Patient Health Questionnaire 9-item (PHQ-9), Acceptance and Action Questionnaire, Anxiety Sensitivity Index, Adult Dispositional Hope Scale, Big Five Inventory, Brief Coping Orientation of Problems Experienced, and Rosenberg Self-Esteem Scale. A descriptive analysis was performed for the overall sample, as well as for each subclassification of depression: none (PHQ-9 = 0–4), mild (PHQ-9 = 5–9), moderate (PHQ-9 = 10–14), and severe (PHQ-9 = 15–27). A one-way multivariate analysis of variance, with post hoc Bonferroni-corrected tests, was conducted to assess the impact of depression symptoms on coping strategies and personality traits.
RESULTS:A total of 89 individuals (56.2% females) were included with a mean age of 46.6±15.1 years and a mean Glasgow Coma Scale score of 13.2±3.4. Overall, individuals were 3.5±4.3 years post injury. There was a statistically significant interaction effect between depression groups and the combined coping strategy and personality trait variables (F(36,128)=2.959, p < .001; Wilks’ Λ= .167). Individuals with mild (p = .045), moderate (p = .004) and severe (p < .001) depression symptoms had greater experiential avoidance (EA) than those without depression. Those with severe depression symptoms had significantly greater anxiety sensitivity than those with no (p < 0.001), mild, (p = .004) or moderate (p = .025) depression symptoms. Overall, individuals in the no, mild, and moderate depression groups used emotion-focused strategies primarily, followed by dysfunctional strategies for coping. Conversely, those with severe depression symptoms primarily used dysfunctional strategies, followed by emotion-focused strategies to cope. All depression groups applied problem-based coping strategies infrequently.
CONCLUSIONS:The use of passive coping strategies combined with increased EA behaviours among severely depressed individuals with ABI may lead to long-term negative outcomes. Programs that promote problem-based coping and reduce EA behaviours may be beneficial in reducing disability and impaired quality of life associated with depression symptoms in individuals with ABI.
[BLOG POST] How my self-esteem plummeted after a brain injury.
Posted by Kostas Pantremenos in Cognitive Rehabilitation, TBI on October 19, 2020

Before my brain injury, and being a realist about my strengths and weaknesses, I was comfortable with them. I was in my early 30’s, and had just got to that point when you really know yourself. Being honest with myself meant I achieved things by playing to my strong points, and asking for support on the things I wasn’t confident in. (Sounds obvious but previously I had been too scared to admit when I was finding something hard.) Life was good, and my self-esteem was in the best place it has ever been.
Enter stage left: Brain injury shakes everything up.
By now you will have heard me talk about how my career ended following my accident. And you might have read how looking for a new job didn’t pan out well for me in Unexpected interviewing disaster for TBI survivor. All of which is bad news for anyone’s self-esteem. But maybe that’s just ego, and I’m over that (sort of).
I have a problem with ME. My consciousness, spirit, soul…. whatever you want to call it. Weirdly, I’m not even sure that I’d noticed. That is until my partner, James, said to me “What’s with all the negative self talk?” This was after days of me listing my perceived faults at any given opportunity. I left like I was just being realistic and acknowledging the facts. But actually this is a change in my “self-concept.”
What is self-concept?
This is the feeling that you’re not the person you were, cognitively or physically, wrapped up in your level of self-esteem. But I’d been through to darkest phase of wondering what was the point of surviving my accident to be left with this inferior version of me. As I knew what that felt like, and how all-consuming it is to question your own existence, I had been brushing under the carpet what I was now feeling.
It appears to me that this can keep coming in waves or cycles. First when you return home and start to see how you can’t go back to life as it was is the first one. But then you adjust and on some level accept what you can achieve. However I allowed myself to be lulled into a false sense of security. Yes I’ve come a long way, and I do have a place in this world. But as my priorities had changed I’d let go of my vanity. I’d become fat and ugly. (Please don’t feel the need to write in telling me what a ‘beautiful’ woman I am. I realise that this is my inner voice being unreasonably hard on me, and I’m not attention seeking or craving compliments.) I think as my life moves forward my attention and priorities move. Thus I have become more interested again in my appearance and how the world sees me. Basically I am regretting letting myself go.

The importance of self-care.
I thought to worry about my appearance was self-centered. When you have been faced with your own mortality and continuing health issues it seemed trivial. But that’s really not the case. I know pride is one of the seven deadly sins and as I’m an atheist you might think I’m falling into its trap. But you have to look after yourself in order to have the strength to give to others. I know I said this before in Confess to pressure: being a voice of brain injury, so I’m not going to bang that drum again. Just know that it’s something that you have to keep coming back to and maintain it.
I know that as a natural part of aging everyone has to face changes in their life. Be it our role in society or how our bodies change, no one is immune. Of course each stage means we have to adjust, and sometimes it’ll be harder than others. You don’t need to feel like you’re failing just because it’s hard. After all, it’s the biggest challenges that teach us the most.
Other articles you might like:
- Unstable emotional lability after brain injury can be tense.
- TBI: Lost confidence.
- Terrified I’ll fail after brain injury.
Do you struggle with your self-esteem following a brain injury? Have you got an advice you want to give to others?
[WEB SITE] Cognitive Behavioral Therapy Benefits & Techniques
Posted by Kostas Pantremenos in Cognitive Rehabilitation on February 2, 2017
In today’s society, doctors and psychiatrists are quick to prescribe psychotropic drugs that often come with dangerous side effects for any disorder that stems from thought patterns. But what if I told you there was a better, safer way to manage and treat stress and brain disorders? Enter cognitive behavioral therapy.
According to the National Association of Cognitive Behavioral Therapists, cognitive behavioral therapy (often just called CBT) is a popular form of psychotherapy that emphasizes the importance of underlying thoughts in determining how we feel and act. Considered to be one of the most successful forms of psychotherapy to come around in decades, cognitive behavioral therapy has become the focus of hundreds of research studies. (1)
CBT therapists work with patients to help them uncover, investigate and change their own thought patterns and reactions, since these are really what cause our perceptions and determine our behaviors. Using CBT therapists offers patients valuable perspective, which helps improve their quality of life and manage stress better than patients simply “problem-solving” tough situations on their own.
Something that might surprise you about CBT: A core principle is that external situations, interactions with other people and negative events are not responsible for our poor moods and problem in most cases. Instead, CBT therapists actually view the opposite as being true. It’s, in fact, our own reactions to events, the things we tell ourselves about the events — which are within our control — that wind up affecting our quality of life.
This is great news — because it means we have the power to change. Through cognitive behavioral therapy, we can learn to change the way we think, which changes the way we feel, which in turn changes the way we view and handle tough situations when they arise. We can become better at intercepting disruptive thoughts that make us anxious, isolated, depressed, prone to emotionally eating and unwilling to change negative habits.
When we can accurately and calmly look at situations without distorting reality or adding additional judgments or fears, we’re better able to know how to react appropriately in a way that makes us feel happiest in the long run.
Proven Benefits of Cognitive Behavioral Therapy
A 2012 meta-analysis published in the Journal of Cognitive Therapy and Researchidentified 269 studies that supported the use of CBT for the following problems: (2)
- substance abuse disorders
- schizophrenia and other psychotic disorders
- depression and dysthymia
- manic depression/bipolar disorder
- anxiety disorders
- somatoform disorders
- eating disorders
- sleep disorders, including insomnia
- personality disorders
- anger and aggression
- criminal behaviors
- general stress and distress due to general medical conditions
- chronic fatigue syndrome
- muscle pains and tension
- pregnancy complications and female hormonal conditions
Researchers found the strongest support for CBT in treating anxiety disorders, somatoform disorders, bulimia, anger control problems and general stress. After reviewing 11 review studies comparing improvement rates between CBT and other therapy treatments, they found that CBT showed higher response rates than the comparison treatments in seven of the 11 reviews (more than 60 percent). Only one of 11 reviews reported that CBT had lower response rates than comparison treatments, leading researchers to believe that CBT is one of the most effective therapy treatments there is.
Here are some of the major ways cognitive behavioral therapy benefits patients from different walks of life:
1. Lowers Symptoms of Depression
Cognitive behavioral therapy is one of the best-known, empirically supported treatments for depression. Studies show that CBT helps patients overcome symptoms of depression like hopelessness, anger and low motivation, and lowers their risk for relapses in the future.
CBT is believed to work so well for relieving depression because it produces changes in cognition (thoughts) that fuel vicious cycles of negative feelings and rumination. Research published in the journal Cognitive Behavioral Therapy for Mood Disordersfound that CBT is so protective against acute episodes of depression that it can be used along with, or in place of, antidepressant medications. CBT has also shown promise as an approach for helping handle postpartum depression and as an adjunct to medication treatment for bipolar patients. (3)
2. Reduces Anxiety
According to work published in Dialogues in Clinical Neuroscience, there’s strong evidence regarding CBT treatment for anxiety-related disorders, including panic disorders, generalized anxiety disorder, social anxiety disorder, obsessive compulsive disorder and post-traumatic stress disorder. Overall, CBT demonstrates both efficacy in randomized controlled trials and effectiveness in naturalistic settings between patients with anxiety and therapists. (4)
Researchers have found that CBT works well as a natural remedy for anxiety because it includes various combinations of the following techniques: psycho-education about the nature of fear and anxiety, self-monitoring of symptoms, somatic exercises, cognitive restructuring (for example disconfirmation), image and in vivo exposure to feared stimuli (exposure therapy), weaning from ineffective safety signals, and relapse prevention.
3. Helps Treat Eating Disorders
The Journal of Psychiatric Clinics of North America reports that eating disorders provide one of the strongest indications for cognitive behavioral therapy. CBT has been found to help address the underlying psychopathology of eating disorders and question the over-evaluation of shape and weight. It can also interfere with the maintenance of unhealthy body weights, improve impulse control to help stop binge eating or purging, reduce feelings of isolation, and help patients become more comfortable around “trigger foods” or situations using exposure therapy. (5)
Cognitive therapy has become the treatment of choice for treating bulimia nervosa and “eating disorders not otherwise specified” (EDNOS), the two most common eating disorder diagnoses. There’s also evidence that it can be helpful in treating around 60 percent of patients with anorexia, considered to be one of the hardest mental illnesses to treat and prevent from returning.
4. Reduces Addictive Behaviors and Substance Abuse
Research has shown that CBT is effective for helping treat cannabis and other drug dependencies, such as opioid and alcohol dependence, plus helping people quit smoking cigarettes and gambling. Studies published in the Oxford Journal of Public Health involving treatments for smoking cessation have found that coping skills learned during CBT sessions were highly effective in reducing relapses in nicotine quitters and seem to be superior to other therapeutic approaches. (6) There’s also stronger support for CBT’s behavioral approaches (helping to stop impulses) in the treatment of problematic gambling addictions compared to control treatments. (7)
5. Helps Improve Self-Esteem and Confidence
Even if you don’t suffer from any serious mental problems at all, CBT can help you replace destructive, negative thoughts that lead to low self-esteem with positive affirmations and expectations. This can help open new ways to handle stress, improve relationships and increase motivation to try new things. The Psychology Tools website provides great resources for using CBT worksheets on your own to work on developing affirmative communication skills, healthy relationships and helpful stress-reducing techniques. (8)
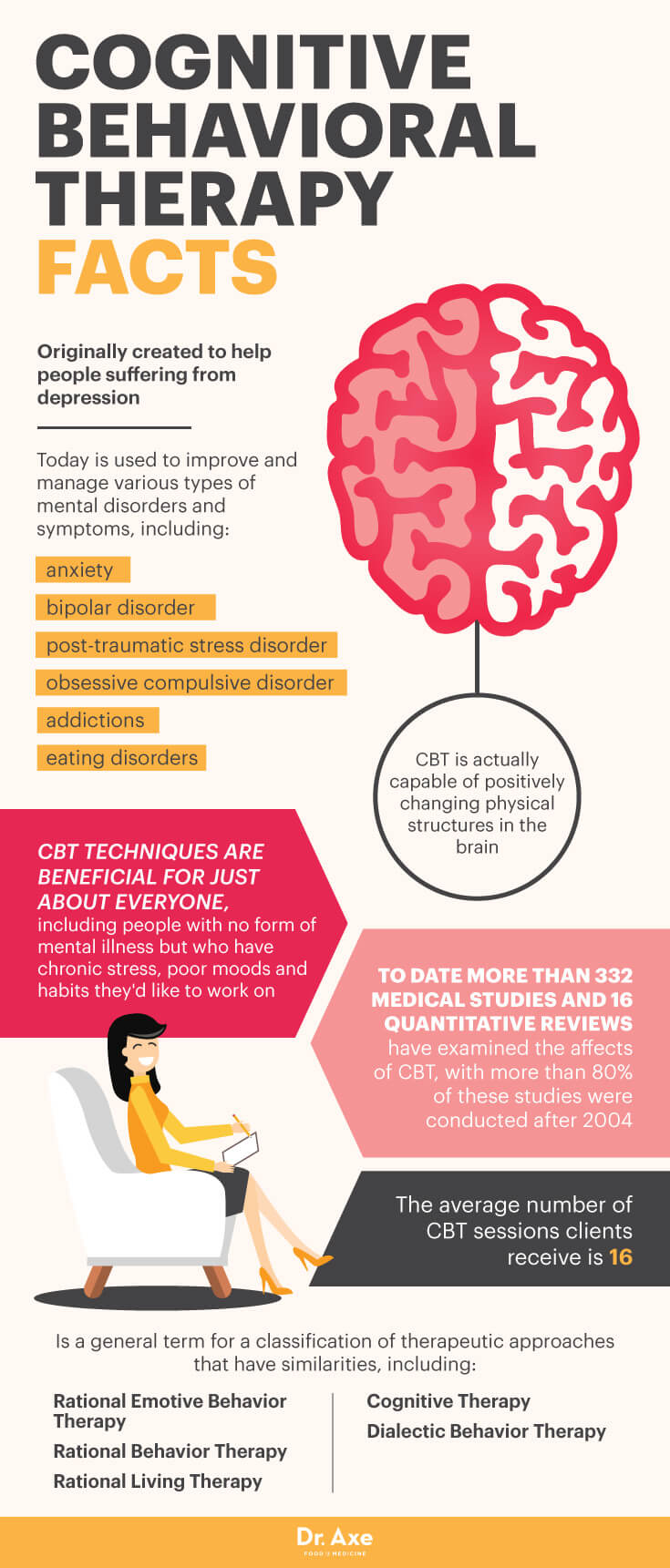
Facts About Cognitive Behavioral Therapy
- CBT was originally created to help people suffering from depression, but today it’s used to improve and manage various types of mental disorders and symptoms, including: anxiety, bipolar disorder, post-traumatic stress disorder, obsessive compulsive disorder, addictions and eating disorders. (9)
- CBT techniques are also beneficial for just about everyone else, including people with no form of mental illness but who have chronic stress, poor moods and habits they’d like to work on.
- The term cognitive behavioral therapy is considered a general term for a classification of therapeutic approaches that have similarities, including: rational emotive behavior therapy, rational behavior therapy, rational living therapy, cognitive therapy and dialectical behavior therapy.
- To date, more than 332 medical studies and 16 quantitative reviews have examined the effects of CBT. Interestingly, more than 80 percent of these studies were conducted after 2004. (10)
- Studies have found that in people who have completed CBT programs and then undergone brain scans, CBT is actually capable of positively changing physical structures in the brain. (11)
- CBT can work quickly, helping patients feel better and experience lessened symptoms within a short period of time (several months, for example). While many forms of therapy can take many months or even years to become very helpful, the average number of CBT sessions clients receive is only 16.
- CBT often involves the patient completing “homework” assignments on their own between therapy sessions, which is one of the reasons benefits can be experienced so quickly.
- In addition to homework being done by the patients while they’re alone, cognitive behavioral therapists also use instructions, questioning and “exposure therapy” during sessions. CBT is very interactive and collaborative. The therapist’s role is to listen, teach and encourage, while the patient’s role is to be open and expressive.
- One of the biggest advantages for patients is that CBT can be continued even after formal sessions with a therapist are over. Eventually, formal therapy ends, but at this point the clients can continue to work on exploring CBT concepts, using techniques they’ve learned, journaling and reading to help prolong benefits and manage symptoms.
How Cognitive Behavior Therapy Works
CBT works by pinpointing thoughts that continuously rise up, using them as signals for positive action and replacing them with healthier, more empowering alternatives.
The heart of CBT is learning self-coping skills, giving patients the ability to manage their own reactions/responses to situations more skillfully, change the thoughts they tell themselves, and practice “rational self-counseling.” While it definitely helps for the CBT therapist/counselor and patient to build trust and have a good relationship, the power really lies in the patient’s hands. How willing a patient is to explore his or her own thoughts, stay open-minded, complete homework assignments and practice patience during the CBT process all determine how beneficial CBT will be for them.
Some of the characteristics that make cognitive behavioral therapy unique and effective include:
- Rational approach: CBT theory and techniques are based on rational thinking, meaning they aim to identify and use facts. The “inductive method” of CBT encourages patients to examine their own perceptions and beliefs to see if they are in fact realistic. In CBT, there is an underlying assumption that most emotional and behavioral reactions are learned. Many times with a CBT therapists’s help, patients learn that their long-held assumptions and hypotheses are at least partially incorrect, which causes them unnecessary worrying and suffering. (12)
- Law of entropy and impermanence: CBT rests on scientific assumptions, including the law of entropy, which is essentially the fact that “if you don’t use it, you lose it.” We always have the power to change how we feel because our feelings are rooted in our brains’ chemical interactions, which are constantly evolving. If we break cycles of thought patterns, our brains will adjust for the better. MRI scans show the human brain creates and sustains neural synapses (connections) between frequent thoughts and emotions, so if you practice positive thinking your brain will actually make it easier to feel happier in the future.
- Accepting unpleasant or painful emotions: Many CBT therapists can help patients learn how to stay calm and clear-headed even when they’re faced with undesirable situations. Learning to accept difficult thoughts or emotions as being “simply part of life” is important, because this can help stop a vicious cycle from forming. Often we get upset about our tough feelings and add on even more suffering. Instead of adding self-blame, anger, frustration, sadness or disappointment to already-tough feelings, CBT teaches patients to calmly accept a problem without judgment in order to not make it even worse.
- Questioning and expressing: Cognitive behavioral therapists usually ask patients many questions in order to help them gain a new perspective, see the situation more clearly and realistically, and help them undercover how they really feel.
- Specific agendas and techniques: CBT is usually done in a series of sessions that each have a specific goal, concept or technique to work with. Unlike some other forms of therapy, sessions are not simply for the therapist and patient to talk openly without an agenda in mind. CBT therapists teach their clients how to better handle difficult thoughts and feelings by practicing specific techniques during sessions that can later be applied to life when they’re most needed.
Cognitive Behavioral Therapy vs. Other Types of Psychotherapy
CBT is a type of psychotherapy, which means it involves open talking between patient and therapist. You might have heard of several other forms of psychotherapy in the past and are wondering what makes CBT stand apart. Many times there is some overlap between different forms of psychotherapy. A therapist might use techniques from various psychotherapy approaches to help patients best reach their goals and improve (for example, to help someone with a phobia, CBT might be coupled with exposure therapy).
According to the National Alliance on Mental Illness, here is how CBT differs from other popular forms of therapy: (13)
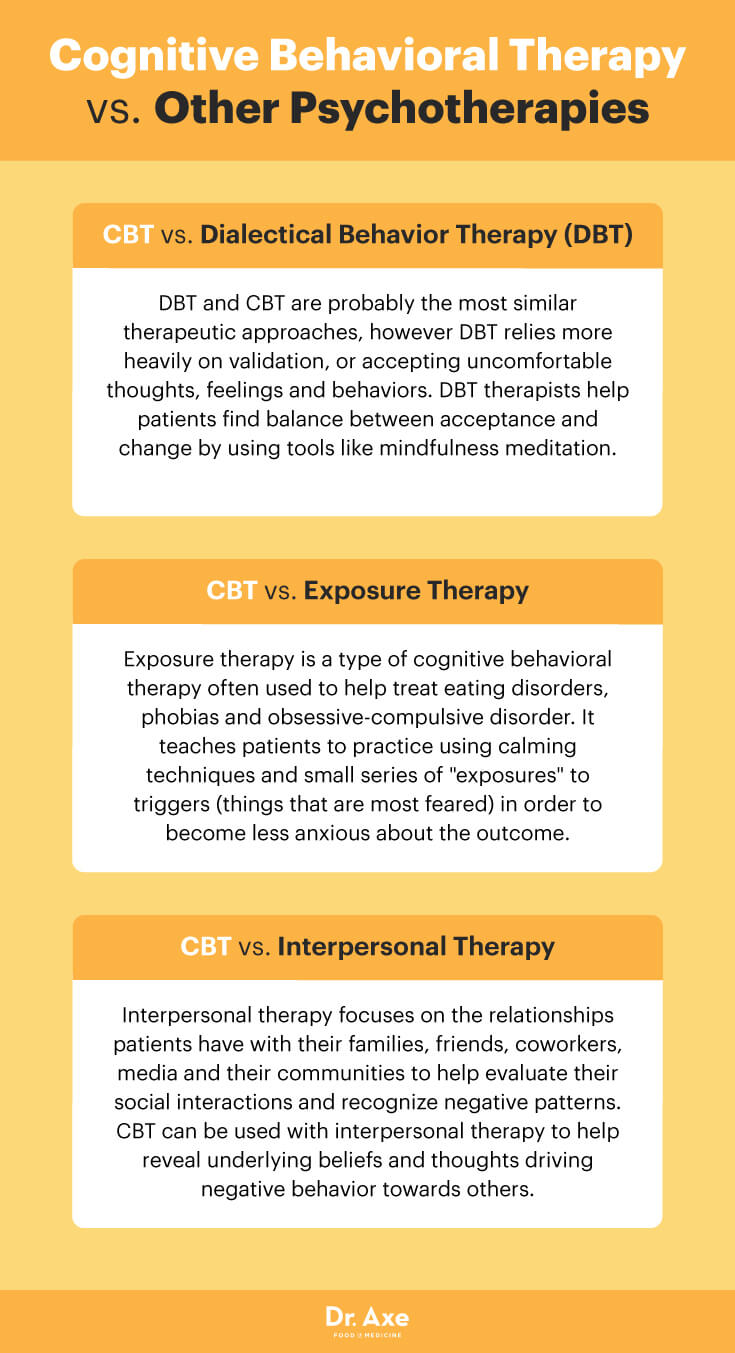
- CBT vs. Dialectical Behavior Therapy (DBT): DBT and CBT are probably the most similar therapeutic approaches, however DBT relies more heavily on validation or accepting uncomfortable thoughts, feelings and behaviors. DBT therapists help patients find balance between acceptance and change by using tools like mindfulness guided meditation.
- CBT vs. Exposure Therapy: Exposure therapy is a type of cognitive behavioral therapy that’s often used to help treat eating disorders, phobias and obsessive-compulsive disorder. It teaches patients to practice using calming techniques and small series of “exposures” to triggers (things that are most feared) in order to become less anxious about the outcome.
- CBT vs. Interpersonal Therapy: Interpersonal therapy focuses on the relationships a patient has with his or her family, friends, co-workers, media and community to help evaluate social interactions and recognize negative patterns (such as isolation, blame, jealousy or aggression). CBT can be used with interpersonal therapy to help reveal underlying beliefs and thoughts driving negative behavior toward others.
Ways to Practice Cognitive Behavioral Therapy Techniques on Your Own
- Identify your current obstacles: The first step is to identify what’s really causing you stress, unhappiness and unease. Maybe you’re feeling resentful toward someone, fearful of failure or worried about being rejected socially in some way. You might find that you have persistent anxiety, symptoms of depression or are struggling to forgive someone for a past event. Once you can recognize this and become more aware of your primary obstacle, then you have the power to start work on overcoming it.
- Try “thought recording”: You can use a journal or even record your own voice on a tape recorder to help you identify recurring destructive thoughts you frequently tell yourself. Ask yourself questions to dig deeper and form connections you weren’t previously aware of. Then reread your entries as if you were not yourself, but a good friend. What advice would you give yourself? What beliefs of yours can you notice aren’t very accurate, only making matters worse and not overall helpful?
- Form patterns and recognize your triggers: Think about what types of situations make you most likely to feel anxious, upset, critical or sad. Start to form patterns of behaving in certain ways or experiencing certain things (for example, maybe drinking too much alcohol or gossiping behind someone’s back) and how they leave you feeling, so you can start breaking the cycle.
- Notice how things are always changing: Feelings come and go constantly (called impermanence), so knowing that fear, anger or other strongly unplesant emotions are only temporary can help you stay calm in the moment.
- “Put yourself in their shoes”: It’s important to try and view situations as rationally, clearly and realistically as possible. It helps to consider other people’s perspectives, question your assumptions, and see if there’s something important you might be missing or ignoring.
- Thank yourself and be patient: Even though CBT works quickly for many people, it’s an ongoing process that’s essentially lifelong. There’s always ways to improve, feel happier, and treat others and yourself better, so practice being patient. Remind yourself there is no finish line. Give yourself credit for putting effort into facing your problems directly, and try to view “slip-ups” as inevitable parts of the journey and learning process.
Final Thoughts on Cognitive Behavioral Therapy
- CBT techniques are also beneficial for just about everyone else, including people with no form of mental illness but who have chronic stress, poor moods and habits they’d like to work on.
- Some of the major ways cognitive behavioral therapy benefits patients from different walks of life includes lowering symptoms of depressions, reducing anxiety, treating eating disorders, reduces addictive behaviors and substance abuse, and helps improve self-esteem and confidence.
- You can practice cognitive behavioral therapy by identifying your current obstacles, trying thought recording, forming patterns and recognizing your triggers, noticing how things are always changing, putting yourself in others’ shoes, and thanking yourself and being patient.
Source: Cognitive Behavioral Therapy Benefits & Techniques – Dr. Axe