Posts Tagged Keppra
[WEB] What To Avoid When Taking Keppra: Energy Drinks, Other Drugs, and More
Posted by Kostas Pantremenos in Epilepsy on September 14, 2023
If you take levetiracetam — sold as Keppra, Elepsia, and Spritam — to help manage your epilepsy, you may want to pass on that second Red Bull or frappuccino. Though levetiracetam can effectively treat certain types of seizures, taking it along with large quantities of caffeine — as well as with alcohol and other medications — can make it less effective or even cause harmful side effects.
Levetiracetam is an anti-seizure medication that comes in a few different forms: tablet, oral solution, or intravenous (IV) solution. Most people who take levetiracetam are prescribed the oral tablet form and they take it on a schedule every day at home. The IV form is given only in the hospital.
Members of MyEpilepsyTeam who take levetiracetam sometimes ask about how their epilepsy medication might interact with their favorite beverages. “I know alcohol messes with medications, but since when do people say Red Bull or any energy drink has an effect on seizure medication?” a member asked.
Another member described a seizure and hospitalization after consuming an energy drink. “I’ve noticed since I’ve been drinking these energy drinks, preferably Red Bull, Amp, Rockstar, or Monster … that it’s made me very dehydrated and I’ve had an increase of seizure activity … which ended up putting me into the hospital.”
Read on to learn about drinks that can interact with formulations of levetiracetam, what drink alternatives are available, and when to talk to your doctor about your anti-seizure medication.
Drinks To Avoid While Taking Levetiracetam
Certain drinks can increase your risk of having a seizure. These include beverages containing caffeine, sugar, and alcohol.
Energy Drinks
The makers of energy drinks such as Red Bull, Monster, 5-Hour Energy, and Rockstar market these beverages as an effective way to boost your physical and mental performance. However, these drinks aren’t regulated by the U.S. Food and Drug Administration (FDA), and they can be harmful if you’re not careful about how much you consume.
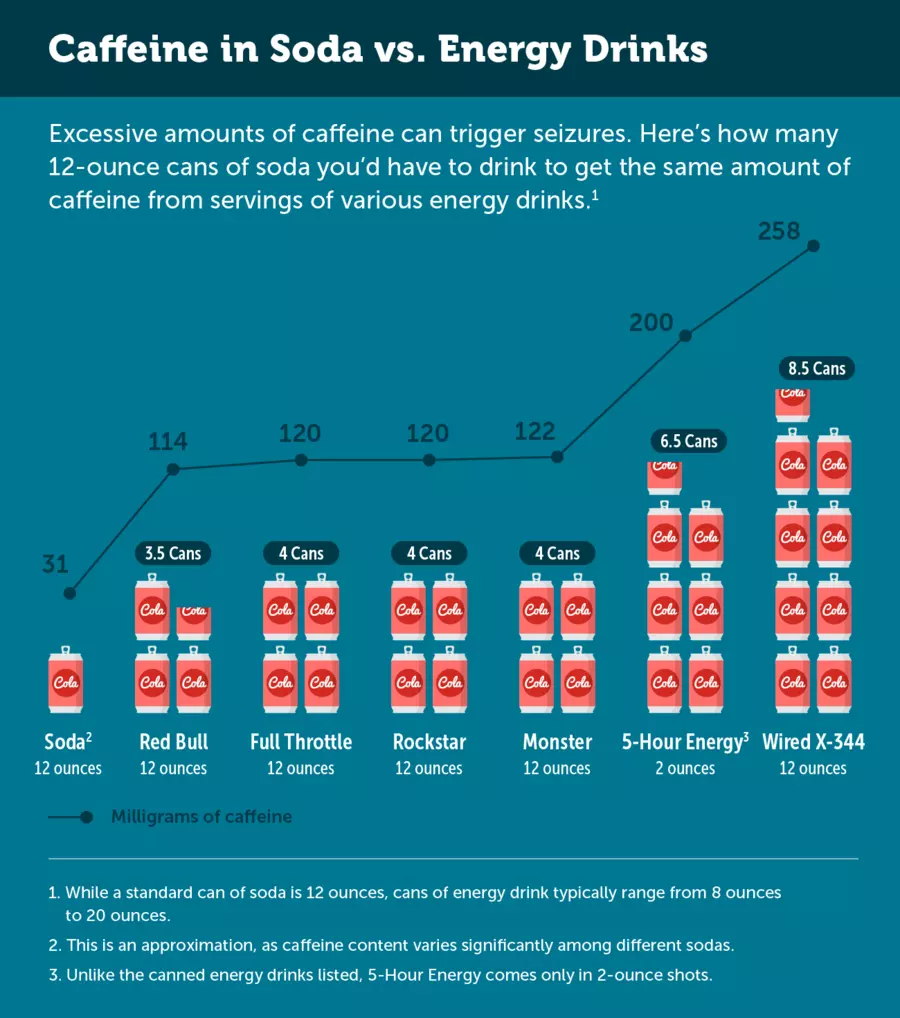
Energy drinks can be dangerous for anyone because they contain high amounts of caffeine, which is a stimulant. The amount of caffeine within an energy drink is usually substantially higher than what’s in a regular cup of coffee or can of soda.
Research has found that energy drinks can trigger seizures, even in people with no history of seizures. A 2014 study showed that children and adolescents are at particular risk for seizures from consuming energy drinks. Dehydration –– a known side effect of energy drinks –– can also lead to seizure.
Notably, some researchers believe that it’s not the stimulant itself that increases a perons’ risk of seizure. Rather, it’s the energy “crash” that happens after it wears off.
Additionally, research involving rats has found that high doses of caffeine may interfere with levetiracetam’s anticonvulsant action — that is, its ability to control seizures. More research is needed, though, to see whether the same holds true for humans.
High doses of caffeine can also cause:
- Tremor
- Agitation
- Heart rhythm abnormalities
- Heart palpitations (e.g., rapid fluttering heartbeat)
- High blood pressure
- Breathing difficulties
- Lightheadedness
Additionally, insomnia (an inability to sleep) can be a side effect of energy drinks. Tiredness or drowsiness is strongly linked with triggering a seizure.
Side effects of overdosing on caffeine can be severe enough to sometimes require a trip to the hospital.
Energy drinks often contain other ingredients that can affect your brain when consumed in high quantities, such as sweeteners, amino acids, guarana, and taurine.
Other Caffeinated Beverages
Caffeine from other sources, including caffeine shots and pills, coffee, soda, and tea, can also impact your seizure risk — especially if you have a low seizure threshold.
One member of MyEpilepsyTeam said “No. I don’t touch energy drinks or anything with caffeine because they will create triggers which lead to seizures. Especially with Keppra. Energy drinks will do twice the damage that coffee will do because of two to three times the caffeine.”
Alternatives to Caffeinated Drinks
In general, it’s safest for people who experience seizures to stay away from energy drinks and other beverages that contain high amounts of caffeine. Staying away from beverages with high amounts of sugar is also a good idea to prevent energy crashes. Be sure to drink plenty of water, given that caffeine and sugar can be dehydrating.
Tea, especially green tea, is a good alternative to highly caffeinated energy drinks when consumed in moderation. Decaffeinated coffee, teas, and sodas can also work well.
Instead of relying on caffeine and other stimulants for energy boosts, consider making some dietary changes. Eating a balanced diet high in protein is important for maintaining good energy levels, whether you’re living with epilepsy or not.
Alcohol
Moderate to large amounts of alcohol can also adversely interact with anti-seizure medication, making you feel intoxicated more quickly and lowering your seizure threshold. Alcohol withdrawal can also cause seizures and be life-threatening.
Mixing energy drinks and alcohol — which is a popular trend — can be even riskier than drinking alcohol by itself. One study used a medication to induce seizures in animals and compared the seizure onset time for those given an energy and alcohol to those who weren’t. The seizure onset time was significantly shorter in the energy drink and alcohol group.
Health experts advise that people who are taking anti-seizure medication avoid consuming alcohol. Like caffeine, drinking excessive amounts of alcohol can trigger seizures in people who’ve never had one before.
Medications To Avoid While Taking Levetiracetam
Several medications can interact with levetiracetam and cause serious health problems. In some cases, two medications should never be used together. In other cases, they can be as long as the doses are adjusted or other appropriate precautions are taken.
Medications and supplements that may have undesirable interactions with levetiracetam include:
- Methotrexate
- Orlistat
- Calcifediol
- Gingko
- Other anti-seizure medications, including carbamazepine and benzodiazepines
- Antihistamines (i.e, allergy medications)
- Antidepressants
- Antipsychotics
- Cannabis
- Clonidine
- General anesthesia medications
- Anticoagulants
- Opioids
This list does not include every medication that interacts with levetiracetam. If you are unsure about a medication, a new beverage, or a new food, it is always advised to seek professional medical advice. Note, too, that some drugs and medications can increase your risk of seizures.
Talk to Your Doctor
When taking any medication –– but especially an anti-seizure medication –– it’s important to follow the directions, dosing, and schedule directly as prescribed by your neurologist. A lot of different substances can have drug interactions, and it’s important to make sure you’re not accidentally increasing your risk for a seizure while taking Keppra.
Sometimes, even things we don’t think of can interact with medications. Herbs, supplements, and natural remedies can sometimes seriously affect the medications you’re taking or your risk of having a seizure. Be sure to talk with your doctor before adding anything new to your diet — including energy drinks.
Talk With Others Who Understand
MyEpilepsyTeam is the social network for people living with epilepsy and their loved ones. On MyEpilepsyTeam, more than 114,000 members come together to ask questions, give advice, and share their stories with others who understand life with epilepsy.
Are you taking levetiracetam for epilepsy and wondering about the risks of energy drinks? Share your experience in the comments below, or start a conversation by posting on your Activities page.
[WEB SITE] List of Seizures (Convulsions) Medications (60 Compared) – Drugs.com
Posted by Kostas Pantremenos in Epilepsy, Pharmacological on June 19, 2018
Medications for Seizures (Convulsions)
About Seizures: A seizure or convulsion can be a sudden, violent, uncontrollable contraction of a group of muscles. A seizure can also be more subtle, consisting of only a brief “loss of contact” or a few moments of what appears to be daydreaming.
See also: sub-topics
Drugs Used to Treat Seizures
The following list of medications are in some way related to, or used in the treatment of this condition.[…]
For the list of medications, Visit Site —> List of Seizures (Convulsions) Medications (60 Compared) – Drugs.com
[WEB SITE] Treating Levetiracetam-Induced Behavioral Effects With Vitamin B6
Posted by Kostas Pantremenos in Cognitive Rehabilitation, Epilepsy, Pharmacological on January 25, 2018

Data showed that 11.8% of levetiracetam-treated patients experienced behavioral side effects.
Daily pyridoxine (vitamin B6) was found to be an effective treatment for the behavioral adverse effects seen with the antiepileptic drug levetiracetam, according to a poster presented at the AES Annual Meeting 2017.
Treatment with levetiracetam (Keppra; UCB) has been shown to cause non-psychotic behavioral effects (eg, aggression, anger, emotional lability, anger, depression, anxiety) in clinical studies (13% in levetiracetam-treated patients vs 6% in placebo-treated). Currently, there is a lack of data regarding the treatment of behavioral effects of levetiracetam, which represents a key cause of treatment discontinuation.
For the retrospective study, Creighton University School of Medicine researchers evaluated whether pyridoxine supplementation could benefit patients who are experiencing behavioral adverse effects due to levetiracetam. The team reviewed electronic medical records of all patients in the Creighton University Epilepsy Center Clinic (2011–2015) for those taking levetiracetam. Forty-five of the 380 total patients receiving levetiracetam (median dose 1000mg daily; highest dose 4000mg daily) were initiated on pyridoxine 100mg daily for symptom control.
The data showed 11.8% of levetiracetam-treated patients experienced behavioral side effects with agitation, insomnia, and irritability being the most commonly observed. These behavioral changes were typically seen within the first month of starting levetiracetam therapy. Nearly all of the patients who received pyridoxine (42/45; 93.3%) remained on levetiracetam therapy as they saw significant improvement in their behavioral symptoms.
“This benefit is seen across the entire range of levetiracetam dosing,” lead author Kalyan Sajja noted. Supplementation with pyridoxine 100mg daily enabled continued treatment with levetiracetam in these patients. The authors added that a large multicenter, prospective, randomized-controlled trial can further validate this clinical benefit.
Reference
Sajja K, Sankaraneni R, Galla K, Singh SP. Role of Pyridoxine (Vitamin B6) in the Treatment of Levetiracetam Induced Behavioral Effects in Epilepsy Patients. Presented at: AES annual meeting in Washington, DC. Abstract 1.308.
via Treating Levetiracetam-Induced Behavioral Effects With Vitamin B6
[WEB SITE] Keppra – The Law Offices of Gregory Krasovsky
Posted by Kostas Pantremenos in Epilepsy on September 22, 2017
Keppra
The dangerous drug attorneys at the Law Offices of Gregory Krasovsky can provide legal advice and representation to individuals and families considering pursuing a Keppra lawsuit. In order for a plaintiff to secure a maximum settlement in litigation of a Keppra claim, regardless of whether in an individual lawsuit or in a class action lawsuit, it is crucial that the law firm representing you have a competent and experienced team of Keppra lawyers to guide you through all of the legal hurdles as well as direct you to sufficient funding (litigation funding or legal finance) to cover pharmaceutical litigation costs. Contact a Keppra attorney today to schedule a free consultation and take your first step to obtaining compensation for losses caused by Keppra side effects.
Keppra, which is generically known as Levetiracetam, is an anticonvulsant drug used to treat epilepsy. Keppra was originally manufactured and marketed by UCB Pharmaceuticals Inc., but now it is available as a generic and is manufactured by a number of firms. Unfortunately, Keppra has a number of serious side effects that can, at times, outweigh its benefits for people who are suffering from epilepsy. Some of the most serious Keppra adverse effects include suicidal tendencies and birth defects.
There are many Levetiracetam side effects. These include, but are not limited to, the following:
- Suicidal Ideation
- Suicidal Tendencies
- Suicide
- Headache
- Unsteady Walk
- Depression
- Hallucinations
- Fever
- Sore Throat
- Mood Changes
- Changes in Skin Color
- Anxiety
- Birth Defects
A 2005 Food and Drug Administration (FDA) study of suicidal ideation in relation to epilepsy drugs has indicated that people taking those drugs, such as Keppra, are twice as likely to suffer from suicidal thoughts as are those who have not been taking these drugs.
Unlike many other drugs, such as Wellbutrin, people taking Keppra are likely to experience suicidal ideation regardless of what age group they might happen to fall into. The aforementioned study tracked almost 30,000 people, and the rick of suicide was spread fairly evenly across the population. Of the 28,000 people who had taken Keppra in this study, four of them had actually committed suicide. These unfortunate incidents serve to confirm the danger of this unsafe drug.
Although Keppra’s ability to cause birth defects is still under investigation, there is some amount of evidence that seems to confirm that Keppra is more harmful to unborn babies than was previously thought. Currently, the FDA has placed Keppra in the Category C for pregnancy, which indicates that there is little human risk. However, AdverseEvents, Inc. believes that Keppra should perhapd be in Category D, which indicates that a significant enough risk to pregnancy exists.
Keppra is similar to another prototypical nootropic drug called piracetam. Keppra is also thought to be a possible treatment for Tourette syndrome, autism, bipolar disorder, and anxiety disorder.
The attorneys at this Keppra law firm believe that drugs should not cause the same ailments that they are meant to cure. If you or your loved one has been injured as a result of taking Keppra, you might be entitled to compensation. Contact our attorneys today to schedule a free consultation.
[WEB SITE] Newer Epilepsy Drugs May Be Safer During Pregnancy: MedlinePlus
Posted by Kostas Pantremenos in Epilepsy on September 8, 2016
Newer Epilepsy Drugs May Be Safer During Pregnancy
Small British study says two drugs don’t harm a child’s mental development, but popular older one does
THURSDAY, Sept. 1, 2016 (HealthDay News) — Women who take the new epilepsy drugs levetiracetam and topiramate during pregnancy don’t run the risk of harming their infant’s mental development, British researchers report.
But the commonly prescribed anti-seizure drug valproate was linked with lower IQs in children, especially when taken at higher doses, researchers say.
“The treatment of epilepsy in women who are considering a pregnancy or are pregnant involves optimizing the health of the mother as well as keeping the risk to the fetus as low as possible,” said lead researcher Rebecca Bromley, a research fellow at the Institute for Human Development at the University of Manchester.
In the study, children exposed to levetiracetam (Keppra) or topiramate (Topamax) in the womb did not differ from children not exposed to these drugs. And they had better outcomes than the children exposed to valproate (Depakote) in terms of their IQ, thinking and language skills, Bromley said.
“These data can be used by doctors and women to help them make their decisions about which medication is best for them,” she added.
For the study, Bromley and her colleagues used the U.K. Epilepsy and Pregnancy Register to identify 171 women with epilepsy who had a child between 5 and 9 years old. During their pregnancy, 42 of the women took levetiracetam, 27 took topiramate, and 47 took valproate, the researchers said.
Bromley’s team compared the women with epilepsy with 55 women who did not take epilepsy drugs during pregnancy. The children had their IQ measured and took tests on verbal and nonverbal comprehension and how fast they could process visual information.
The researchers found that children of women who took levetiracetam or topiramate did not have lower IQs or other thinking-skill problems, compared with kids of mothers who did not take these drugs, no matter what dose of these drugs were taken.
Children whose mothers took valproate, however, had the lowest IQs of the study, Bromley said. These kids scored, on average, 11 points lower on the IQ test.
Among children whose mothers took valproate, 19 percent had IQs lower than the average score of 100, compared with 6 percent among kids whose mothers did not take any epilepsy drugs during pregnancy, the researchers found.
Because the registry the researchers used does not include all women with epilepsy, the findings might not apply to all women with the conditions, Bromley noted. She also said that topiramate, one of the newer drugs, has been associated with an increased risk of birth defects, such as cleft lip and palate.
The study was funded by Epilepsy Research U.K. and the report was published online Aug. 31 in the journal Neurology.
Dr. Ian Miller is a pediatric neurologist and medical director of the comprehensive epilepsy program at Nicklaus Children’s Hospital in Miami. “This study means that we have a little bit more information for women who become pregnant while taking epilepsy medicines,” he said.
The exact risks of taking any medicine during pregnancy are very difficult to know, he added.
“As a result, many questions remain,” Miller said. “But this study gives doctors a reason to choose topiramate or levetiracetam, which did not show a measurable effect on the child’s development, rather than valproate, which did.”
Women who are on valproate because they already tried other medications and “moved on because those medications were less effective, will face some difficult decisions,” he said.
“Any woman of childbearing potential should discuss this aspect of their medical management with their doctor, especially in light of these new findings,” Miller added.
SOURCES: Rebecca Bromley, Ph.D., research fellow, Institute for Human Development, University of Manchester, England; Ian Miller, M.D., pediatric neurologist, and medical director, comprehensive epilepsy program, Nicklaus Children’s Hospital, Miami; Aug. 31, 2016, Neurology, online
- More Health News on:
- Epilepsy
- Pregnancy and Medicines
Source: Newer Epilepsy Drugs May Be Safer During Pregnancy: MedlinePlus
[WEB SITE] Why Am I Having Seizures Seven Years Post-Brain Injury? – braineline.org
Posted by Kostas Pantremenos in Epilepsy on October 22, 2015
Question
I had a subdural hematoma from a rock climbing fall back in 2003. I was rescued by helicopter and taken to a trauma center where I had a craniotomy to stop the bleeding. I was told by the surgeons that I had an excellent chance of a full recovery, which proved to be true after about five months.
In January 2010, I had a grand mal seizure. After MRIs and an EEG, the seizure was thought to be a one-time event due to drinking too much and then coming home and taking some prescription sleep medication, which lowered my seizure threshold.
But a month ago, I had a tonic-clonic seizure totally by surprise. I was at a meeting and was not drinking. I had been working extremely hard and not sleeping well as a result. I was told to take 1,000 of Keppra per day which had terrible side affects. I cut back the Keppra to 250mg before bedtime and that’s all. My doctor is sending me another brand of medication to try.
Why would I have seizures seven years after the accident? And, what are the chances of staying off medication and just taking good care of myself? I have been sleeping regularly and better, quit drinking alcohol, exercising, doing meditation and yoga, and I feel great.
Answer
Aproximately…..
Continue —> Why Am I Having Seizures Seven Years Post-Brain Injury?
[WEB SITE] Do You Use Levetiracetam to Treat Status Epilepticus?
Posted by Kostas Pantremenos in Epilepsy on April 9, 2015
A Refresher: Treating Status Epilepticus in the ICU
I was working in the intensive care unit (ICU) the other night when I was called to the emergency department to see a patient who was reported to be in status epilepticus (SE). The patient had received several doses of lorazepam (Ativan®) and was loaded with intravenous levetiracetam (Keppra®). I hadn’t ever used levetiracetam for patients with SE before, so I went ahead and loaded the patient with fosphenytoin (Cerebyx®). I’d hardly call myself an expert in neurocritical care, so I figured it was time to go back and read about the management of SE in the ICU.
There’s no shortage of review articles out there, but I started with guidelines published by the Neurocritical Care Society in 2012.[1] Levetiracetam is on the list of agents recommended for emergent, urgent, and refractory treatment of SE. All levetiracetam recommendations are class IIb/level C (more data are needed, but treatment is not unreasonable based on consensus opinion, case reports, or standard of care).[1]
A quick look at the available references confirms that most are small case reports or observational case series. A recent review says that the practice of using levetiracetam shows promise—citing efficacy, safety, and tolerability across studies and one pilot study that compared levetiracetam to lorazepam.[2] They also noted that the Neurocritical Care Society guidelines list no serious adverse effects and minimal drug interactions. Perhaps levetiracetam is the ideal drug to use in the elderly and in the ICU.
To be clear, I’ll still be using lorazepam as my first line based on the results from the Veterans Affairs Status Epilepticus Cooperative Study Group.[3] It’s absolutely the best designed study on SE that we have. For urgent control, levetiracetam sure looks like a reasonable option when compared with fosphenytoin, which often causes hypotension.
Cost: A Reasonable Consideration
Of course, cost must be considered, and while I was unable to find a cost-efficacy analysis specific to SE treatment, studies looking at levetiracetam vs phenytoin for prophylaxis after traumatic brain injury clearly favored phenytoin.[4,5]
It’s not clear that these data can be readily generalized to SE treatment. In summary, for patients who are elderly, hemodynamically unstable, or on multiple medications, I’ll be using levetiracetam at the doses recommended in the recent guidelines.[1]
[WEB SITE] Keppra (Levetiracetam) Drug Information: Description, User Reviews, Drug Side Effects, Interactions
Posted by Kostas Pantremenos in Epilepsy on August 22, 2014
KEPPRA is an antiepileptic drug available as 250 mg (blue), 500 mg (yellow), 750 mg (orange), and 1000 mg (white) tablets and as a clear, colorless, grape-flavored liquid (100 mg/mL) for oral administration…
More Fetal Risks Linked to Epilepsy Drugs
Posted by Kostas Pantremenos in Epilepsy on August 20, 2014
…Fetal exposure to anti-epileptic drugs (AEDs) appears to carry risks beyond those congenital defects currently listed on the products’ labels, a researcher said here…
[ARTICLE] Post-traumatic epilepsy: current and emerging treatment options – Full Text PDF or HTML
Posted by Kostas Pantremenos in Epilepsy on August 17, 2014
…Traumatic brain injury (TBI) leads to many undesired problems and complications, including immediate and long-term seizures/epilepsy, changes in mood, behavioral, and personality problems, cognitive and motor deficits, movement disorders, and sleep problems. Clinicians involved in the treatment of patients with acute TBI need to be aware of a number of issues, including the incidence and prevalence of early seizures and post-traumatic epilepsy (PTE), comorbidities associated with seizures and anticonvulsant therapies, and factors that can contribute to their emergence…
μέσω Post-traumatic epilepsy: current and emerging treatment options | NDT.
