Resilience is not a trait that you are either born with or without. It’s a set of behaviors, thoughts, and actions that can be learned and developed. When you break it down to the physical level in your brain, resilience is a neuroplastic process. It’s really about how well your brain handles stress.
What is Resilience?
Resilience is the process of adapting in the face of adversity, trauma, tragedy, threats or significant sources of stress, such as family or relationship problems, serious health challenges, or workplace and financial issues. Essentially, it’s “bouncing back” from life’s difficult experiences.
Being resilient doesn’t mean that you don’t experience hard times. In fact, intense emotional pain, extreme trauma, and severe adversity are common in people who are considered resilient. The road to resilience most often involves considerable hardship. That’s how these people get resilient. Their brains build it. A resilient brain even has physical differences.
What a Resilient Brain Looks Like
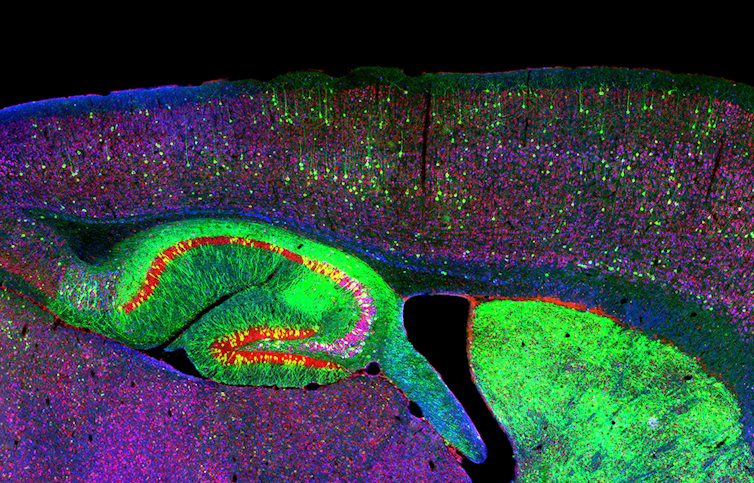
According to Richard Davidson in his book, The Emotional Life of Your Brain, resilience is one dimension of your emotional style and includes greater activation in the left prefrontal cortex (PFC) of the brain. Davidson writes:
The amount of activation in the left prefrontal region of a resilient person can be thirty times that in someone who is not resilient.”
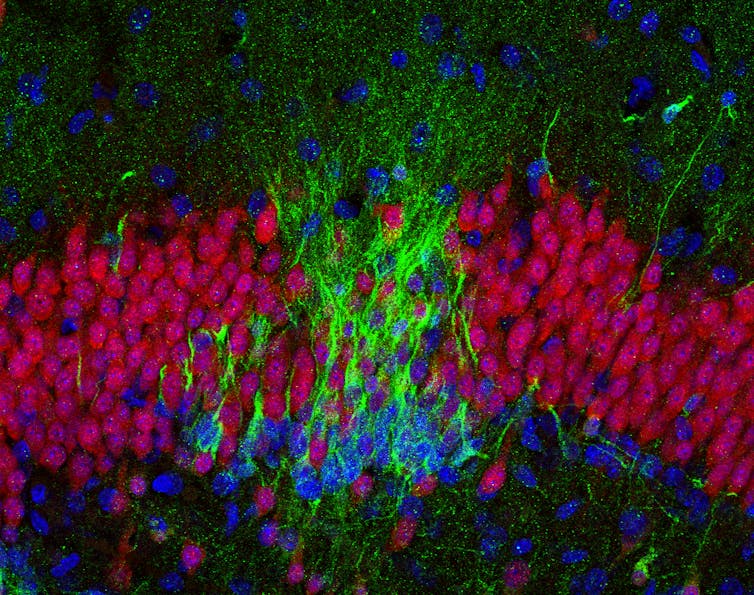
Davidson’s early research found that the abundance of signals back and forth from the PFC to the amygdala determines how quickly the brain recovers from being upset. The amygdala is your brain’s threat detector responsible for the fight-or-flight response. More activity in the left PFC shortens the period of amygdala activation. Less activation in certain zones of the PFC resulted in longer amygdala activity after an experience producing negative emotions. Basically, some people’s brains weren’t good at turning off negative emotion once it was turned on.
In later research with the help of MRIs, Davidson confirmed that the more white matter (axons connecting neurons) lying between the prefrontal cortex and the amygdala, the more resilient a person was. The converse was also true. Less white matter equates with less resilience. By turning down the amygdala, the PFC is able to quiet signals associated with negative emotions. The brain can then plan and act effectively without being overly influenced by negative emotions.
Don’t despair if you aren’t currently resilient. Every brain is capable of building more connections between the brain regions.
12 Inner Strengths that Build Resilience
In his book, Resilient: How to Grow an Unshakable Core of Calm, Strength, and Happiness, Rick Hanson writes:
Mental Resources like determination, self-worth, and kindness are what make us resilient: able to cope with adversity and push through challenges in the pursuit of opportunities. While resilience helps us recover from loss and trauma, it offers much more than that. True resilience fosters well-being, an underlying sense of happiness, love, and peace. Remarkably, as you internalize experiences of well-being, that builds inner strengths which in turn make you more resilient. Well-being and resilience promote each other in an upward spiral.”
Hanson goes on to tell us that you can build a more resilient brain in the same way you would strengthen your muscles. You do it through lots of little efforts that add up over time. Little efforts throughout your day can result in real physical changes for a better brain. You can teach your brain to be more resilient by working on the following 12 primary inner strengths:
Compassion
Compassion can be extended to yourself and others. Not to be confused with self-pity, complacency or arrogance, self-compassion involves acknowledging your own suffering, faults, and mistakes and responding with kindness, caring, and understanding, without judgment or evaluation. It’s talking to and treating yourself as you would a friend. It’s seeing your troubles and screw-ups as part of being human.
To practice self-compassion requires finding a healthy balance between self-acceptance and working for self-improvement. Instead of criticizing yourself for making a mistake or drowning in pity when things don’t go your way, you adopt a kind, but realistic view of your experience. Kristin Neff, Ph.D., a pioneer in self-compassion research, identifies three main components of the trait:
- Self-kindness – Become aware of your negative self-talk and replace the inner critic with a kinder, gentler voice.
- Common humanity – Acknowledge that suffering and personal failure are part of the universal experience of being human.
- Mindfulness – Observe your negative emotions without reacting to, focusing on, or suppressing them.
Research shows that self-compassion is a determining factor in whether life events become setbacks from which you don’t recover or stepping stones on the path forward.
Mindfulness
Mindfulness is a way of thinking. At the most basic level, it’s simply being aware of what’s happening as it’s happening. Being mindful means that you become aware of the workings of your mind, at that moment. When practicing mindfulness, you deliberately direct your awareness back into the now and focus your attention there. In essence, mindfulness is training your brain. In The Meaning Of Mindfulness, I explain the five basic factors that tend to be included in all mindfulness philosophies.
By following this pattern of thought repeatedly, over time, your brain actually physically changes. Through the process of neuroplasticity, the brain forms new connections and default neuronal pathways to support this kind of thinking, even when not consciously engaging in mindfulness. The consistent practice of mindfulness calms your brain and changes its default mode of operation.
Every brain is capable of building resilience.
Learning
You change your brain through learning. Learning is a neuroplastic process. Any lasting change of mood, outlook or behavior requires learning. Science shows that only about a third of your attributes are innate in your DNA. The other two-thirds are learned.
Hanson tells us that one effective way to teach our brains to be happier, more optimistic, confident, and resilient is by having and internalizing small experiences of safety, satisfaction, and connection throughout your day. He calls this “taking in the good“. You do this through a process he calls HEAL.
- Have a good experience.
- Enrich it.
- Absorb it.
- Link positive and negative.
Grit
Hanson defines grit as “dogged, tough resourcefulness. It’s what remains after all else has been worn down”. On his website, he says:
Much of our success in life comes down to our ability to identify the things we’re passionate about, pursue them with consistency, and keep going when things get tough. Anyone can be passionate and productive for a few days, or when things are easy. But to keep going day after day when the weather gets rough? That’s when we need grit.”
He describes grit as being based on several things:
- Agency is the sense of being a cause rather than an effect. It’s the opposite of helplessness.
- Determination is the steadfast fortitude you draw on to cope with, endure, and survive challenging events.
- Resolve is focused effort and passion towards a goal.
- Patience is the ability to delay gratification and distress tolerance.
- Persistence is sustained efforts over time.
Gratitude
Because of a negativity bias, your brain always notices, focuses on, and hangs on to what is less than ideal or potential problems. This tendency to notice and never forget the bad is just your brain doing its job, protecting you. Your brain has a good reason for its natural negativity. Your ancestors were more likely to live long enough to pass on their genes by remembering where they were chased by a predator than a prime napping spot. For this reason, there could be a tremendous amount of good in your life, but your brain doesn’t even notice it. In order to counteract this tendency, you have to intentionally look for, put emphasis on, and internalize the good that is in your life.
One way to do this is through gratitude. A wealth of research has proven significant benefits of gratitude for mental and physical health. Studies show that the practice of gratitude can increase happiness levels by an average of 25 percent and overall health by, for example, increasing the quantity and quality of sleep. Beneficial outcomes can be achieved by such simple practices as praying, writing in a gratitude journal, placing a thankful phone call, making a mental gratitude list, or writing a thank-you letter to someone.
Confidence
Confidence is developed throughout childhood and adulthood from interactions with parents, siblings, bosses, partners, friends, and enemies. If things go pretty well, you acquire a sense of worth, being cared about, and the ability to handle life. However, if a person experiences too much disapproval and rejection without accompanying encouragement and support, they can become insecure and self-critical.
No matter what has happened in the past, you can develop your confidence by training your brain to look for opportunities to support and encourage yourself. You can do this by looking for wins, accomplishments, and strengths with which to support and encourage yourself. This also requires that you become aware of your inner dialogue. Notice when it’s critical, shaming, discouraging, or judgemental. Reframe and work with your thoughts to help you.
Calm
Unfortunately, the modern world pushes many of us into a chronic state of fight-or-flight where our sympathetic nervous sytems (SNS) are frequently or continuously activated. It’s normal to experience fear, anger, helplessness, and overwhelm from time to time. However, the cumulative damage of chronically over stimulating the SNS leads to many physical and mental health problems.
The counter to the SNS is the parasympathetic nervous system (PNS). It’s often called the rest and digest system. You can think of the SNS as your gas pedal and the PNS as the brake. In his book, Buddha’s Brain: The Practical Neuroscience of Happiness, Love, and Wisdom, Hanson suggests that you want to strive to exist predominantly in a baseline state PNS arousal of calm peacefulness with mild SNS activations for enthusiasm, vitality, wholesome passions, and occasional spikes to deal with demanding situations.
Hanson advises us to look for ways that we are overestimating threats, which activate the SNS, and underestimating our resources to deal with them. Then, you can utilize other practices to calm your brain and body.
Motivation
Resilience involves the continuing pursuit of goals even in the face of challenges. Motivation keeps a person moving forward. Motivation involves your brain’s reward circuit and dopamine. Dopamine gives the brain an energetic, pleasurable feeling and is responsible for reward-seeking behavior. It’s the primary neurotransmitter behind any addiction.
Your brain has a fundamental motivation circuit based on dopamine activity. Everybody has natural variations in the amount of dopamine produced. There are many ways to naturally increase dopamine. You can also strengthen this circuit by increasing the association between rewards and what you are trying to motivate yourself towards. You do this by noting your accomplishments — even the small ones — with rewards and really paying attention to and internalizing them.
Intimacy
Different degrees of intimacy are present in all relationships. Intimacy requires a balance between being vulnerable and a sense of boundaries and asserting yourself. Intimacy also requires the ability to empathize with others. Hanson writes:
Empathy is the foundation of the sense that ‘I am not alone, others are with me, we are in this together, we share a common humanity.”
You can develop and grow your empathy.
Courage
You may think you need courage to do the big things in life. However, it’s often the little, everyday interactions with others that need us to be courageous. Open, authentic communication requires that we take some risk. Oftentimes, it takes courage to be truthful and assert yourself in any relationship. This doesn’t mean that you need to forcefully make demands. It means to skillfully express yourself with good intentions while keeping an eye on the results you wish to achieve.
Aspire
To aspire is an inherent part of being alive. In his book, Resilient: How to Grow an Unshakable Core of Calm, Strength, and Happiness, Hanson says:
To live is to lean into the future. We’re always stretching toward one thing or another: the next person, the next task, the next sight or sound, the next breath.”
In this life, it’s important to meet your need for satisfaction by reaching for results that have meaning to you — whatever those may be. If you don’t have any idea, Hanson suggests that you look back to what you dreamed about and were interested in when you were young. Think about what you hoped for before the world taught you “to be sensible” and “avoid risks.” (That’s how I started writing. Life had made me “forget” my childhood dreams of being a writer. Two books and hundreds of articles later, I am a writer!)
Hanson cautions us that it is important to aspire without attachment. That means to work towards a goal, but to manage your expectations and be fundamentally at peace with whatever happens. I know — easier said than done, but it is possible. It requires a growth mindset and being OK with failure.
Resilience is not a trait that you are born with or without. You can build it.
Generosity
Generosity is a positive cycle. It fills you up and strengthens you mentally and emotionally while connecting you with others which gives you even more to offer. The essence of generosity is altruism, which is giving without expecting anything in return. Humans evolved to be generous. It’s in our DNA. The generosity of one individual — sharing food, protecting from danger, increased the chances of survival for others.
Generosity doesn’t have to be material and often is not. Many times throughout a day you may be generous with your time, attention, patience, forgiveness, or encouragement. However, this does not mean to give because you are pressured or manipulated into it or to the point it is detrimental to you.
Source: The Best Brain Possible