-
1.Mathers, C., Fat, D.M., Boerma, J.T., World Health Organization: The global burden of disease: 2004 update. World Health Organization (2008)Google Scholar
-
2.McPhee, S.J., Hammer, G.D.: Nervous system disorders. Pathophysiol. Dis. Introd. Clin. Med. 59, 177–180 (2010)Google Scholar
-
3.Committee on Nervous System Disorders in Developing Countries the Board on Global Health and the Institute of Medicine. Neurological, Psychiatric, and Develop-Mental Disorders. National Academies Press, Washington, DC (2001)Google Scholar
-
4.Zhang, Y., Arakalian, V.: Design of a passive robotic ExoSuit for carrying heavy loads. In: Proceedings of the IEEE-RAS, 18th Annual International Conference on Humanoid Robots, Lyon, France (2018)Google Scholar
-
5.Gross, R., et al.: Modulation of lower limb muscle activity induced by curved walking in typically developing children. Gait Posture 50, 34–41 (2016)CrossRefGoogle Scholar
-
6.Viteckova, S., Kutilek, P., Jirina, M.: Wearable lower limb robotics: a review. Biocybern. Biomed. Eng. 33(2), 96–105 (2013)CrossRefGoogle Scholar
-
7.Rupala, B.S., Singla, A., Virk, G.S.: Lower limb exoskeletons: a brief review. In: Proceedings of the Conference on Mechanical Engineering and Technology COMET, Varanasi, Utter Pradesh, pp. 18–24 (2016)Google Scholar
-
8.Collo, A., Bonnet, V., Venture, G.: A quasi-passive lower limb exoskeleton for partial body weight support. In: Proceedings of the 6th IEEE/RAS-EMBS International Conference on Biomedical Robotics and Biomechatronics (BioRob), UTown, Singapore, pp. 643–648 (2016)Google Scholar
-
9.Stewart, A.M., Pretty, C.G., Adams, M., Chen, X.: Review of upper limb hybrid exoskeletons. IFAC 50(1), 15169–15178 (2017)Google Scholar
-
10.Serea, F., Poboroniuc, M., Hartopanu, S., Olaru, R.: Exoskeleton for upper arm rehabilitation for disabled patients. In: International Conference and Exposition on Electrical and Power Engineering, (EPE 2014), pp. 153–157 (2014)Google Scholar
-
11.Perry, J.C., Rosen, J., Burns, S.: Upper-limb powered exoskeleton design. IEEE/ASM Trans. Mechatron. 12(4), 408–417 (2007)CrossRefGoogle Scholar
-
12.Li, B., Yuan, B., Chen, J., Zuo, Y., Yang, Y.: Mechanical design and human-machine coupling dynamic analysis of a lower extremity exoskeleton. In: Huang, Y., Wu, H., Liu, H., Yin, Z. (eds.) ICIRA 2017. LNCS (LNAI), vol. 10462, pp. 593–604. Springer, Cham (2017). https://doi.org/10.1007/978-3-319-65289-4_56CrossRefGoogle Scholar
-
13.Jarrasé, N.: Contributions à l’explotation d’exosquelettes actifs pour la rééducation neuromotrice. Ph.D. thesis of Pierre et Marie Curie University (UPMC) (2010)Google Scholar
-
14.Gunn, M., Shank, T.M., Epps, M., Hossain, J., Rahman, T.: User evaluation of a dynamic arm orthosis for people with neuromuscular disorders. IEEE Trans. Neural Syst. Rehabil. Eng. 24(12), 1277–1283 (2016)CrossRefGoogle Scholar
-
15.Seth, D., Chablat, D., Bennis, F., Sakka, S., Jubeau, M., Nordez, A.: New dynamic muscle fatigue model to limit musculo-skeletal disorder. In: Virtual Reality International Conference 2016, Article no. 26 (2016)Google Scholar
-
16.Seth, D., Chablat, D., Sakka, S., Bennis, F.: Experimental validation of a new dynamic muscle fatigue model. In: Duffy, V.G.G. (ed.) DHM 2016. LNCS, vol. 9745, pp. 54–65. Springer, Cham (2016). https://doi.org/10.1007/978-3-319-40247-5_6CrossRefGoogle Scholar
-
17.Seth, D., Chablat, D., Bennis, F., Sakka, S., Jubeau, M., Nordez, A.: Validation of a new dynamic muscle fatigue model and DMET analysis. Int. J. Virtual Real. 2016(16), 2016 (2016)Google Scholar
-
18.Talaty, M., Esquenazi, A., Briceno, J.E.: Differentiating ability in users of the ReWalk(TM) powered exoskeleton: an analysis of walking kinematics. In: Proceedings of the IEEE International Conference on Rehabilitation Robotics (ICORR), Seattle, USA, pp. 1–5 (2013). https://doi.org/10.1109/icorr.2013.6650469
-
19.Aoustin, Y.: Walking gait of a biped with a wearable walking assist device. Int. J. of Humanoid Robotics 12(2), 1 550 018-1–11 550 018-20 (2015). https://doi.org/10.1142/s0219843615500188CrossRefGoogle Scholar
-
20.Ktistakis, I.P., Bourbakis, N.G.: A survey on robotic wheelchairs mounted with robotic arms. In: National Aerospace and Electronics Conference (NAECON), pp. 258–262 (2015)Google Scholar
-
21.Aoustin, Y., Formalskii, A.: Walking of biped with passive exoskeleton: evaluation of energy consumption. Multibody Syst. Dyn. 43, 71–96 (2017). https://doi.org/10.1007/s11044-017-9602-7MathSciNetCrossRefzbMATHGoogle Scholar
-
22.Park, W., Jeong, W., Kwon, G., Kim, Y.H., Kim, L.: A rehabilitation device to improve the hand grasp function of stroke patients using a patient-driven approach. In: IEEE International Conference on Rehabilitation Robotics, Seattle Washington, USA (2013)Google Scholar
-
23.Akhmadeev, K., Rampone, E., Yu, T., Aoustin, Y., Le Carpentier, E.: A testing system for a real-time gesture classification using surface EMG. In: Proceedings of the 20th IFAC World Congress, Toulouse France (2017)Google Scholar
-
24.Schwartz, C., Lempereur, M., Burdin, V., Jacq, J.J., Rémy-Néris, O.: Shoulder motion analysis using simultaneous skin shape registration. In: Proceedings of the 29th Annual International Conference of the IEEE EMBS, Lyon, France (2007)Google Scholar
-
25.National Stroke Association Brochure (2017)Google Scholar
-
26.Nef, T., Guidali, M., Riener, R.: ARMin III – arm therapy exoskeleton with an ergonomic shoulder actuation. Appl. Bionics Biomech. 6(2), 127–142 (2009)CrossRefGoogle Scholar
-
27.Krebs, H.I., Hogan, N., Volpe, B.T., Aisen, M.L., Edelstein, L., Diels, C.: Overview of clinical trials with MITMANUS: a robot-aided neuro-rehabilitation facility. Technol. Health Care 7(6), 419–423 (1999)Google Scholar
-
28.Ali, H.: Bionic exoskeleton: history, development and the future. IOSR J. Mechan. Civ. Eng. 58–62 (2014)Google Scholar
-
29.Banala, S.K., Agrawal, S.K., Scholz, J.P.: Active leg exoskeleton (ALEX) for gait rehabilitation of motor-impaired patients. In: IEEE 2007 Rehabilitation Robotics, pp. 401–407 (2007)Google Scholar
-
30.Fitle, K.D., Pehlivan, A.U., O’Malley, M.K.: A robotic exoskeleton for re-habilitation and assessment of the upper limb following incomplete spinal cord in-jury. In: 2015 IEEE International Conference on Robotics and Automation (ICRA), pp. 4960–4966 (2015)Google Scholar
-
31.
-
32.
-
33.Plagenhoef, S., et al.: Anatomical data for analyzing human motion (1983)Google Scholar
Posts Tagged Exosuit
[ARTICLE] An Overview of Artificial Intelligence-based Soft Upper Limb Exoskeleton for Rehabilitation: A Descriptive Review – Full Text PDF
Posted by Kostas Pantremenos in Artificial intelligence on January 18, 2023
Abstract: The upper limb robotic exoskeleton is an electromechanical device which
use to recover a patient’s motor dysfunction in the rehabilitation field. It can provide
repetitive, comprehensive, focused, positive, and precise training to regain the joints
and muscles’ capability. It has been shown that existing robotic exoskeletons are
generally used rigid motors and mechanical structures. Soft robotic devices can be a
correct substitute for rigid ones. Soft exosuits are flexible, portable, comfortable,
user-friendly, low-cost, and travel-friendly. Somehow, they need expertise or
therapist to assist those devices. Also, they cannot be adaptable to different patients
with non-identical physical parameters and various rehabilitation needs. For that
reason, nowadays we need intelligent exoskeletons during rehabilitation which have
to learn from patient’s previous data and act according to it with patient’s intention.
There also has a big gap between theoretical and practical applications for using
those exoskeletons. Most of the intelligent exoskeletons are prototype in manner. To
solve this problem, the robotic exoskeleton should be made both criteria as
ergonomic and portable. The exoskeletons have to the power of decision-making to
avoid the presence of expertise. In this growing field, the present trend is to make
the exoskeleton intelligent and make it more reliable to use in clinical practice.
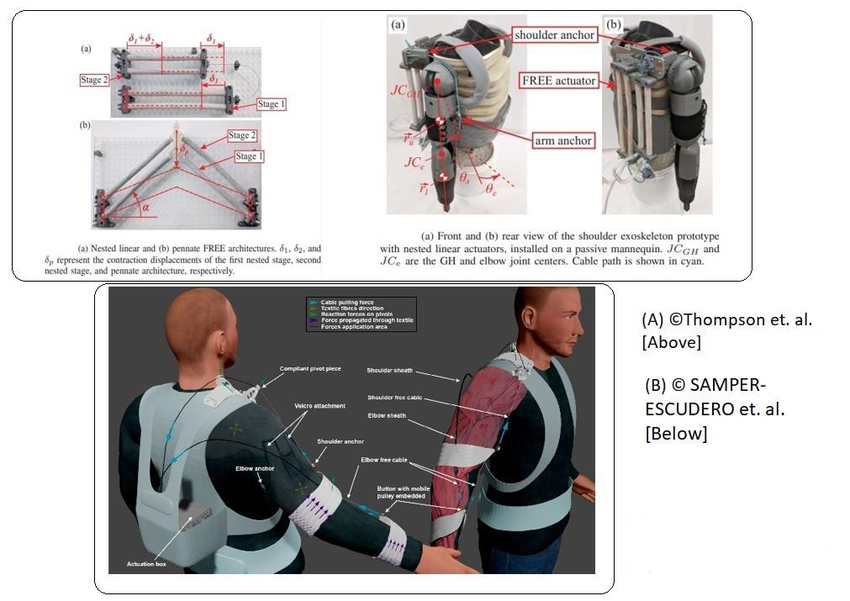
[Abstract] Soft, lightweight wearable robots to support the upper limb in activities of daily living: a feasibility study on chronic stroke patients
Posted by Kostas Pantremenos in Paretic Hand, Rehabilitation robotics on May 22, 2022
Abstract
Stroke can be a devastating condition that impairs the upper limb and reduces mobility. Wearable robots can aid impaired users by supporting performance of Activities of Daily Living (ADLs). In the past decade, soft devices have become popular due to their inherent malleable and low-weight properties that makes them generally safer and more ergonomic. In this study, we present an improved version of our previously developed gravity-compensating upper limb exosuit and introduce a novel hand exoskeleton. The latter uses 3D-printed structures that are attached to the back of the fingers which prevent undesired hyperextension of joints. We explored the feasibility of using this integrated system in a sample of 10 chronic stroke patients who performed 10 ADLs.We observed a significant reduction of 30.3 ± 3.5% (mean ± standard error), 31.2 ± 3.2% and 14.0 ± 5.1% in the mean muscular activity of the Biceps Brachii (BB), Anterior Deltoid (AD) and Extensor Digitorum Communis muscles, respectively. Additionally, we observed a reduction of 14.0 ± 11.5%, 14.7 ± 6.9% and 12.8 ± 4.4% in the coactivation of the pairs of muscles BB and Triceps Brachii (TB), BB and AD, and TB and Pectoralis Major (PM), respectively, typically associated to pathological muscular synergies, without significant degradation of healthy muscular coactivation. There was also a significant increase of elbow flexion angle (12.1±1.5°). These results further cement the potential of using lightweight wearable devices to assist impaired users.
[Abstract] Individualization of exosuit assistance based on measured muscle dynamics during versatile walking
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, Rehabilitation robotics on November 22, 2021

Abstract
Variability in human walking depends on individual physiology, environment, and walking task. Consequently, in the field of wearable robotics, there is a clear need for customizing assistance to the user and task. Here, we developed a muscle-based assistance (MBA) strategy wherein exosuit assistance was derived from direct measurements of individuals’ muscle dynamics during specific tasks. We recorded individuals’ soleus muscle dynamics using ultrasonographic imaging during multiple walking speeds and inclines. From these prerecorded images, we estimated the force produced by the soleus through inefficient concentric contraction and designed the exosuit assistance profile to be proportional to that estimated force. We evaluated this approach with a bilateral ankle exosuit at each measured walking task. Compared with not wearing a device, the MBA ankle exosuit significantly reduced metabolic demand by an average of 15.9, 9.7, and 8.9% for level walking at 1.25, 1.5, and 1.75 meters second−1, respectively, and 7.8% at 1.25 meters second−1 at 5.71° incline while applying lower assistance levels than in existing literature. In an additional study (n = 2), we showed for multiple walking tasks that the MBA profile outperforms other bioinspired strategies and the average profile from a previous optimization study. Last, we show the feasibility of online assistance generation in a mobile version for overground outdoor walking. This muscle-based approach enables relatively rapid (~10 seconds) generation of individualized low-force assistance profiles that provide metabolic benefit. This approach may help support the adoption of wearable robotics in real-world, dynamic locomotor tasks by enabling comfortable, tailored, and adaptive assistance.
[WEB] Personalized Exosuit Uses Ultrasound to Adapt to User’s Needs – Video
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, Rehabilitation robotics on November 16, 2021

At Harvard University a team of scientists and engineers developed an exosuit that uses ultrasound to measure muscle activity. The capability allows for rapid calibration of the suit for users’ needs. The soft wearable device continuously assists when walking or running, reducing the energy required to perform these tasks, which could be very useful for patients with neurological issues or muscular dystrophy. By directly measuring muscle dynamics, the suit provides activity- and user-specific assistance, bringing such wearable technologies a step closer to fruition.
Wearable ‘exosuits’ have significant potential in assisting those with mobility issues by providing supplemental power when a wearer is walking or running. Medgadget has featured these technologies in the past. However, at present, it is not straightforward to calibrate an exosuit to optimize for a particular user or for different activities a single user might take part in. For instance, the mechanics of running and walking are quite different and uneven terrain can drastically change the requirements of the exosuit.
Currently, it is typical that hours of fine tuning are required before an exosuit is ready for the needs of a particular user performing a specific task. This is laborious and impractical, and a barrier to the wider adoption of such technology. In response to this, the Harvard researchers designed an exosuit that can directly measure the muscle activity of its wearer as they perform a specific task and then enable rapid customization of the suit so that it fulfills the needs of the user.
“We used ultrasound to look under the skin and directly measured what the user’s muscles were doing during several walking tasks,” said Richard Nuckols, one of the developers of the new exosuit technology, in a Harvard press release. “Our muscles and tendons have compliance which means there is not necessarily a direct mapping between the movement of the limbs and that of the underlying muscles driving their motion.”

The new system consists of a portable ultrasound system that is strapped to the leg of a user, which images the underlying muscle activity. “From these pre-recorded images, we estimated the assistive force to be applied in parallel with the calf muscles to offset the additional work they need to perform during the push off phase of the walking cycle,” said Krithika Swaminathan, another researcher involved in the study.
After just a couple of seconds of walking, the suit can accurately assess the muscle activity. “By measuring the muscle directly, we can work more intuitively with the person using the exosuit,” said Sangjun Lee, another researcher involved creating the device. “With this approach, the exosuit isn’t overpowering the wearer, it’s working cooperatively with them.”
See a video about the technology below.
Study in Science Robotics: Individualization of exosuit assistance based on measured muscle dynamics during versatile walking
Via: Harvard
Conn Hastings received a PhD from the Royal College of Surgeons in Ireland for his work in drug delivery, investigating the potential of injectable hydrogels to deliver cells, drugs and nanoparticles in the treatment of cancer and cardiovascular diseases. After achieving his PhD and completing a year of postdoctoral research, Conn pursued a career in academic publishing, before becoming a full-time science writer and editor, combining his experience within the biomedical sciences with his passion for written communication.
[ARTICLE] Activity-based training with the Myosuit: a safety and feasibility study across diverse gait disorders – Full Text
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, REHABILITATION, Rehabilitation robotics on November 30, 2020
Abstract
Background
Physical activity is a recommended part of treatment for numerous neurological and neuromuscular disorders. Yet, many individuals with limited mobility are not able to meet the recommended activity levels. Lightweight, wearable robots like the Myosuit promise to facilitate functional ambulation and thereby physical activity. However, there is limited evidence of the safety and feasibility of training with such devices.
Methods
Twelve participants with diverse motor disorders and the ability to walk for at least 10 m were enrolled in this uncontrolled case series study. The study protocol included five training sessions with a net training time of 45 min each. Primary outcomes were the feasibility of engaging in training with the Myosuit, the occurrence of adverse events, and participant retention. As secondary outcomes, we analyzed the walking speed using the 10-m Walk Test (10MWT) and for three participants, walking endurance using the 2-min Walk Tests.
Results
Eight out of 12 participants completed the entire study protocol. Three participants withdrew from the study or were excluded for reasons unrelated to the study. One participant withdrew because of an unsafe feeling when walking with the Myosuit. No adverse events occurred during the study period for any of the participants and all scheduled trainings were completed. For five out of the eight participants that completed the full study, the walking speed when using the Myosuit was higher than to their baseline walking speed.
Conclusions
Activity-based training with the Myosuit appears to be safe, feasible, and well-tolerated by individuals with diverse motor disorders.
Background
Physical inactivity has been identified as the fourth leading risk factor for global mortality, only surpassed by hypertension, tobacco use, and hyperglycemia. To contain the risks associated with physical inactivity, the World Health Organization recommends that all adults engage in moderate intensity physical activity for at least 150 min each week [1].
Physical activity is also a recommended part of treatment for stroke patients [2], and for patients with incomplete spinal cord injury (SCI) [3], inherited neuropathies such Charcot–Marie–Tooth disease [4], heart failure [5], or chronic obstructive pulmonary disease [6]. These wide-ranging recommendations reflect the consistent association between increased physical activity and improved health-related quality of life (e.g. [7,8,9].).
In spite of the evident health benefits of physical activity, a large proportion of elderly individuals and individuals with limited mobility do not meet the recommended dose of physical activity in their daily lives [10]. In many of these cases, neurological, neuromuscular, or cardiovascular deficits prevent individuals from reaching moderate intensity levels during exercise. In some cases, they prohibit any voluntary exercise altogether.
To address this problem, various technological solutions like full-leg, rigid exoskeletons have been developed to assist overground mobility (e.g. [11,12,13,14].). The safety and feasibility of gait training with mobile exoskeletons has been evaluated in several longitudinal training studies for individuals with spinal cord injury [15,16,17] and hemiparesis following stroke [18, 19]. Rigid exoskeletons largely substitute the ambulatory function of severely affected or completely paralyzed individuals and enable them to walk. Electric motors are used to provide large assistive torques to the users’ leg joints via rigid linkages. This allows exoskeletons to support the majority of the users’ weight and advance the users’ legs without a major voluntary contribution from the leg muscles.
The typically large masses of mobile rigid exoskeletons increase limb inertia and thereby hinder walking at higher speeds. The highest walking speed achieved in previous training studies [15,16,17,18,19] was 0.67 m/s, while most speeds were as low as 0.1 m/s to 0.4 m/s. This is well below the speeds required to support individuals with residual mobility during moderate intensity exercise.
To assist this more capable section of the population, more lightweight wearable robots (also known as “exosuits”, “exomuscles” or “dermoskeletons”) have been proposed [20,21,22,23,24]. Unlike exoskeletons that act on all leg joints, these devices allow for—and require—the active participation of the user, and can (partially) assist walking over a larger range of speeds [20, 25]. Thereby, such wearable robots can provide assistance as needed for functional ambulation [25] while simultaneously modulating the cardiovascular load of their users according to exercise recommendations. For example, a soft robotic exosuit unilaterally acting on one ankle joint was shown to reduce the energy expenditure and interlimb asymmetry of individuals with hemiparesis following a stroke during walking at 0.5 to 1.3 m/s [20]. In previous work from our group, we demonstrated that a soft wearable robot actively supporting hip and knee extension, the Myosuit, enabled an individual with incomplete SCI to walk substantially faster when assisted [25]. More recently, we showed that this functional improvement also translates to an increase in exercise intensity and a momentary reduction of the energetic cost of transport [26]. In larger longitudinal studies, training with wearable robots acting on the hip joint was shown to result in an intrinsic reduction of the cost of transport for elderly individuals [23] and individuals following stroke [24].
Further work [27,28,29] has primarily focused on the functional effects of robotic movement assistance. A lightweight wearable robot that assists knee flexion and extension reduced momentary movement performance, but elicited larger intrinsic improvements after 2 weeks of exercise training than when training without the device in users with multiple sclerosis [27]. In larger randomized controlled trials with individuals post-stroke, training with a robotic knee brace was shown to result in only modest functional benefits that were comparable to the control group [28], while training with a hip exoskeleton resulted in more pronounced functional benefits [29].
While it is hard to synthesize common trends out of the limited studies available, it appears that the most pronounced improvements were so far achieved with devices that targeted a very specific motor deficit (e.g. ankle assistance [20] or hip assistance [24, 29] improved hemiparetic gait for individuals after stroke). Other findings with devices that bear promise to work for more diverse gait disorders were based on single-participant observations [22, 25, 26], and it remains unclear to what extend these results generalize to larger populations.
There is limited evidence of how a single wearable robot could effectively assist individuals with diverse neuromuscular and neurological gait disorders during exercise training. Such a wider applicability would be highly desirable considering that in everyday clinical life, patients present with a wide array of different conditions and functional deficits [30].
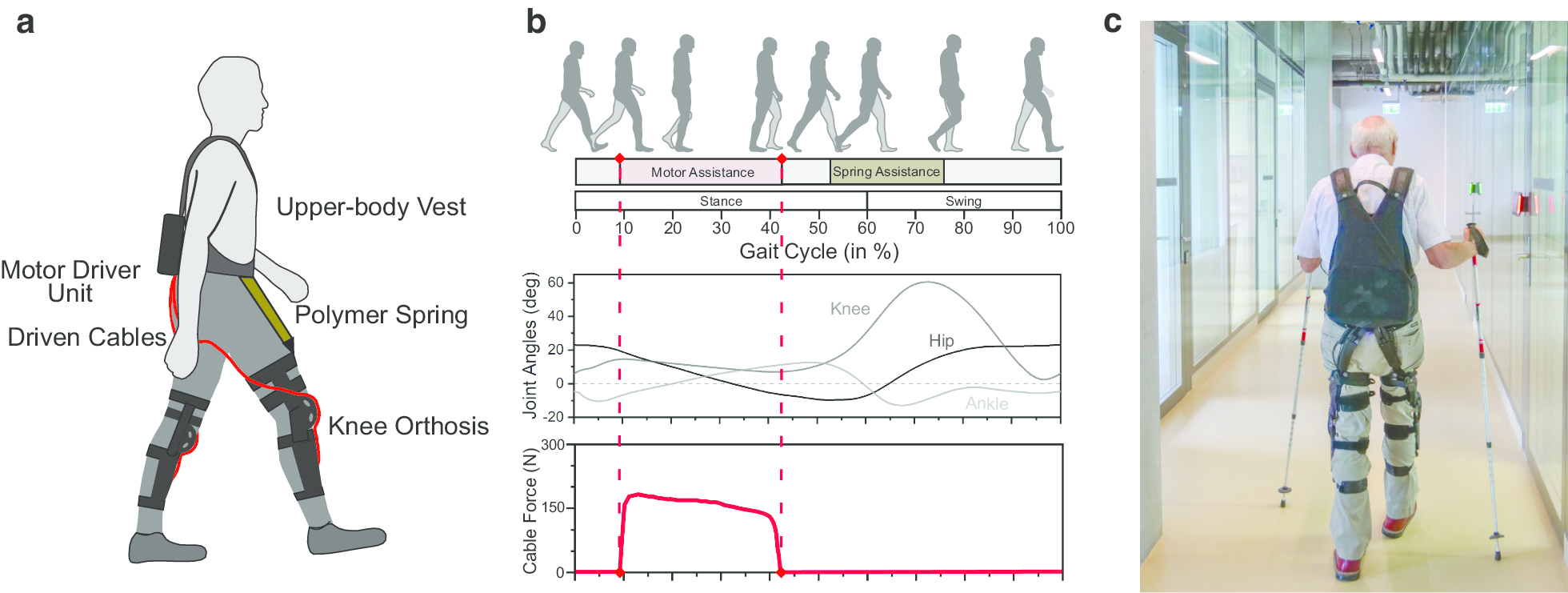
We believe that the Myosuit is a promising device to assist the training of individuals with diverse gait disorders. The Myosuit assists walking in essential functions [31] by supporting the user’s bodyweight from weight acceptance through mid-stance and assisting swing initiation from terminal stance into early swing (see Fig. 1b). By working in parallel with the user’s hip and knee extensor muscles and exploiting natural synergies [32], the Myosuit supports the muscles with the largest contribution to bodyweight support in that phase of walking [33]. Training with the Myosuit can extend beyond step training and into areas of balance, strength, and coordination.
[ARTICLE] The ReWalk ReStore™ soft robotic exosuit: a multi-site clinical trial of the safety, reliability, and feasibility of exosuit-augmented post-stroke gait rehabilitation – Full Text
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, REHABILITATION, Rehabilitation robotics on June 18, 2020
Abstract
Background
Atypical walking in the months and years after stroke constrain community reintegration and reduce mobility, health, and quality of life. The ReWalk ReStore™ is a soft robotic exosuit designed to assist the propulsion and ground clearance subtasks of post-stroke walking by actively assisting paretic ankle plantarflexion and dorsiflexion. Previous proof-of-concept evaluations of the technology demonstrated improved gait mechanics and energetics and faster and farther walking in users with post-stroke hemiparesis. We sought to determine the safety, reliability, and feasibility of using the ReStore™ during post-stroke rehabilitation.
Methods
A multi-site clinical trial (NCT03499210) was conducted in preparation for an application to the United States Food and Drug Administration (FDA). The study included 44 users with post-stroke hemiparesis who completed up to 5 days of training with the ReStore™ on the treadmill and over ground. In addition to primary and secondary endpoints of safety and device reliability across all training activities, an exploratory evaluation of the effect of multiple exposures to using the device on users’ maximum walking speeds with and without the device was conducted prior to and following the five training visits.
Results
All 44 study participants completed safety and reliability evaluations. Thirty-six study participants completed all five training days. No device-related falls or serious adverse events were reported. A low rate of device malfunctions was reported by clinician-operators. Regardless of their reliance on ancillary assistive devices, after only 5 days of walking practice with the device, study participants increased both their device-assisted (Δ: 0.10 ± 0.03 m/s) and unassisted (Δ: 0.07 ± 0.03 m/s) maximum walking speeds (P’s < 0.05).
Conclusions
When used under the direction of a licensed physical therapist, the ReStore™ soft exosuit is safe and reliable for use during post-stroke gait rehabilitation to provide targeted assistance of both paretic ankle plantarflexion and dorsiflexion during treadmill and overground walking.
Introduction
Bipedal locomotion is characterized by alternating periods of single and double limb support, with ground clearance by the swing limb and propulsion by the trailing stance limb serving as crucial walking subtasks [1, 2]. Healthy individuals are able to generate an ankle dorsiflexion moment during each limb’s swing phase to lift the foot and facilitate ground clearance. They are also able to generate an ankle plantarflexion moment during each limb’s late stance phase to produce the propulsive force required to advance the limb and body [3]. In contrast, post-stroke hemiparesis results in impaired paretic dorsiflexion and plantarflexion that, in turn, hinders ground clearance and propulsion [4,5,6,7,8] and, ultimately, necessitates compensatory walking strategies [9, 10] that make walking more effortful and unstable [11,12,13,14].
The ReWalk ReStore™ is a soft robotic exosuit designed to augment the paretic ankle’s ability to produce both dorsiflexor and plantarflexor moments during walking. In early proof-of-concept studies conducted with a research version of the device [15, 16], exosuits were shown to facilitate immediate increases in swing phase paretic ankle dorsiflexion by an average 5 degrees [17], the propulsion force generated by the paretic limb by an average 10% [17], and the positive center of mass (COM) power generated by the paretic limb during late stance phase by an average 22% [18]. Together, these improvements in paretic limb function resulted in reduced propulsion asymmetry by 20% [17] and the asymmetry in positive COM power generated during late stance phase by 39% [18]. Also observed were immediate reductions in hip hiking and circumduction compensations of over 20% [9], reductions in the energy cost of walking by an average 10% [17, 18], faster overground walking speeds by a median 0.14 m/s, and farther walking distances during the 6-min walk test by a median 32m [19].
Building on this foundational biomechanical, physiological, and clinical research, the objective of this multi-site clinical trial was to evaluate safety, feasibility, and reliability of using exosuits during post-stroke rehabilitation in preparation for a commercial clinical application to the United States Food and Drug Administration (FDA). In contrast to previous laboratory-based research that studied the immediate effects of exosuit prototypes on clinical, biomechanical, and physiological outcomes, this translational research sought to determine the safety of clinicians and patients with post-stroke hemiparesis using the commercially-adapted ReStore™ in clinical settings, the feasibility of clinician operators applying the ReStore™ during both treadmill and over ground gait training activities, and the reliability of the technology across multiple training visits. In addition to outcomes of safety, feasibility, and device reliability, an exploratory evaluation of the impact that multiple training visits with the device have on users’ maximum walking speeds, both with and without the device, was also included.
Methods
The ReStore™ is indicated for use by individuals with post-stroke hemiparesis undergoing stroke rehabilitation under the supervision of a licensed physical therapist. To assess the safety, device reliability, and clinical feasibility of using the ReStore™ during post-stroke gait rehabilitation, a multi-site trial was conducted. The trial included five clinical sites and 44 users with post-stroke hemiparesis. The study was approved by the Institutional Review Boards of Boston University, Spaulding Rehabilitation Hospital, The Shirley Ryan AbilityLab, TIRR Memorial Hermann Hospital, Kessler Rehabilitation Hospital, and Moss Rehabilitation Hospital. Written informed consent was secured for all participants.
Study inclusion and exclusion criteria
Study participant eligibility requirements consisted of: (i) one-sided ischemic or hemorrhagic stroke, (ii) > 2 weeks post-stroke, (iii) age > 18 years, (iv) height between 4′8″ and 6′7″, (v) weight < 264lbs, (vi) medical clearance, (vii) ability to ambulate at least 5 ft without an AFO and with no more than minimal contact assistance, (viii) ability to follow a 3-step command, (ix) ability to fit suit components, (x) no greater than 5 degrees of ankle plantar flexion contracture, and (xi) Modified Ashworth Scale for tone at 3 or less for ankle dorsiflexor and plantarflexor muscles. Exclusion criteria included: (i) severe aphasia limiting ability to express needs or discomfort verbally or non-verbally, (ii) serious co-morbidities that interfere with ability to participate, (iii) significant Peripheral Artery Disease, (iv) colostomy bag, (v) current pregnancy, (vi) uncontrolled hypertension, (vii) participation in any other clinical trial, (viii) open wounds or broken skin at device locations requiring medical management, (ix) urethane allergies, (x) and current DVT.
Study overview
After screening and enrollment, study participants completed up to two walking evaluations and five device exposure visits. Each exposure visit consisted of up to 20 min of overground walking practice and 20 min of treadmill walking practice while receiving assistance from the device. The visit schedule consisted of a minimum of two visits per week, with the expectation of no more than 4 weeks between the pretraining and posttraining evaluations. Actual activities and durations were dependent on each study participant’s abilities as determined by the treating physical therapist as per their usual practices. The target level for plantarflexion assistance during all active walking with the ReStore™ was 25% of the user’s bodyweight [17, 19]. The target level for dorsiflexion assistance was the minimum needed for adequate ground clearance and heel strike, as determined visually by the physical therapist.
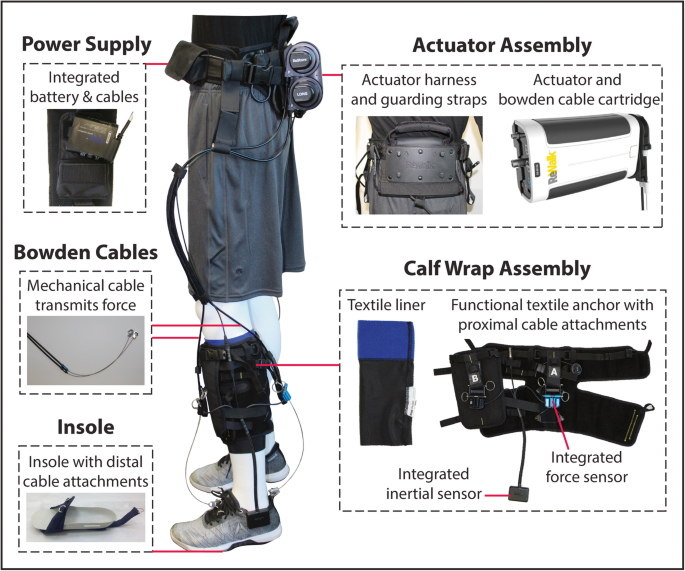
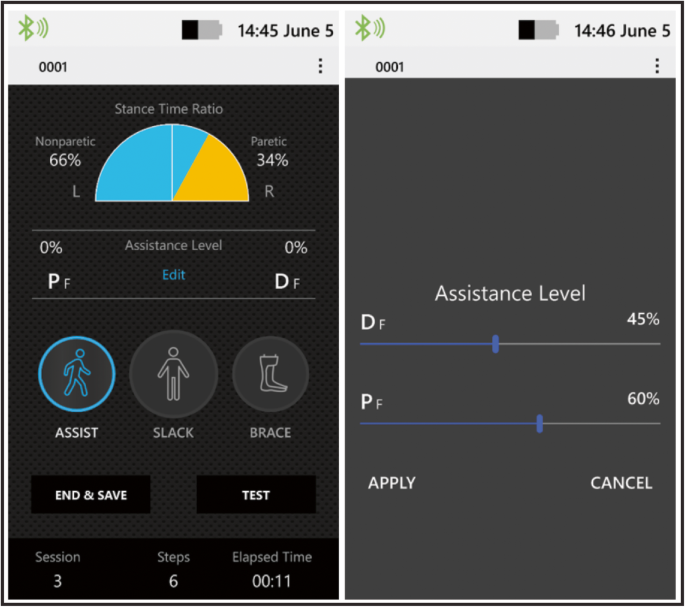
Device overview
The exosuit consists of motors worn at the waist that generate mechanical forces that are transmitted by cables to attachment points located proximally on a functional textile worn around the calf and distally on a shoe insole (Fig. 1). The overall weight of the exosuit is approximately 5kgs, with the vast majority of the weight located proximally in the actuation pack worn at the waist. Each functional textile contains a detachable liner that can be washed. For users who require medio-lateral ankle support in addition to ankle plantarflexion and dorsiflexion assistance, an optional textile component that prevents ankle inversion without restricting dorsiflexion and plantarflexion can also be used. Inertial sensors that attach to a patient’s shoes measure gait events and automate the independent timing of the active ankle plantarflexion and dorsiflexion assistance provided by the ReStore™ as previously described [16]. Load cell sensors located at the end of each cable are used to monitor the interaction between user and exosuit and ensure that the target level of assistance is achieved [16, 17]. A hand-held device with a graphical interface allows clinicians to monitor patients’ performance and select and progress, in real-time, the assistance parameters (Fig. 2).
[…]
Continue …
[Abstract + References] Preliminary Design of Soft Exo-Suit for Arm Rehabilitation – Conference paper
Posted by Kostas Pantremenos in Paretic Hand, Rehabilitation robotics on July 16, 2019
Abstract
Every year, millions of people experience a stroke but only a few of them fully recover. Recovery requires a working staff, which is time consuming and inefficient. Therefore, over the past few years rehabilitation robots like Exoskeletons have been used in the recuperation process for patients. In this paper we have designed an Exosuit which takes into considerations of the rigid Exo-Skeleton and its limitations for patients suffering from loss of function of the arm. This paper concentrates on enabling a stroke affected person to perform flexion-extension at elbow joint. Validation of the developed model on general population is still needed.
References
via Preliminary Design of Soft Exo-Suit for Arm Rehabilitation | SpringerLink
[VIDEO] Watch a robotic exoskeleton help a stroke patient walk – YouTube
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, Video on February 11, 2019
Although it’s a far cry from the exosuits of science fiction, researchers have developed a robotic exoskeleton that can help stroke victims regain use of their legs. Nine out of 10 stroke patients are afflicted with partial paralysis, leaving some with an abnormal gait. The exosuit works by pulling cords attached to a shoe insole, providing torque to the ankle and correcting the abnormal walking motion. With the suit providing assistance to their joints, the stroke victims are able to maintain their balance, and walk similarly to the way they had prior to their paralysis, the team reports today in Science Translational Medicine. The exosuit is an adaptation of a previous design developed for the Defense Advanced Research Projects Agency Warrior Web program, a Department of Defense plan to develop assistive exosuits for military applications. Although similar mechanical devices have been built in the past to assist in gait therapy, these were bulky and had to be kept tethered to a power source. This new suit is light enough that with a decent battery, it could be used to help patients walk over terrain as well, not just on a treadmill. The researchers say that although the technology needs long-term testing, it could start to decrease the time it takes for stroke patients to recover in the near future.
via Watch a robotic exoskeleton help a stroke patient walk | Science | AAAS
[WEB SITE] Study Examines Exoskeleton’s Ability to Improve Walking for Stroke Patients
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, Rehabilitation robotics on August 18, 2017

Conor Walsh and his graduate student, Jaehyun Bae, fine-tune an ankle-assisting exosuit. (Photo courtesy of Rolex Awards/Fred Merz)
A study published recently in Science Translational Medicine suggests that the use of a soft suit exoskeleton system helps aid in the facilitation of walking ability among ambulatory patients following a stroke.
Researchers from Harvard University’s Wyss Institute for Biologically Inspired Engineering, the Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS), and Boston University’s (BU) College of Health & Rehabilitation Sciences: Sargent College developed the lightweight, soft, wearable ankle-assisting exosuit, and they they suggest in the study that it could help reinforce normal gait in people with hemiparesis after stroke.
The study centers on the use of the exosuit among nine participants, each of whom recently experienced a stroke, and examines the immediate improvements in walking capability that could be obtained when wearing the suit, dubbed the Restore system, according to a media release from ReWalk Robotics Ltd.
According to the release, the study concludes that improvements in paretic limb function contributed to a 20 +/- 4% reduction in forward propulsion interlimb asymmetry and a 10 +/- 3% reduction in the energy cost of walking, which is equivalent to a 32+/- 9% reduction in the metabolic burden associated with poststroke walking. Relatively low assistance (~12% of biological torques) delivered with a lightweight and nonrestrictive exosuit was sufficient to facilitate more normal walking in ambulatory individuals after stroke.
“This foundational study shows that soft wearable robots can have significant positive impact on gait functions in patients post-stroke, and it is the result of a translational-focused multidisciplinary team of engineers, designers, biomechanists, physical therapists, and most importantly patients who volunteered for this study and gave valuable feedback that guided our research,” says Wyss Core Faculty member Conor Walsh, who is also the John L. Loeb Associate Professor of Engineering and Applied Sciences at SEAS and the Founder of the Harvard Biodesign Lab, in the release.
ReWalk is working with the Wyss Institute on the development of lightweight designs to complete clinical studies, pursue regulatory approvals, and commercialize the systems on a global scale. The first commercial application will be for stroke survivors, followed by Multiple Sclerosis patients and then additional applications.
“Exoskeletons are now a commercially available, disruptive technology that have changed the lives of many individuals in the paraplegic community,” states ReWalk CEO Larry Jasinski, in the release. “The ongoing research at the Wyss Institute on soft exosuits adds a new dimension to exoskeletons that can potentially meet the needs of individuals that have had a stroke, as well as for those diagnosed with Multiple Sclerosis, Parkinson’s disease or people who have limitations in walking.”
[Source(s): ReWalk Robotics Ltd, PR Newswire, Science Daily]
Source: Study Examines Exoskeleton’s Ability to Improve Walking for Stroke Patients – Rehab Managment
[WEB SITE] Wyss Institute Collaborating with ReWalk Robotics to Develop Soft Exosuit.
Posted by Kostas Pantremenos in Gait Rehabilitation - Foot Drop, Rehabilitation robotics on May 24, 2016

The Wyss Institute for Biologically Inspired Engineering announces a collaboration with ReWalk Robotics Ltd to develop an assistive exosuit for use by stroke and multiple sclerosis patients.
The exosuit in development at Wyss Institute, located at Harvard University, differs from the ReWalk exoskeleton and others for spinal cord injury patients in that, rather than being rigid and used to provide structural support and large assistance for patients with extremely severe movement disabilities, it is lightweight, nonrestrictive, made from soft and wearable materials, and built for those who could move partially on their own, per a media release from Wyss Institute.
The soft exosuit transmits power to key joints of the legs via cable technologies powered with software and mechanics that are similar to the technologies used in the ReWalk system. The cables are connected to fabric-based designs that attach to the legs and foot, explains a media release from ReWalk Robotics.
Initial pilot studies with stroke patients conducted at Wyss Institute, in collaboration with faculty and researchers from Boston University, demonstrate the function of the softsuit exoskeleton technology.
ReWalk’s collaboration with the Wyss Institute will entail the continued development of lightweight designs to complete clinical studies, the pursuit of regulatory approvals, and the commercialization the soft exosuit on a global scale. The first commercial application is expected to be with stroke patients, then with multiple sclerosis patients, and then additional applications, the ReWalk release continues.
“This is a very exciting day for the soft exosuit technology,” said Conor Walsh, PhD, a core faculty member at the Wyss Institute, in the ReWalk release.
“ReWalk brings commercialization expertise and experience in the area of wearable robotics and complements our translation-focused research. Ultimately this agreement paves the way for this technology to make its way to patients,” adds Walsh, also the John L. Loeb Associate Professor of Engineering and Applied Sciences at Harvard John A. Paulson School of Engineering and Applied Sciences, and Founder of the Harvard Biodesign Lab.
“There is a great need in the health care system for lightweight, lower-cost wearable exoskeleton designs to support stroke patients, individuals diagnosed with multiple sclerosis, and senior citizens who require mechanical mobility assistance. This collaboration will help create the next generation of exoskeleton systems, making life-changing technology available to millions of consumers across a host of patient populations,” states Larry Jasinski, CEO of ReWalk, per the ReWalk Release.
[Source(s): Wyss Institute for Biologically Inspired Engineering at Harvard University, ReWalk Robotics Ltd, PR Newswire]
Source: Wyss Institute Collaborating with ReWalk Robotics to Develop Soft Exosuit – Rehab Managment
